1/ Have you ever had a patient with low back pain & degenerative findings on lumbar MR imaging? 🔎👀
Demystifying lumbar stenosis is one of my favorite things to teach medical students & junior residents!
A thread 🧵
Demystifying lumbar stenosis is one of my favorite things to teach medical students & junior residents!
A thread 🧵

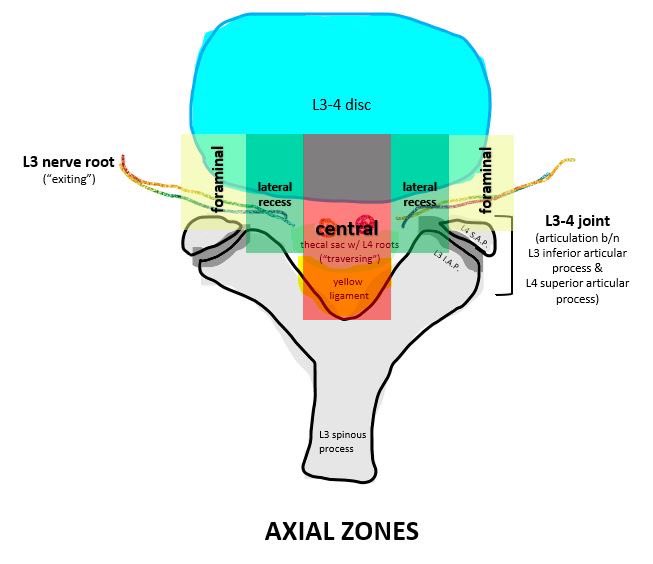
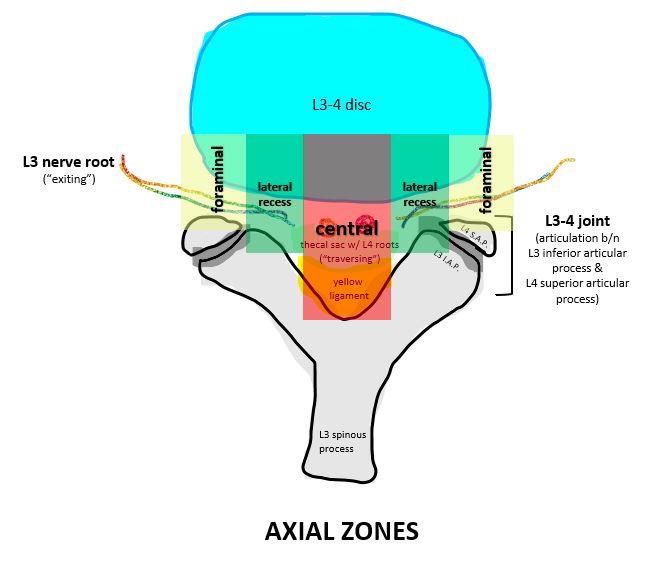
2/ Let’s review the normal anatomy of the L3-4 spinal segment.
🟡 Mid-sagittal: we see the central canal w/ the thecal sac, containing nerve roots distal to the conus.
🟠 Parasagittal: the lumbar nerve roots exit below their respective pedicles via the neural foramina.
🟡 Mid-sagittal: we see the central canal w/ the thecal sac, containing nerve roots distal to the conus.
🟠 Parasagittal: the lumbar nerve roots exit below their respective pedicles via the neural foramina.

3/ Normal anatomy cont’d:
🔵 Posterior view: we see the relationship between “exiting” nerve roots & their respective pedicles, as well as “traversing” nerve roots.
⚪️ Axial (simplified): shows the relationship between the disc, thecal sac, root, and joint.

🔵 Posterior view: we see the relationship between “exiting” nerve roots & their respective pedicles, as well as “traversing” nerve roots.
⚪️ Axial (simplified): shows the relationship between the disc, thecal sac, root, and joint.


4/ “Lumbar stenosis” refers to anything that decreases the area of:
▫️central canal (thecal sac)
▫️lateral recess
▫️neural foramen
Correspondingly, we classify pathologies anatomically as causing “central,” “lateral recess,” or “foraminal” stenosis (color-coded below).
▫️central canal (thecal sac)
▫️lateral recess
▫️neural foramen
Correspondingly, we classify pathologies anatomically as causing “central,” “lateral recess,” or “foraminal” stenosis (color-coded below).
5/ Central stenosis 🟰 compression of the thecal sac by any central pathology (central disc herniation, yellow ligament hypertrophy, epidural lipomatosis, &c).
Primary symptoms:
🔻neurogenic pseudoclaudication
🔻traversing (L4) nerve root radicular pain/numbness/or weakness

Primary symptoms:
🔻neurogenic pseudoclaudication
🔻traversing (L4) nerve root radicular pain/numbness/or weakness

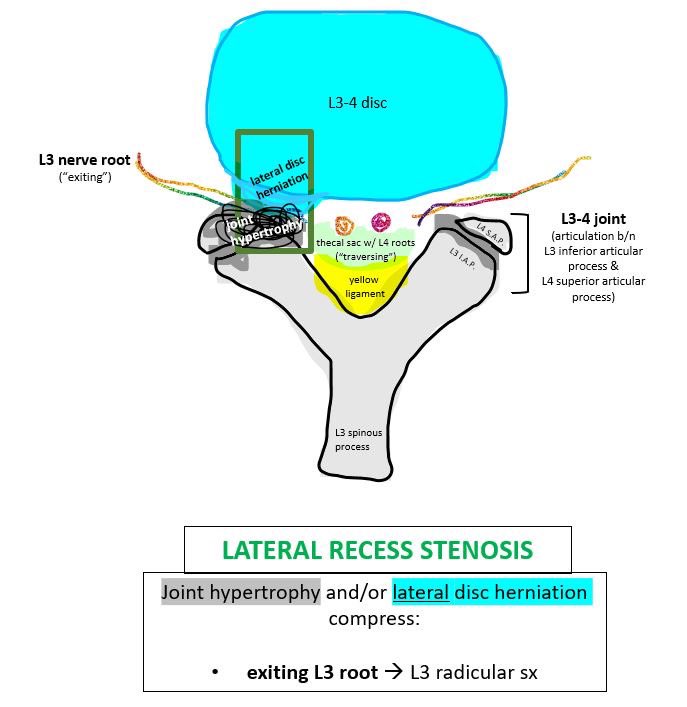
6/ Lateral recess stenosis 🟰 compression in the area bound by the pedicle, vertebral body, & superior articular process…basically the area containing the first part of the exiting root (L3).
Most common symptoms:
🔻exiting (L3) nerve root radicular pain/numbness/or weakness
Most common symptoms:
🔻exiting (L3) nerve root radicular pain/numbness/or weakness
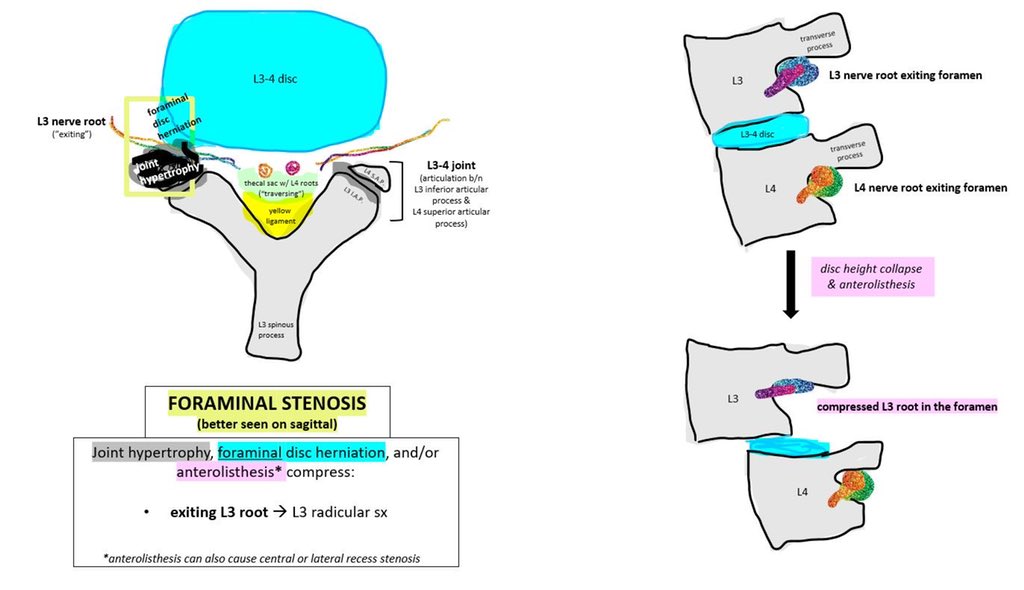
7/ Foraminal stenosis = compression of the exiting nerve root in the foramen, distal to the lateral recess. Common causes include lateral disc herniation, joint hypertrophy, spondylolisthesis, &c.
Main symptoms:
🔻exiting (L3) nerve root radicular pain/numbness/or weakness
Main symptoms:
🔻exiting (L3) nerve root radicular pain/numbness/or weakness
8/ SUMMARY: Lumbar stenosis has many causes & is classified anatomically. Each classification has corresponding implications for symptom localization & treatment!
Disclaimer: content was simplified for purposes of conceptualization.
Any comments or extra info welcomed :)

Disclaimer: content was simplified for purposes of conceptualization.
Any comments or extra info welcomed :)


🙏 You can find my thread on cauda equina syndrome here:
https://twitter.com/k_scheitler/status/1524981647397031962
• • •
Missing some Tweet in this thread? You can try to
force a refresh