PGY-7 #Neurosurgery Resident & #PhD Candidate @MayoClinic | addiction neurobiology, psychiatric #DBS | erstwhile pianist with Liszt lineage | views mine 🪐📚
How to get URL link on X (Twitter) App




 Intraoperative head stabilization is often performed by pinning. Careful & thoughtful consideration is required to
Intraoperative head stabilization is often performed by pinning. Careful & thoughtful consideration is required to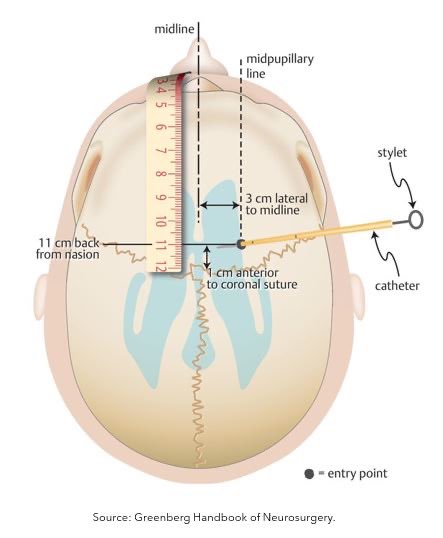
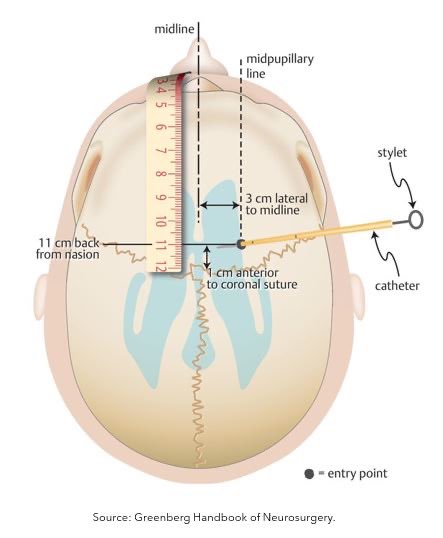 First, let's review how EVDs work. An EVD is a temporary catheter placed in the ventricle at the foramen of Monro that can (1) measure ICP & (2) control ICP by draining CSF.
First, let's review how EVDs work. An EVD is a temporary catheter placed in the ventricle at the foramen of Monro that can (1) measure ICP & (2) control ICP by draining CSF.


 2/ Let’s review the normal anatomy of the L3-4 spinal segment.
2/ Let’s review the normal anatomy of the L3-4 spinal segment.