Three #cardiology cases with diagnostic ECGs in our resus room today and some learning points for emergency clinicians
#ecg #ekg
#ecg #ekg
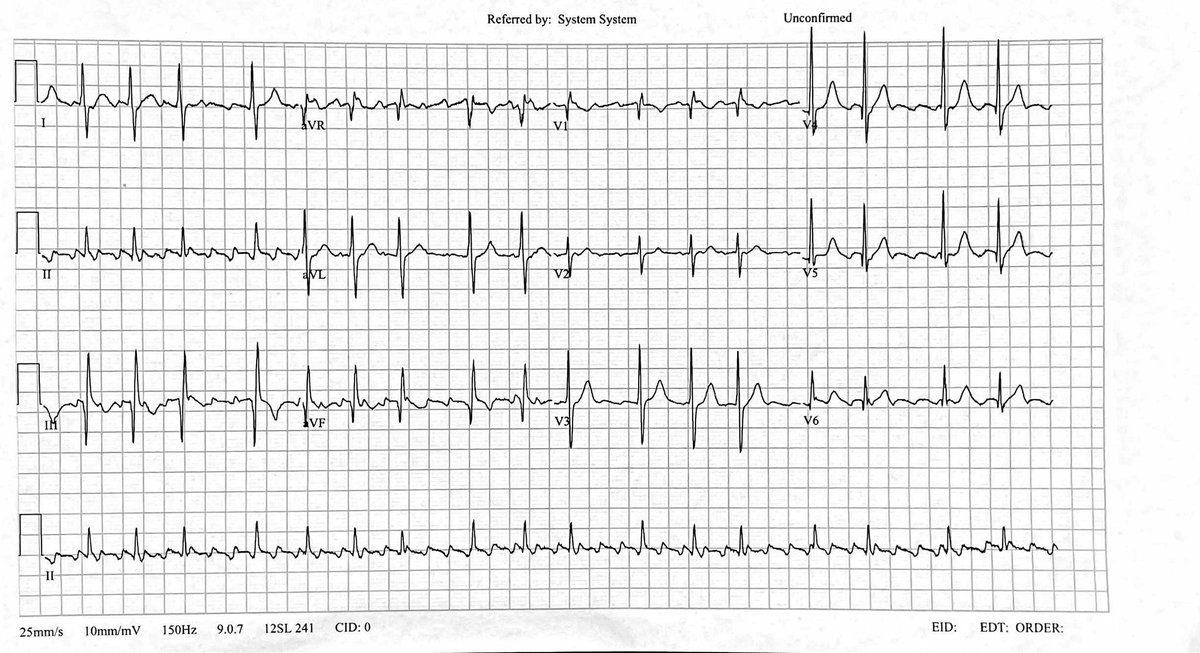
We suspected this was atrial flutter
Rather than subject a patient to the horror of iv adenosine (which only reveals flutter - it can’t convert it), we moved the ECG limb leads around to get a ‘Lewis lead’ which better shows atrial activity
(See litfl.com/lewis-lead-s5-… )
Rather than subject a patient to the horror of iv adenosine (which only reveals flutter - it can’t convert it), we moved the ECG limb leads around to get a ‘Lewis lead’ which better shows atrial activity
(See litfl.com/lewis-lead-s5-… )

After some fentanyl, a checklist, some white medicine and 50 Joules of synchronised electricity, the patient was in sinus rhythm and discharged to follow up with his cardiologist after observation on the ED Short Stay Unit 

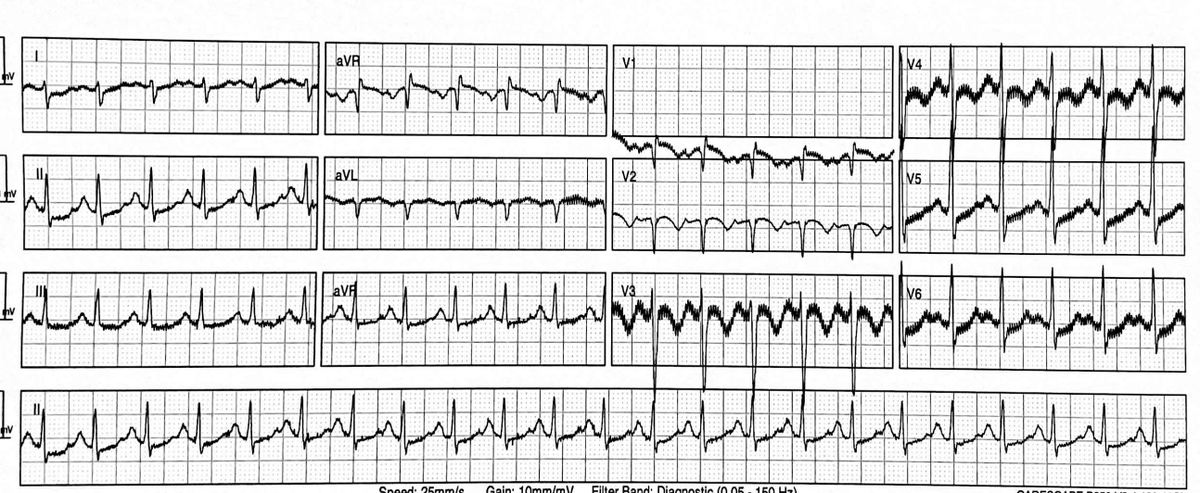
2. A patient who had had a transcatheter aortic valve implantation (TAVI) a few days earlier came in feeling dizzy 

He has complete heart block
Conduction problems are a well recognised complication of TAVI due to the close proximity of the aortic root and conduction tissue
frontiersin.org/articles/10.33…
Conduction problems are a well recognised complication of TAVI due to the close proximity of the aortic root and conduction tissue
frontiersin.org/articles/10.33…

He was normotensive and mentating normally with good skin perfusion and a normal lactate
He did not require intervention in the emergency department and was admitted for pacemaker insertion
He did not require intervention in the emergency department and was admitted for pacemaker insertion
A diagnosis of anterolateral STEMI was made. Cath lab was activated and he was given fentanyl, aspirin, ticagrelor and heparin
The on call interventional cardiologist was still on his way in when other cath lab staff were ready
The on call interventional cardiologist was still on his way in when other cath lab staff were ready
Normally the patient should stay in ED until the cardiologist is ready but we suggested bringing him up anyway to reduce delays and reassured the cath lab nurses we would stay with him until the cardiologist arrived
This enabled the patient to have wrist and groin prepped and draped and was ready for intervention as soon as the cardiologist arrived (ED registrar and cath lab nurse shown in image) 

Summary from today’s cardiology patients in the ED:
1. Lewis lead unveils atrial activity that’s difficult to identify on standard ECG
2. Conduction problems can occur after TAVI
3. EM & Cardiology can work together to devise local solutions to minimise reperfusion delays
1. Lewis lead unveils atrial activity that’s difficult to identify on standard ECG
2. Conduction problems can occur after TAVI
3. EM & Cardiology can work together to devise local solutions to minimise reperfusion delays
• • •
Missing some Tweet in this thread? You can try to
force a refresh