Trying #EECP at @FlowTherapyEECP today for my #LongCovid
It’s intense but cool. Will try a full course after the holidays.
More in thread below… 1/
It’s intense but cool. Will try a full course after the holidays.
More in thread below… 1/

2/ What is #EECP?
Enhanced External Counterpulsation (EECP) is used for non-invasive treatment of heart conditions like angina.
ncbi.nlm.nih.gov/pmc/articles/P…
Enhanced External Counterpulsation (EECP) is used for non-invasive treatment of heart conditions like angina.
ncbi.nlm.nih.gov/pmc/articles/P…
3/ What happens when getting #EECP?
During EECP Flow Therapy, patients lie down on a padded table with specialized cuffs (similar to blood pressure cuffs) wrapped around their calves, lower thighs, and hips. They place a 3-lead EKG
During EECP Flow Therapy, patients lie down on a padded table with specialized cuffs (similar to blood pressure cuffs) wrapped around their calves, lower thighs, and hips. They place a 3-lead EKG

4/ When the heart is in diastole (resting phase), these cuffs inflate sequentially from the calves toward the hips. 🫀➡️🦵🏽
This pressure creates blood flow that is similar to exercise–fueling all areas of your cardiovascular system with essential oxygenated blood while you rest.
This pressure creates blood flow that is similar to exercise–fueling all areas of your cardiovascular system with essential oxygenated blood while you rest.
5/ I’m told an hour of EECP pumps the equivalent amount of blood pumped in a half marathon.
(Which I haven’t been able to do in almost 2 years)
(Which I haven’t been able to do in almost 2 years)

6/ MOA?
The sequential cuff inflation of #EECP creates retrograde pressure wave that augments diastolic pressure, increasing coronary perfusion pressure & venous return to the right heart (increasing preload & cardiac output).
⬆️ growth factors & nitrous oxide.
⬇️inflam cytokines
The sequential cuff inflation of #EECP creates retrograde pressure wave that augments diastolic pressure, increasing coronary perfusion pressure & venous return to the right heart (increasing preload & cardiac output).
⬆️ growth factors & nitrous oxide.
⬇️inflam cytokines

7/ Data on #EECP in #LongCovid?
Research was presented at @ACCinTouch on 50 patients.
🚶🏽♀️Functional capacity using the DASI assessment improved by 20 points (range 0-58.2)
🥱Fatigue levels using the PROMIS score decreased by 6 points (Range 4-20)
acc.org/About-ACC/Pres…
Research was presented at @ACCinTouch on 50 patients.
🚶🏽♀️Functional capacity using the DASI assessment improved by 20 points (range 0-58.2)
🥱Fatigue levels using the PROMIS score decreased by 6 points (Range 4-20)
acc.org/About-ACC/Pres…
8/
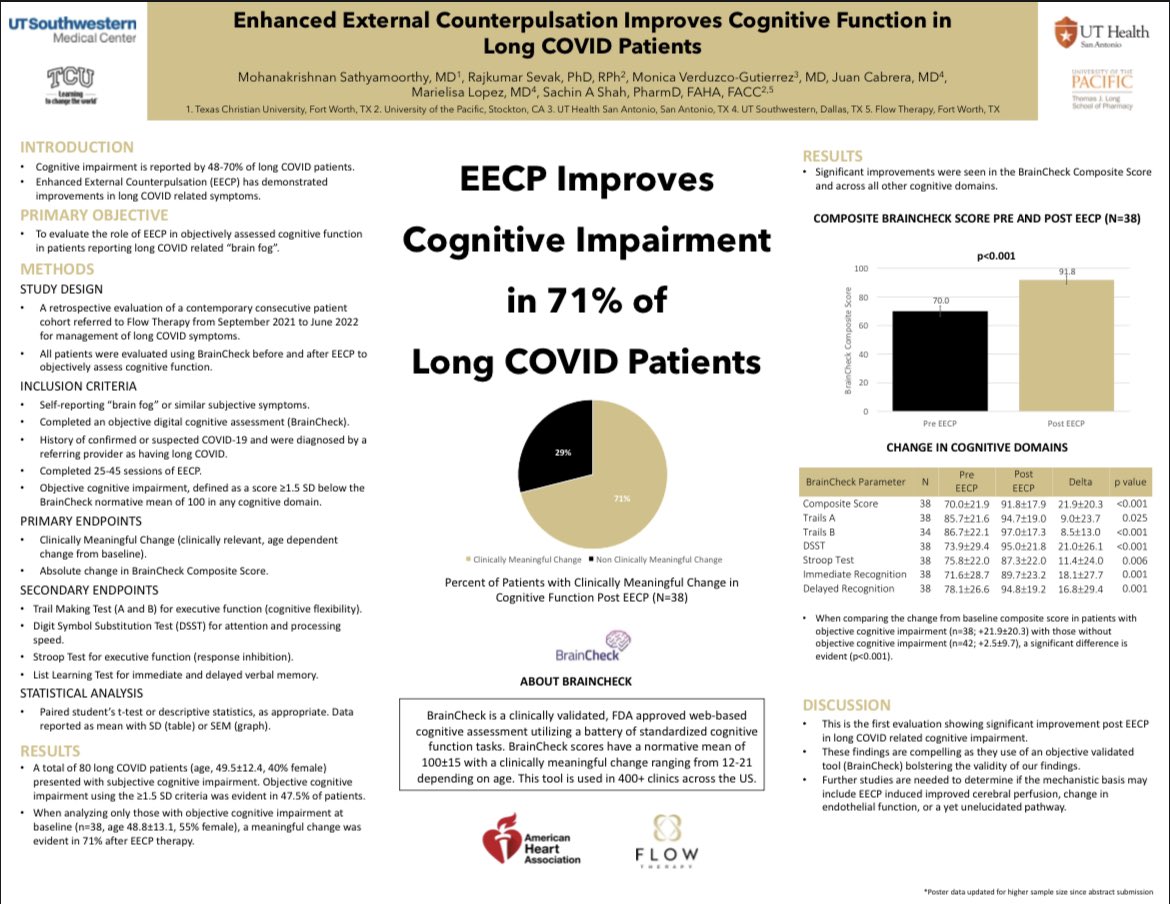
2 other posters presented at AHA in November…
🧠Including how #EECP helps in cognitive impairment in #LongCovid.
Knowing #LongCovid is endothelial dysfunction & immunothrombosis, of course @FlowTherapyEECP has been extremely impactful.
2 other posters presented at AHA in November…
🧠Including how #EECP helps in cognitive impairment in #LongCovid.
Knowing #LongCovid is endothelial dysfunction & immunothrombosis, of course @FlowTherapyEECP has been extremely impactful.
• • •
Missing some Tweet in this thread? You can try to
force a refresh