Covid (@UCSF) Chronicles, Day 1038
Some folks continue asking what I'm doing viz Covid behavior...
Answer: I'm changing my behavior. In the Bay Area, I'm now OK with indoor dining & removing my mask for small group gatherings.
I haven't changed, the risk has. Here's how: (1/25)
Some folks continue asking what I'm doing viz Covid behavior...
Answer: I'm changing my behavior. In the Bay Area, I'm now OK with indoor dining & removing my mask for small group gatherings.
I haven't changed, the risk has. Here's how: (1/25)
Specifically, I haven't changed my perspective on balancing prudent caution with everyone's (including my) desire for "normal."
But, in the Bay Area at least, the Covid risk has come down considerably, and, by my way of thinking, this allows for a more permissive approach.(2/25)
But, in the Bay Area at least, the Covid risk has come down considerably, and, by my way of thinking, this allows for a more permissive approach.(2/25)
Where I'm coming from:
1) I'm 65 & haven't had Covid
2) I want to live as fully as I can, but am comfortable taking reasonable steps to avoid infection
3) I'm fully vaxxed & had bivalent in Sept
4) My main fear is Long Covid, which I peg at ~5% probability per Covid case. (3/25)
1) I'm 65 & haven't had Covid
2) I want to live as fully as I can, but am comfortable taking reasonable steps to avoid infection
3) I'm fully vaxxed & had bivalent in Sept
4) My main fear is Long Covid, which I peg at ~5% probability per Covid case. (3/25)
As I've described
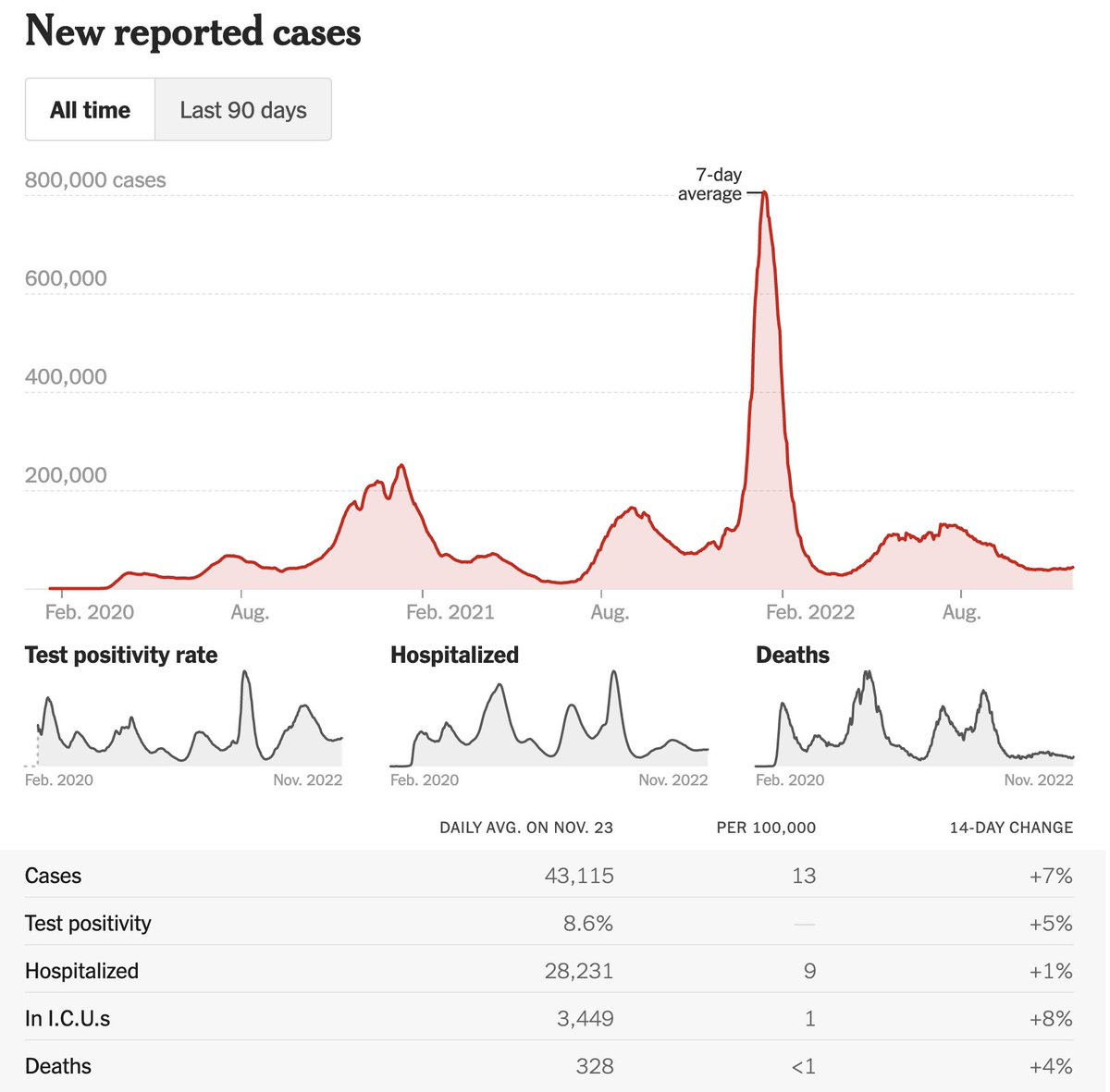
https://twitter.com/bob_wachter/status/1607162086282645505, this leads me to being comfortable indoors without a mask when the effective case rate is <10/100K/d in my region. This # is based on my own risk tolerance & risk factors. Some people may choose to accept more risk, others less.(4/25)
Because fewer people are testing in general, & more testing is at home, published case rates aren't as useful as they used to be. But trends in case rates are likely to still be meaningful, particularly if they agree with other data sources that are less subject to bias. (5/25)
That's how I approach things: I look at the published case rates in my region, and then look at other data sources less subject to measurement/reporting bias. The latter are:
1) Wastewater
2) Covid hospitalizations
3) Our @UCSFHospitals asymptomatic test positivity rate (6/25)
1) Wastewater
2) Covid hospitalizations
3) Our @UCSFHospitals asymptomatic test positivity rate (6/25)
None of these measures are perfect. Wastewater is a great, unbiased measure of circulating virus trends in a population, but it doesn't really give you a good answer to "What are the chances that a person at my table in a restaurant has Covid and is infectious?" (7/25)
Hospitalizations are influenced by the age of the population, co-morbidities, vaccination rates, as well as the usual, "Is the person hospitalized 'with' vs. 'for' Covid" questions. But hospitalization trends also give a feel for how much Covid is in the region. (8/25)
@UCSFHospitals asymptomatic test + rate has been my go-to # for estimating the likelihood that a person who feels OK in SF has Covid. But it's a bit less reliable than it was since we're no longer testing all pre-op pts – only ones where surgeon or patient requests testing.(9/25)
Yet we're still doing a lot of asymptomatic testing (~300/d), & I'd guess that any bias introduced by voluntary testing might be to push the rate a bit higher – with people who ask for a test being ones who might have a reason to wonder if they're positive. And,... (10/25)
... like many of these data points, even if they're not perfect, the trends offer important insights. So if our asymptomatic test positivity rate is half of what it was last month (as is the case), I would assume there is a significant fall in Covid population prevalence. (11/25)
With all that as background, let's look at the numbers.
Per @nytimes, SF's current case rate is 14/100K/d. But NYT uses a 2-week average, and it's falling fast (down 25% in last 2 weeks). @SF_DPH has us at 99 cases/d (=12/100K/d; Fig), avg'd over 1 week and also falling. (12/25)
Per @nytimes, SF's current case rate is 14/100K/d. But NYT uses a 2-week average, and it's falling fast (down 25% in last 2 weeks). @SF_DPH has us at 99 cases/d (=12/100K/d; Fig), avg'd over 1 week and also falling. (12/25)
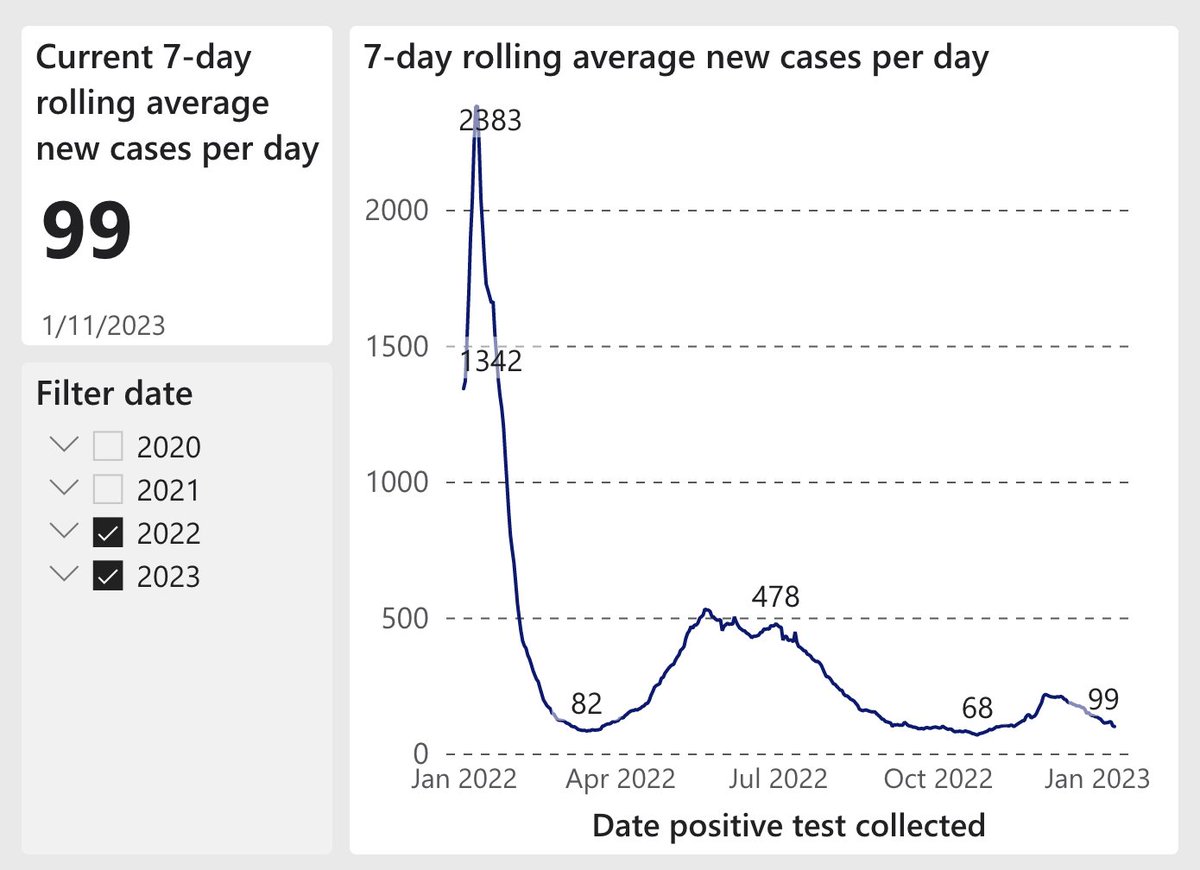
So it's reasonable to assume that case rate is ~10/100K/d in SF today.
Does that jive with the other, more reliable measures?
Wastewater (SF) is shown below. Again, hard to translate this into quantitative risk, but it supports the premise that there's less virus around. (13/25)
Does that jive with the other, more reliable measures?
Wastewater (SF) is shown below. Again, hard to translate this into quantitative risk, but it supports the premise that there's less virus around. (13/25)

Next, hospitalizations @UCSFHospitals. Again, not easy to translate this into risk of, say, indoor dining, but trend line certainly supports the premise that there's less virus around than last month. BTW, our 22 patients in hospital today compares with ~150 in Jan 2022. (14/25) 

Finally, there's @UCSFHospitals asymptomatic test pos. rate (Fig). It's now 2.4%, down from ~5% in Dec. This implies 1-in-42 asymptomatic folks would test positive. But since it's a PCR, ~half wouldn't be infectious (PCR stays + for ~15-20d; infectious for ~5-10d). So...(15/25) 
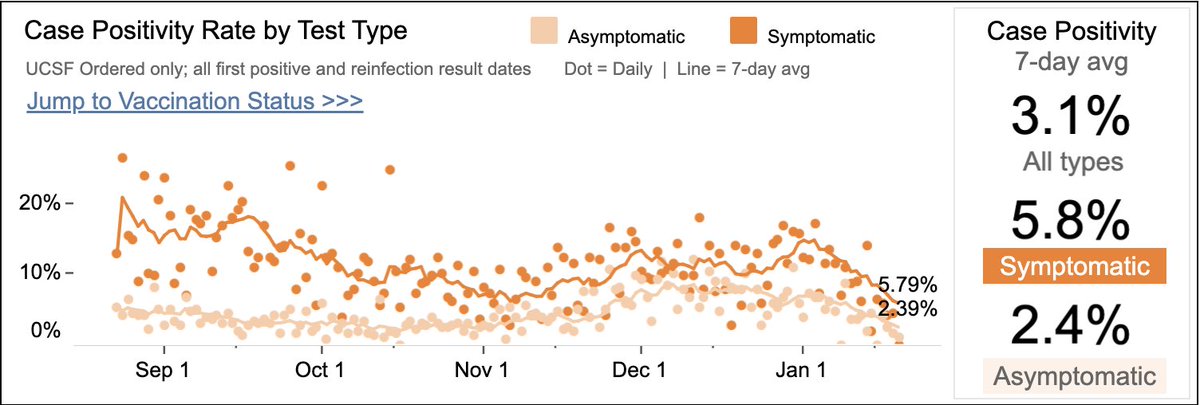
...a 2.4% rate implies ~1-in-100 folks who feel well may be infectious. To me, that's still a reason to prefer outdoor dining over indoor, to add ventilation when feasible, & consider testing before hi-risk gatherings. But it's low enough for me to drop my guard a bit. (16/25)
In Oct-Dec, the additional threats of RSV & flu served as a tiebreaker -- ie, if it was a close call, I'd favor caution since, while the above precautions are to decrease Covid risk, the same practices also help with Flu/RSV. But these two threats have also receded a lot. (17/25)
So there you have it. Based on all of this data and analysis, what am I doing in specific situations?
(18/25)
(18/25)
Dining:
I'm having dinner indoors w/ wife & kids tonight in SF.
But we're seeing older friends in Palm Springs this weekend: we'll eat outdoors & test before we arrive. Ditto when I visit my 87 year old mom in FL next month (case rate in FL is twice CA's, & going up). (19/25)
I'm having dinner indoors w/ wife & kids tonight in SF.
But we're seeing older friends in Palm Springs this weekend: we'll eat outdoors & test before we arrive. Ditto when I visit my 87 year old mom in FL next month (case rate in FL is twice CA's, & going up). (19/25)
Public transit, theaters, other large gatherings:
Plan to wear a mask (always a KN95; why not wear a good mask if you're going to mask?), likely forever. I'm comfortable taking it off briefly to eat on a long flight, but will try to keep it on when I can.(20/25)
Plan to wear a mask (always a KN95; why not wear a good mask if you're going to mask?), likely forever. I'm comfortable taking it off briefly to eat on a long flight, but will try to keep it on when I can.(20/25)
Small indoor gatherings:
Poker – I'm now comfy playing with a small, vaccinated group (n=8) without testing. I'll lobby (till they throw me out) to keep the doors/windows open during the game.
I'll do the same with other small indoor gatherings (eg, friends at the house).(21/25)
Poker – I'm now comfy playing with a small, vaccinated group (n=8) without testing. I'll lobby (till they throw me out) to keep the doors/windows open during the game.
I'll do the same with other small indoor gatherings (eg, friends at the house).(21/25)
Shopping:
30 minutes in a crowded Safeway: I'll keep wearing my mask.
Darting into an uncrowded bodega to get ice cream: I probably won't wear it. (Probably shouldn't eat the ice cream either, but that another story.) (22/25)
30 minutes in a crowded Safeway: I'll keep wearing my mask.
Darting into an uncrowded bodega to get ice cream: I probably won't wear it. (Probably shouldn't eat the ice cream either, but that another story.) (22/25)
As always, I'm not telling anybody what they SHOULD do. Perfectly reasonable people have looked at all of these odds (or decided not to) and chosen to live life like it's 2019. Most of them will do just fine – they'll have a higher odds of getting Covid than me, but...(23/25)
.... few will get super sick (particularly if up to date on vax), & most won't get Long Covid (either prolonged symptoms or be victim of elevated long-term risk of stroke, MI, or cognitive decline).
And I have no doubt that there's some joy in getting back to "normal." (24/25)
And I have no doubt that there's some joy in getting back to "normal." (24/25)
But I continue to be guided by the current risk, & so I'll continue to follow case rates & other metrics. And, if warranted, I'll re-up my precautions. Just because we're all tired of this doesn't change the risks & thus doesn't change the way I think about managing them.(25/end)
• • •
Missing some Tweet in this thread? You can try to
force a refresh