v2.0 with adjustments
Radicular pain and/or radiculopathy. A thread on decision making.
1⃣ Setting the scene
3Ps/serious pathology (red lines) aside. What does the evidence tells us?
✳️Wait & see
✳️Physiotherapy interventions
✳️Nerve root block
✳️Microdiscectomy
👇👇👇
Radicular pain and/or radiculopathy. A thread on decision making.
1⃣ Setting the scene
3Ps/serious pathology (red lines) aside. What does the evidence tells us?
✳️Wait & see
✳️Physiotherapy interventions
✳️Nerve root block
✳️Microdiscectomy
👇👇👇

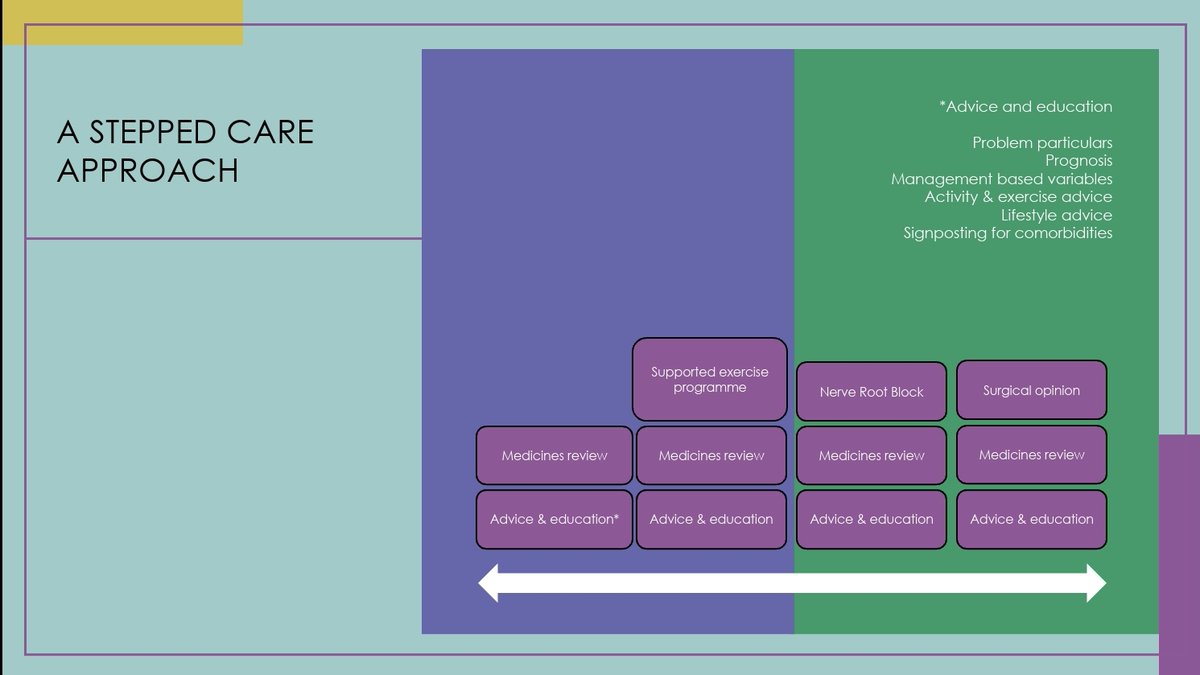
2⃣ A stepped care approach
So, who will get better anyway? What about relieving suffering? We only have early work into trajectories and prognostics.
Current guidelines and national pathways recommend a stepped approach. One that is 'least intrusive'.
👇👇👇
So, who will get better anyway? What about relieving suffering? We only have early work into trajectories and prognostics.
Current guidelines and national pathways recommend a stepped approach. One that is 'least intrusive'.
👇👇👇
3⃣ Management variables
What characteristics should we consider? To map onto the stepped care approach.
✳️Confidence in dx
✳️Prognostics
✳️Additional factors
What characteristics should we consider? To map onto the stepped care approach.
✳️Confidence in dx
✳️Prognostics
✳️Additional factors
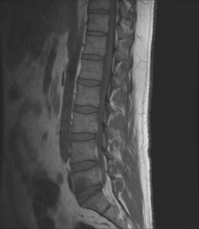
4⃣ Confidence in dx
Does the story fit?
Is symptomology consistent?
Does the pt have clear muscle power loss? Any objective numbness with clear borders?
👇👇👇
Does the story fit?
Is symptomology consistent?
Does the pt have clear muscle power loss? Any objective numbness with clear borders?
👇👇👇

5⃣ Prognostics
Green: Positive prognostically
Red: Negative prognostically
Use these to plan care and have sensible conversations with pts.
👇👇👇
Green: Positive prognostically
Red: Negative prognostically
Use these to plan care and have sensible conversations with pts.
👇👇👇

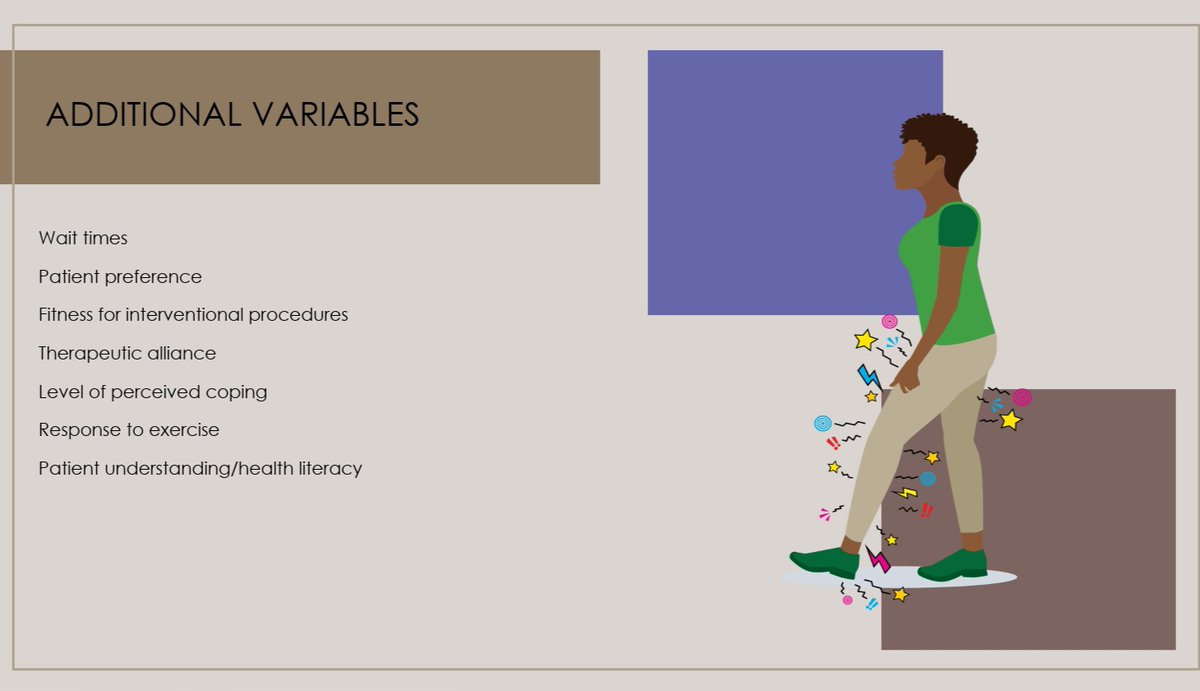
6⃣Additional variables
Does your pt even want to consider interventional procedures ? Do they understand their options.
Gone are the days that pt MUST have interventions done to them.
What about surgical fitness?
#SharedDecisionMaking
👇👇👇
Does your pt even want to consider interventional procedures ? Do they understand their options.
Gone are the days that pt MUST have interventions done to them.
What about surgical fitness?
#SharedDecisionMaking
👇👇👇
7⃣
So remember, a stepped approach with least level of intrusiveness. Remember your redlines.
For further CPD come attend our annual @NatSpineNetwork event
mailchi.mp/boa/nsn-17-apr…
Also check out our NHS booklets
southtees.nhs.uk/services/back-…
@AnninaBSchmid @SiobhanStynes
So remember, a stepped approach with least level of intrusiveness. Remember your redlines.
For further CPD come attend our annual @NatSpineNetwork event
mailchi.mp/boa/nsn-17-apr…
Also check out our NHS booklets
southtees.nhs.uk/services/back-…
@AnninaBSchmid @SiobhanStynes
• • •
Missing some Tweet in this thread? You can try to
force a refresh