How does primary SARS-CoV-2 infection compare to mRNA vaccination when it comes to autoantibody development? @_BlueJay3 led an effort with @VirusesImmunity and her lab and our @BRIseattle collaborators to answer this question: nature.com/articles/s4146…
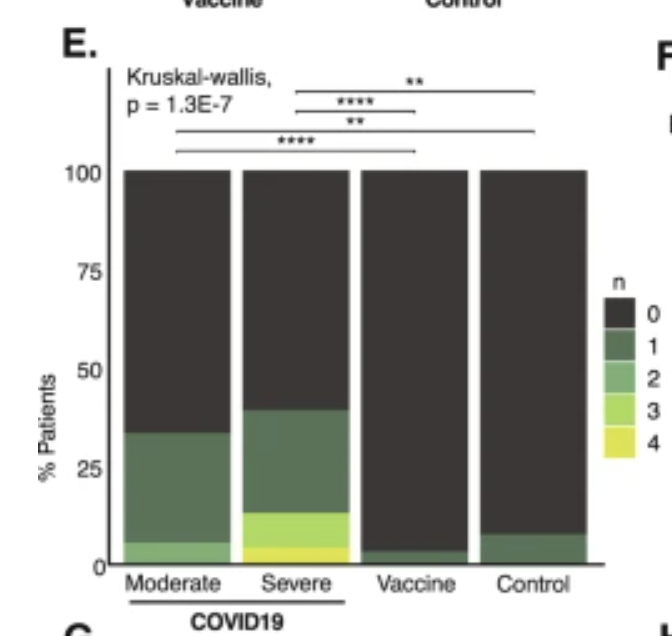
We and others previously found that SARS-CoV-2 infection is associated with the development of new autoantibodies (AAbs), with a trend towards increasing AAb levels with more severe infection. nature.com/articles/s4158…
In this report, we find that in both healthy individuals and patients with pre-existing autoimmune diseases, there is no detectable net increase in AAbs after mRNA vaccination using our REAP method.
Changes in AAb levels after vaccination look like unvaccinated controls followed longitudinally in terms of the # of new reactivities detected. The # of new reactivities in COVID-19 is likely an underestimate as we don't have a pre-infection baseline in most cases. 
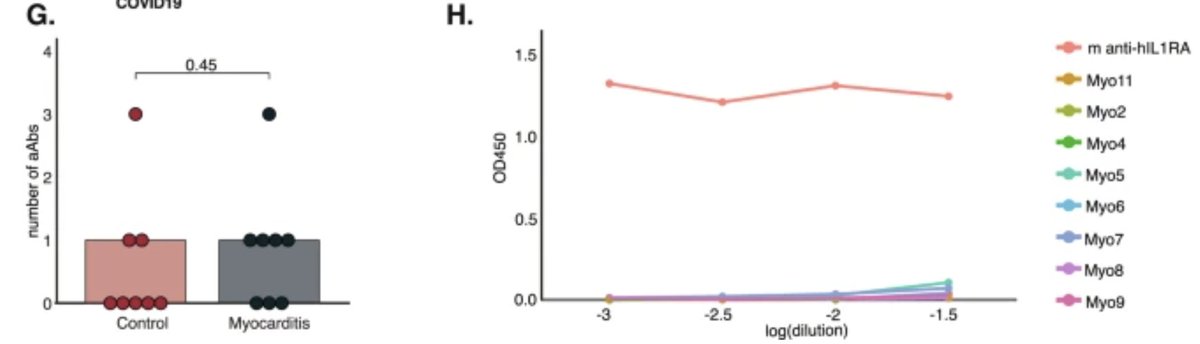
We also looked at AAbs in patients who developed vaccine-associated myocarditis. We did not detect elevated numbers of reactivities in these patients relative to age-matched controls. Notably, we did not detect anti-IL1Ra AAbs in any patient, a contrast to a previous NEJM report. 
To be clear, our results do not definitively rule out that mRNA vaccination can drive the formation of new AAbs. If that does occur, it is a relatively rare phenomenon compared to its high incidence with infection. Thus, mRNA vaccines 'decouple' AAb risk from SARS-CoV-2 immunity.
Mechanistically, these results seem to decrease the likelihood that new AAbs seen with SARS-CoV-2 infection are due to 'molecular mimicry' against the spike protein, as the vaccinated patients develop excellent responses to spike as expected without AAbs.
This was a great collaboration with many fantastic scientists, including @carolilucas, @InciYildirim11, Cate Speake, and Jane Buckner. (End)
• • •
Missing some Tweet in this thread? You can try to
force a refresh