Some of the issues with "foregone clinical checks" – where a clinical check is done on a prescription supply then no check is completed for any number of subsequent supplies occurring within a defined period - have not yet been highlighted by #pharmacy bodies.
Thread 🧵/
Thread 🧵/
Pharmacists considering raising concerns to the superintendent (“SI”) about foregone clinical checks should remember that the SI has already signed off on the procedure.
2/
2/
In the companies using FGCs, a paper will have been put to the SI and directors explaining that reducing clinical checking frequency would make the company more profit, through associated staffing cuts, and/or pharmacists spending more time on other profitable activities.
3/
3/
The patient safety risks will also have been set out in the paper. The company will have decided it was worth taking these risks to acquire the profit increase.
The risk considerations for individual pharmacists are unlikely to be the same.
4/
The risk considerations for individual pharmacists are unlikely to be the same.
4/
Centrally-set staffing budgets will already have been cut to reflect the new foregone clinical check procedure. This will “automate” the attempted enforcement of the procedure, with minimal effort from the company.
5/
5/
If pharmacists perform clinical checks for each supply, they won't be given the time for it. The staffing model will automatically put pressure on those who dissent; they will have less time to fulfil other duties, though these duties will remain, and may have been increased.
6/
6/
Somewhere within a company spreadsheet and/or database, there will be one or more formula changes to the staffing model to reflect the fact that pharmacists are no longer given time to conduct clinical checks on each supply.
7/
7/
There will likely also be an accompanying paper from the team that deals with the staffing model which describes the purpose and effect of the changes, and associated correspondence.
8/
8/
Would patients, pharmacists and their legal advisors know to expect such things to be disclosed in the course of legal proceedings? Would they be disclosed voluntarily?
9/
9/
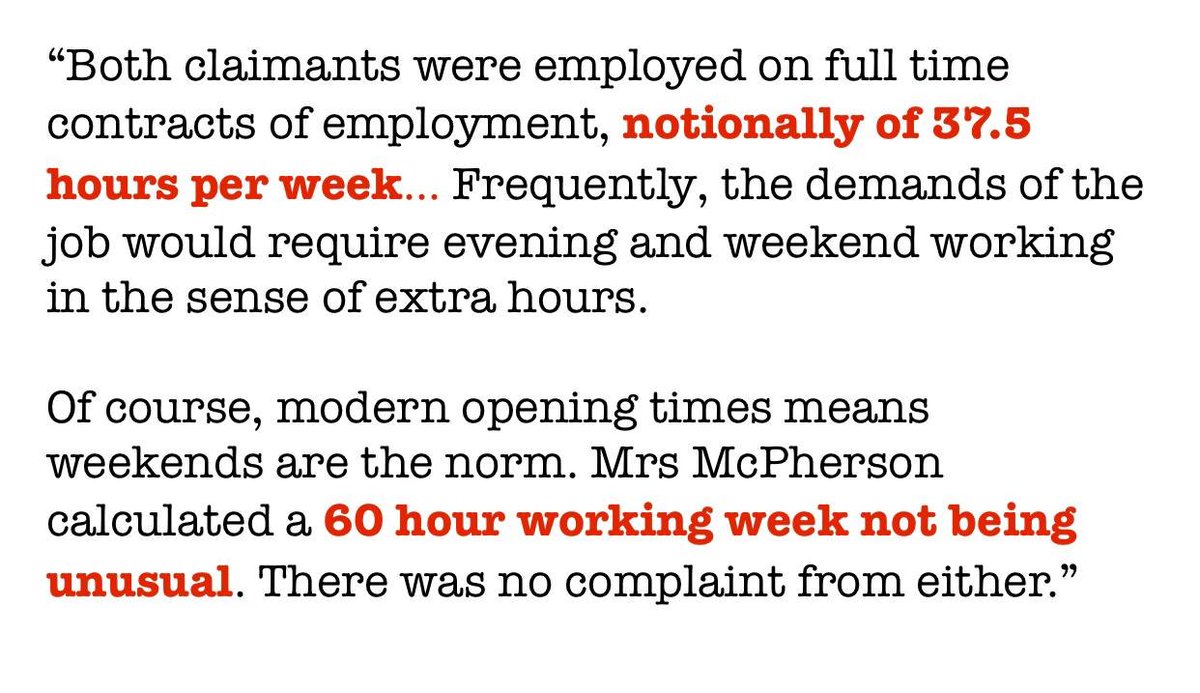
The multiples also have a problem in respect of liability because they’re unable to demonstrate that pharmacists *have* enough time to do all of the tasks expected of them (it can’t be demonstrated if it isn’t the case).
10/
10/
If it's not possible for pharmacists to fulfil all their duties within the finite time they have, including clinically checking each supply, then some activity or another will need to be foregone.
11/
11/
It may be presented as a choice to pharmacists: do they want to use the foregone clinical check procedure? If they want to check each supply, they will be put under time pressure, and potentially admonished for not hitting targets.
12/
12/
If a pharmacist raises concerns to the effect that foregone clinical checks are inappropriate, but then relies on them and it results in patient harm, the company could argue that not only did the pharmacist cause the harm, but believed that his/her own actions were wrong.
13/
13/
The company could say that in the alternative, the pharmacist must, having decided to press ahead, have reconsidered his/her position after careful thought, and decided it wasn't a problem - so it’s for the pharmacist to explain why that’s now the case.
14/
14/
These arguments may arise in different circumstances, such as regulatory or employment proceedings, or negligence claims, with varying likelihood. That likelihood will depend on factors such as the company’s desire to protect its profit, by protecting its reputation.
15/
15/
A pharmacist who supplies a medicine in reliance on a foregone clinical check, where patient harm results from some clinical issue that would otherwise have been detected, should expect to incur some liability in a clinical negligence claim.
16/
16/
The initial clinical checker may incur some liability, too, through instructing others that a clinical check is not required and accepting responsibility for the future clinical appropriateness of the supply.
17/
17/
Employers are vicariously liable for the actions of their employees, and most claims will be brought against the employer, since they are at least perceived to be in a better position to pay.
18/
18/
This may be leveraged, since complainants will know that employers will be keen to protect their profits by protecting their reputations. From a pharmacist’s perspective, when such claims are settled, will he/she see what is said about him/her in the letter to the claimant?
19/
19/
In respect of regulation, how would a competent, non-corrupt regulator apportion blame, between the initial clinical checker, the one who failed to further check, the SI who signed off on the procedure, and the company that designed and introduced it?
20/
20/
Each party would have competing interests in arguing that the other was at fault / the most at fault from a regulatory perspective. The parties may be close colleagues, and may have the same indemnity insurance / legal defence provider.
21/
21/
A further issue is that dispensing staff may be instructed not to send the prescriptions for clinical checking where relying on the foregone clinical checking procedure.
22/
22/
A dispensed medicine may be handed out without any clinical check being performed specifically on that supply. Or, a medicine may be dispensed, accuracy checked and handed out, without involving the pharmacist on duty - because the procedure says no clinical check is needed.
23/
23/
The pharmacist on duty may not even be informed by colleagues that they are dispatching some prescriptions without a clinical check having been conducted on that supply.
24/
24/
It is a pity that the people who work at the head offices of the multiples devising such changes don't put their talents to use improving patient safety, instead of initiatives at the expense of it.
25/
25/
It's standard practice in the multiples to run significant changes like this past the GPhC in advance of any wider discussion, to get its rubber stamp and limit the chance of any blowback. Pharmacists should not expect anything to come of concerns being raised to the GPhC.
26/
26/
It is worth noting that such "foregone clinical checks” were introduced around four years ago, by a multiple. There has been no meaningful comment on it from pharmacy bodies in the meantime.
27/
27/
• • •
Missing some Tweet in this thread? You can try to
force a refresh