
The specialty of #CriticalCare has achieved important advances in survival for many patients with the most complex disorders. Along with these advances, however, there has been an increasing awareness of the complicated and persistent morbidity that follows critical illness. 1/10
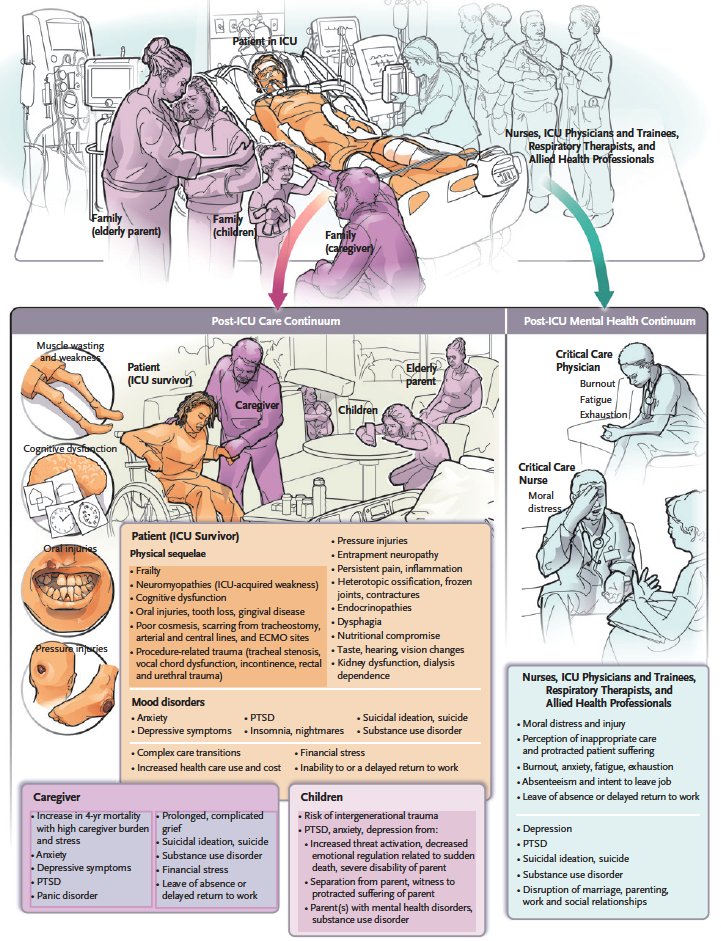
Episodes of critical illness result in multidimensional acquired or exacerbated conditions that may persist for years after the critical illness and may not be wholly reversible. Health inequities may worsen these outcomes. 2/10
A continuum of care for patients and families after critical illness, extending from the ICU to community or primary care, must become the standard of care and be developed concurrently with basic science inquiry to elucidate the multiple mechanisms of morbidity. 3/10 
Transparent and public reporting of long-term ICU outcomes is fundamental for obtaining informed consent to initiate and continue treatment, aligning care with patient and family values, and ensuring accountability for the high human and financial costs of these outcomes. 4/10
ICU-acquired weakness is prevalent among ICU survivors and encompasses a critical illness myopathy (myosin-depletion myopathy), polyneuropathy (axonopathy), or a combination of these disorders. 5/10
ICU outcomes data highlight myriad coexisting conditions including frailty, oral and dental complications, swallowing difficulties, taste changes, vision or hearing loss, new need for renal replacement therapy, procedure-related trauma, and others. 6/10 

High frequencies of symptoms of anxiety, depression, PTSD, and prolonged grief disorder have been reported among family members of ICU patients. 7/10
When a patient dies in the ICU, subsequent distress in the family is more common, more severe, and more lasting than in family members of patients who survive. Other patient outcomes, such as persistent disability, also influence the family. 8/10 

The literature on long-term ICU outcomes is robust across a broad spectrum of patient and caregiver groups, yet long-term outcomes are not a prominent part of the ICU lexicon. Our patients and their families need this to change. 9/10 

To learn more, read “Outcomes after Critical Illness” by Margaret S. Herridge, M.D., M.P.H., and Élie Azoulay, M.D., Ph.D.: nej.md/3kUs4bK 10/10
• • •
Missing some Tweet in this thread? You can try to
force a refresh






