For those following along as we continue the countdown to #MatchDay2023, it’s now time for Part 4 in our six-part series.
Yesterday, I described how the NRMP did their best to ignore one doctor’s fight to make the matching algorithm applicant-optimal.
Today, I’ll explain why.
Yesterday, I described how the NRMP did their best to ignore one doctor’s fight to make the matching algorithm applicant-optimal.
Today, I’ll explain why.
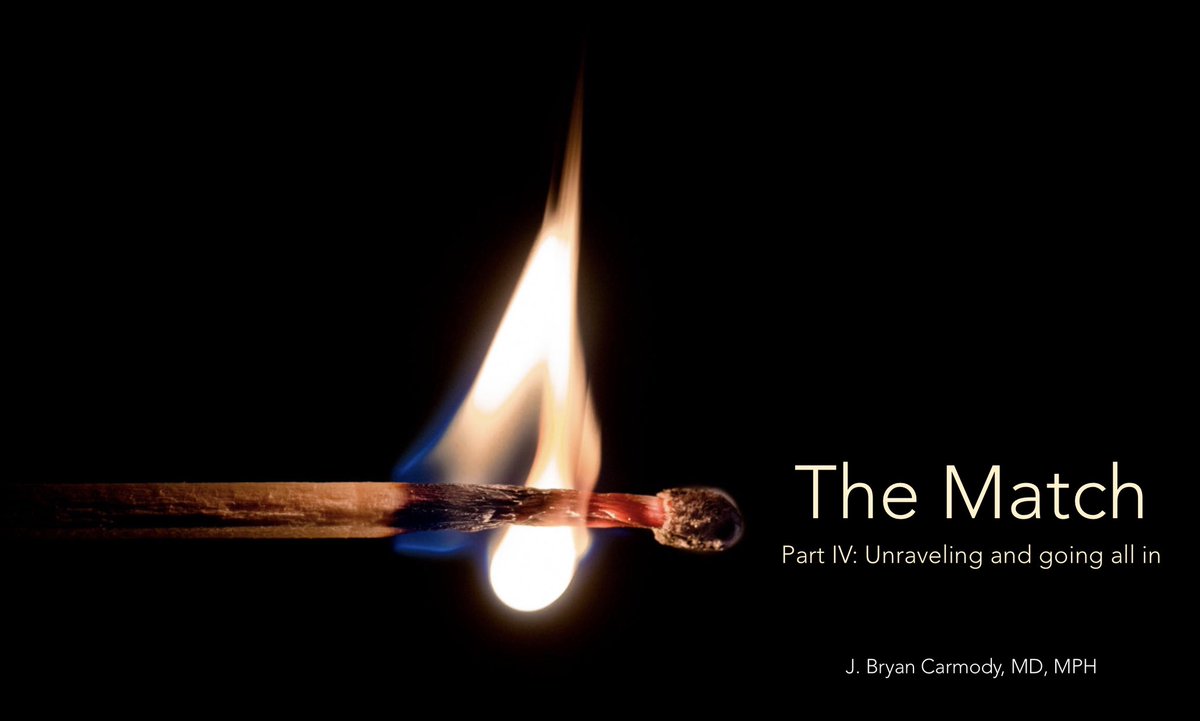
We’ll cover why outside-the-match offers threaten the existence of the match; how the GI fellowship match failed; and why the NRMP fought so hard for their “All In” policy.
It’s all here:
The Match, Part 4: Unraveling and going all in
It’s all here:
The Match, Part 4: Unraveling and going all in
If you missed yesterday’s thread, it’s here:
https://twitter.com/jbcarmody/status/1635317117573820416
And if you missed the earlier videos, let me help you get caught up:
The Match, Part 1: Why do we have a Match?
The Match, Part 2: The battle for the algorithm
The Match, Part 3: On marriages and matching
The Match, Part 1: Why do we have a Match?
The Match, Part 2: The battle for the algorithm
The Match, Part 3: On marriages and matching
• • •
Missing some Tweet in this thread? You can try to
force a refresh