
The Sheriff of Sodium | Pediatric nephrologist | Associate professor | APD | Husband | Dad | Virginian | Advocate for medical students and common sense
4 subscribers
How to get URL link on X (Twitter) App


 First, stop and think.
First, stop and think.
 First, the data.
First, the data.
https://twitter.com/jbcarmody/status/1765118274604314720

 If you’ve somehow missed all of this, here’s a typical article (which happens to be the one I screenshotted above).
If you’ve somehow missed all of this, here’s a typical article (which happens to be the one I screenshotted above).
https://twitter.com/jbcarmody/status/1757965502968672748The court will issue a ruling by February 21 - so the outcome of the suit remains uncertain.
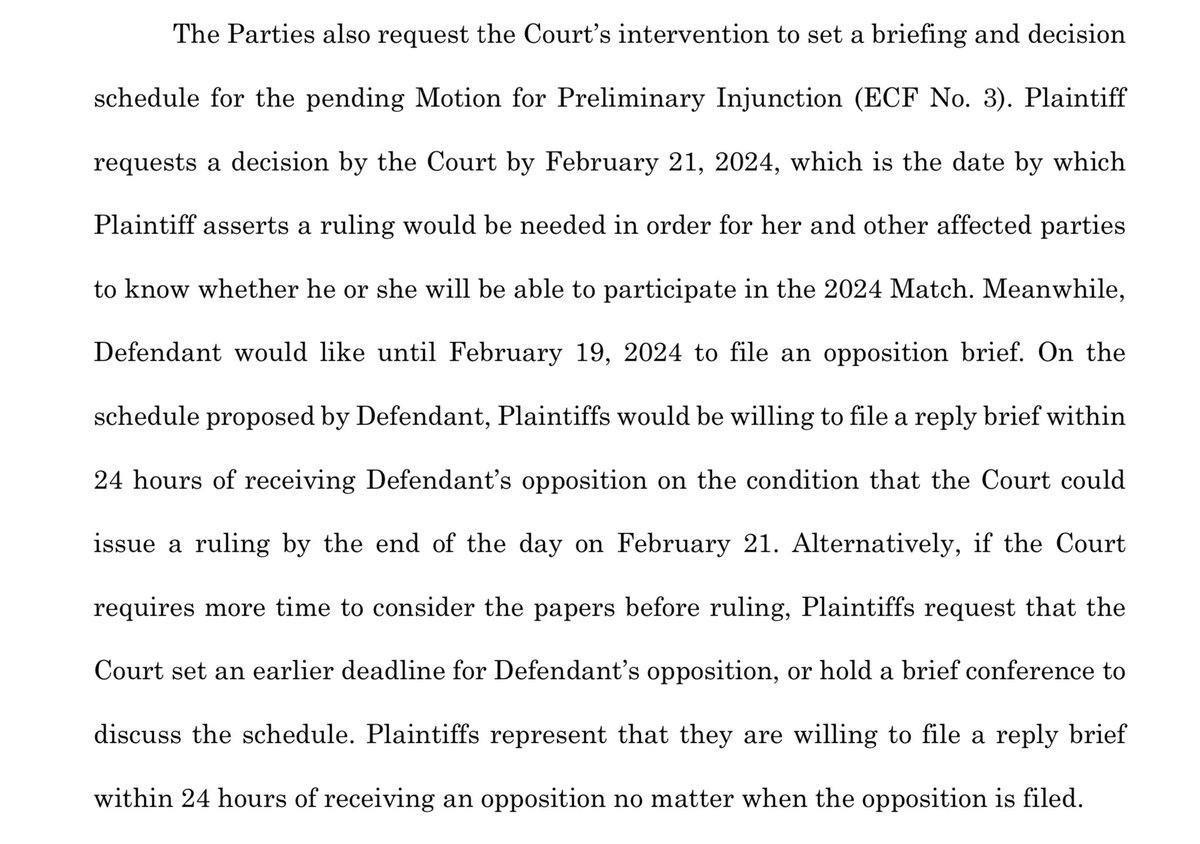
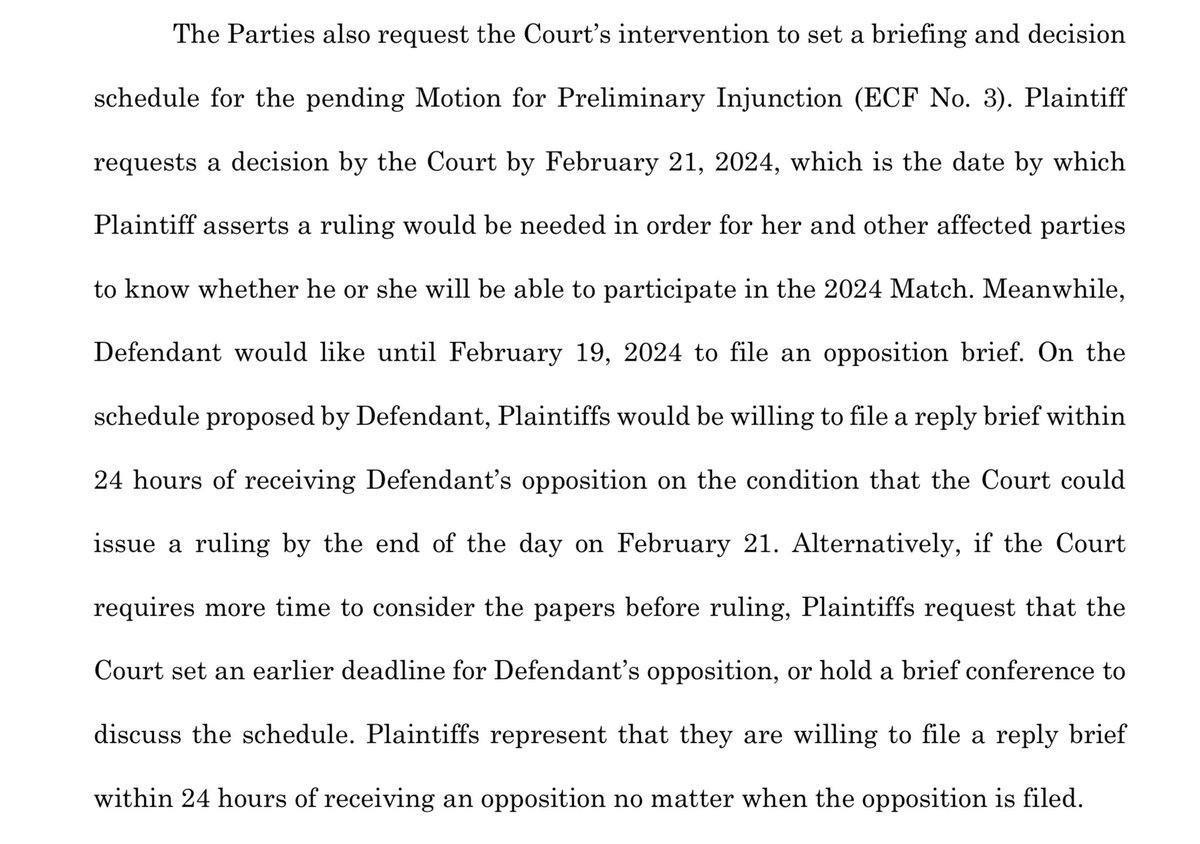 The suit alleges that the NBME did not follow its own policies by invalidating scores before the involved examinees had an opportunity to appeal.
The suit alleges that the NBME did not follow its own policies by invalidating scores before the involved examinees had an opportunity to appeal. 
https://twitter.com/jbcarmody/status/1745596493120029083Some background:



 The short answer is, “because the American Board of Pediatrics requires it.”
The short answer is, “because the American Board of Pediatrics requires it.”



 Quick background:
Quick background:

 The document goes on for pages and pages - 18 in all - outlining the hospital’s expectations of and obligations to the resident.
The document goes on for pages and pages - 18 in all - outlining the hospital’s expectations of and obligations to the resident.




 Again, this is the overall average… so many hospitals receive less. But some receive more.
Again, this is the overall average… so many hospitals receive less. But some receive more.

 WINNER: Experienced IMGs.
WINNER: Experienced IMGs.

 When the HealthONE family medicine residency shut down, the residents lost their jobs.
When the HealthONE family medicine residency shut down, the residents lost their jobs.
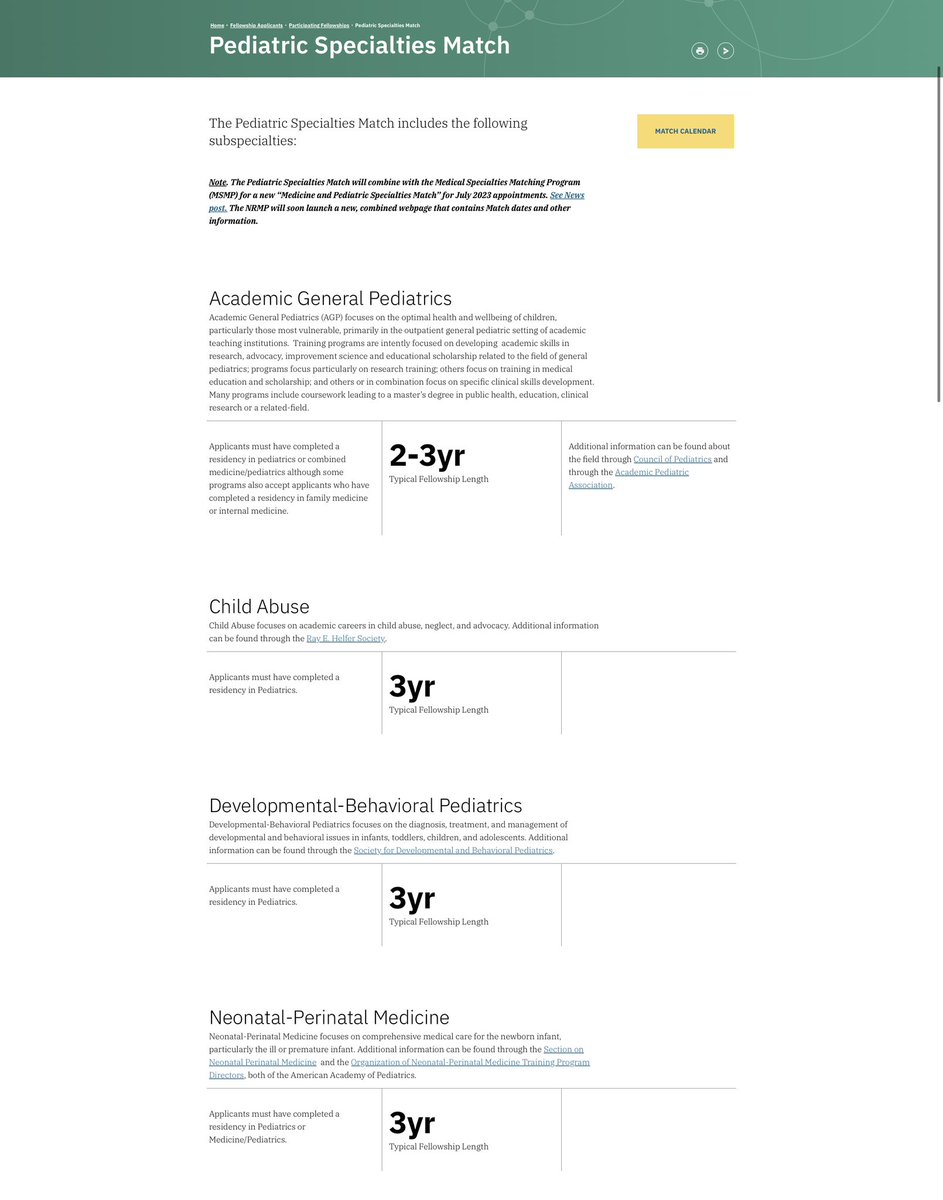
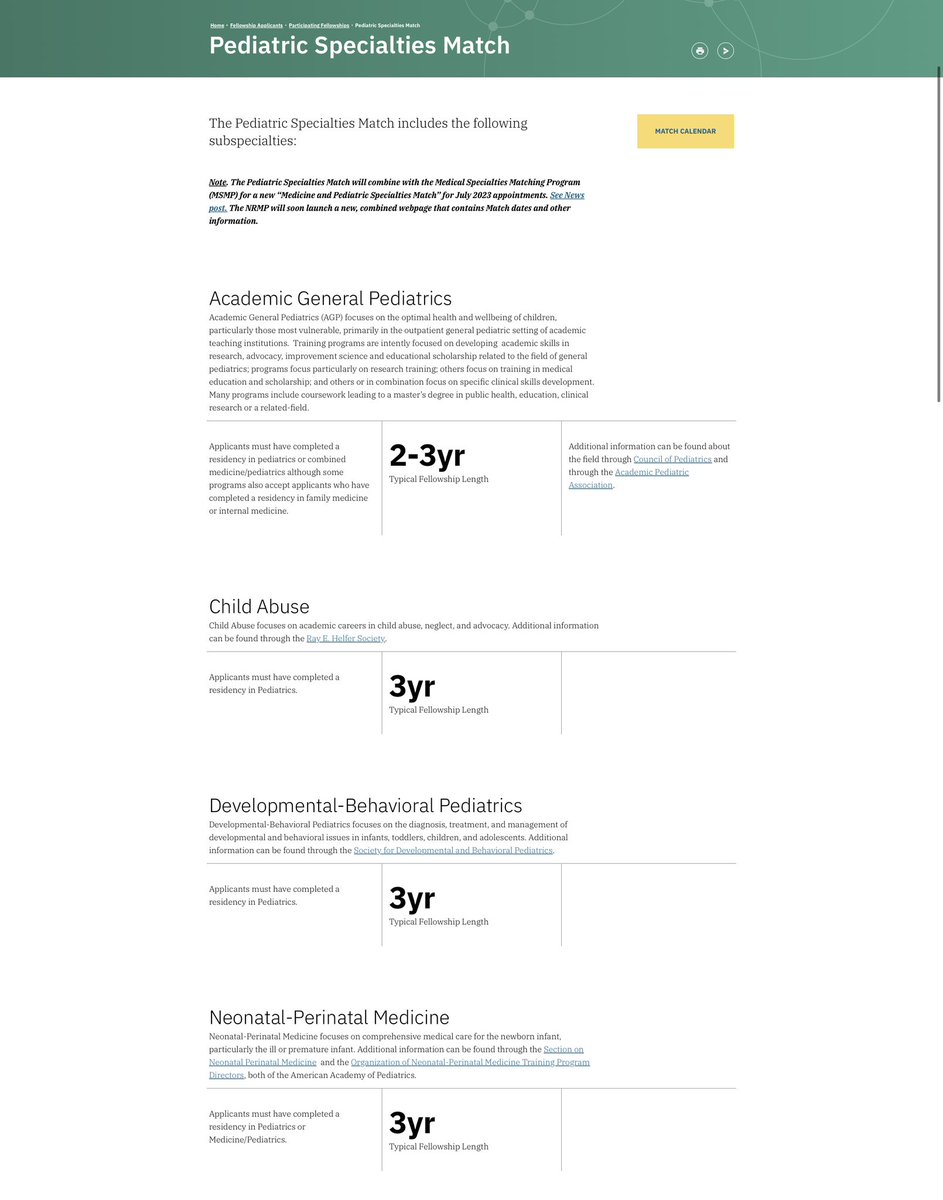
 We’ll cover why outside-the-match offers threaten the existence of the match; how the GI fellowship match failed; and why the NRMP fought so hard for their “All In” policy.
We’ll cover why outside-the-match offers threaten the existence of the match; how the GI fellowship match failed; and why the NRMP fought so hard for their “All In” policy.https://twitter.com/jbcarmody/status/1635317245420371969At least say something like, “In response to student concerns that the existing algorithm advantaged programs [Williams reference], the NRMP Board commissioned a study…”

 Lemme explain.
Lemme explain.
https://twitter.com/ajkavanaugh/status/1632773278891667460The issue is the so-called “80/20 rule” of the Affordable Care Act.

https://twitter.com/jbcarmody/status/1628042230874210306WINNER: Patient caps.
