Just got done presenting at the 31st Annual Clinical Update in Geriatric Medicine, put on by @AHNtoday and @UPMC. Awesome attendees, as usual!
Was asked to talk about "Controversies in Antimicrobial Therapy"
Figured would share here.
#IDTwitter #MedTwitter
🧵
1/
Was asked to talk about "Controversies in Antimicrobial Therapy"
Figured would share here.
#IDTwitter #MedTwitter
🧵
1/

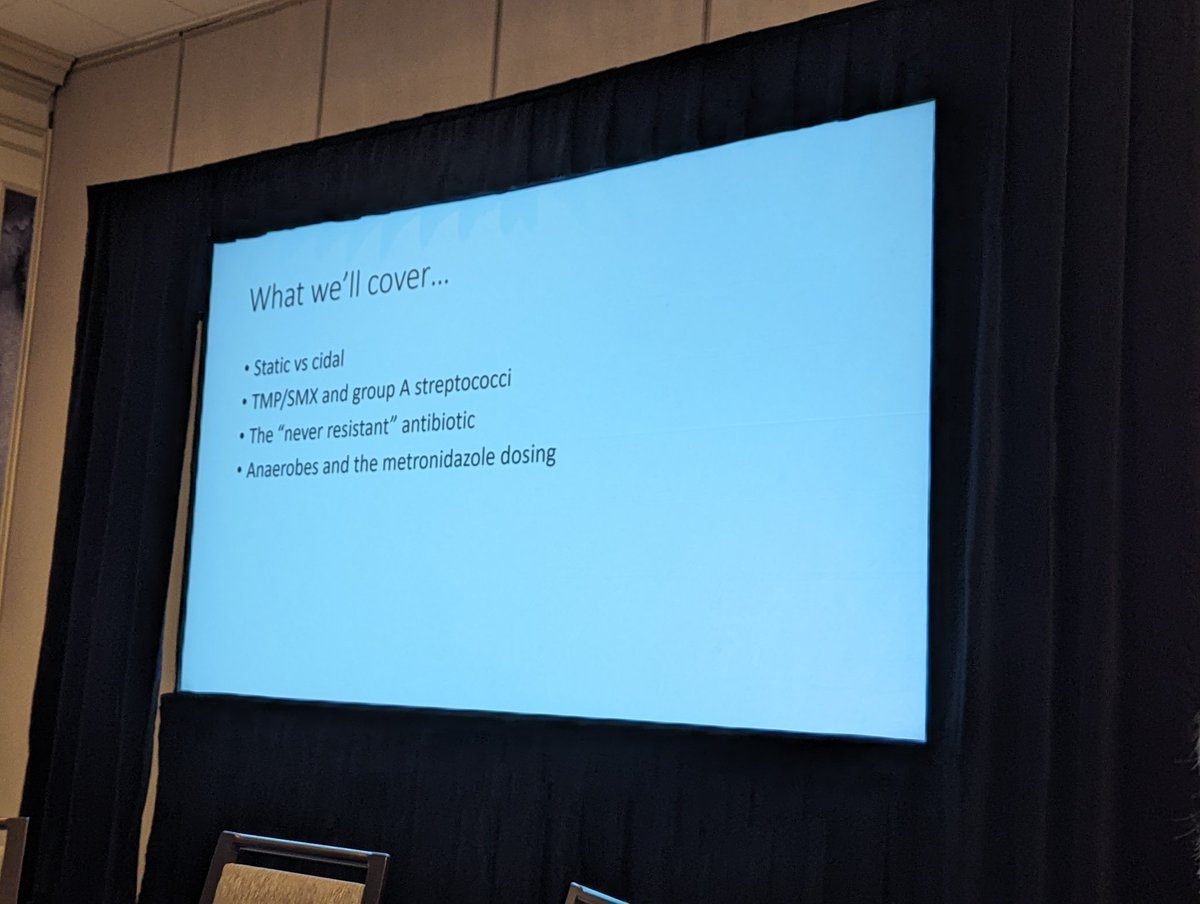
With a Geriatric audience, had to take the opportunity to focus first on the urine.
But also get into SSTI, Bactrim for Group A strep, if you need IV antibiotics for Lyme, dental prophylaxis for prosthetic joints, and duration of therapy.
First up - does +UA/UCx=UTI?
2/
But also get into SSTI, Bactrim for Group A strep, if you need IV antibiotics for Lyme, dental prophylaxis for prosthetic joints, and duration of therapy.
First up - does +UA/UCx=UTI?
2/

Emphatic NO on that one.
Need SYMPTOMS to diagnose a UTI.
I tell patients they need to tell us, we can't tell them.
Positive UCx without symptoms = asymptomatic bacteriuria.
3/

Need SYMPTOMS to diagnose a UTI.
I tell patients they need to tell us, we can't tell them.
Positive UCx without symptoms = asymptomatic bacteriuria.
3/


Asymptomatic bacteriuria is super common - up to 50% of women in nursing homes will have a positive urine culture on any given day.
When should we screen for ASB and treat it?
➡️ Pregnancy
➡️ Urologic procedures
That's about it. Doesn't help and may harm in everyone else.
4/


When should we screen for ASB and treat it?
➡️ Pregnancy
➡️ Urologic procedures
That's about it. Doesn't help and may harm in everyone else.
4/



Nope.
Lots of things can change the appearance and smell of the urine.
The thought of asparagus night at the nursing home gives this steward nightmares.
@TomWalshMD13 always says if the urine stinks, stop smelling it!
6/
Lots of things can change the appearance and smell of the urine.
The thought of asparagus night at the nursing home gives this steward nightmares.
@TomWalshMD13 always says if the urine stinks, stop smelling it!
6/

Here's a big one and one we see every day with stewardship.
Is altered mental status an indicator or UTI?
7/
Is altered mental status an indicator or UTI?
7/

NO!
Lots of things cause altered mental status.
There are some criteria that you can use if patients can't give a history. Best approach in a stable patient is hold antibiotics and look for other things (left side of algorithm here).
8/


Lots of things cause altered mental status.
There are some criteria that you can use if patients can't give a history. Best approach in a stable patient is hold antibiotics and look for other things (left side of algorithm here).
8/



Better safe than sorry? Just give the antibiotic?
We do a lot of harm with unnecessary antibiotics. They are not benign.
10/

We do a lot of harm with unnecessary antibiotics. They are not benign.
10/


"OK, I know you said only pregnancy and urologic procedures, but what about before joint replacement?"
11/
11/

Nope. Really, only urologic procedures. No other surgeries.
Screening urine cultures don't change the risk for prosthetic joint infection or risk of post-op UTI.
12/

Screening urine cultures don't change the risk for prosthetic joint infection or risk of post-op UTI.
12/


Ok, some people truly do have a UTI.
First line empiric therapy for us, and in most places: Nitrofurantoin.
We use cephalexin first line if can't use Nitrofurantoin.
Rates of resistance to FQs and TMP-SMX too high, and tons of adverse effects with FQs.
13/
First line empiric therapy for us, and in most places: Nitrofurantoin.
We use cephalexin first line if can't use Nitrofurantoin.
Rates of resistance to FQs and TMP-SMX too high, and tons of adverse effects with FQs.
13/

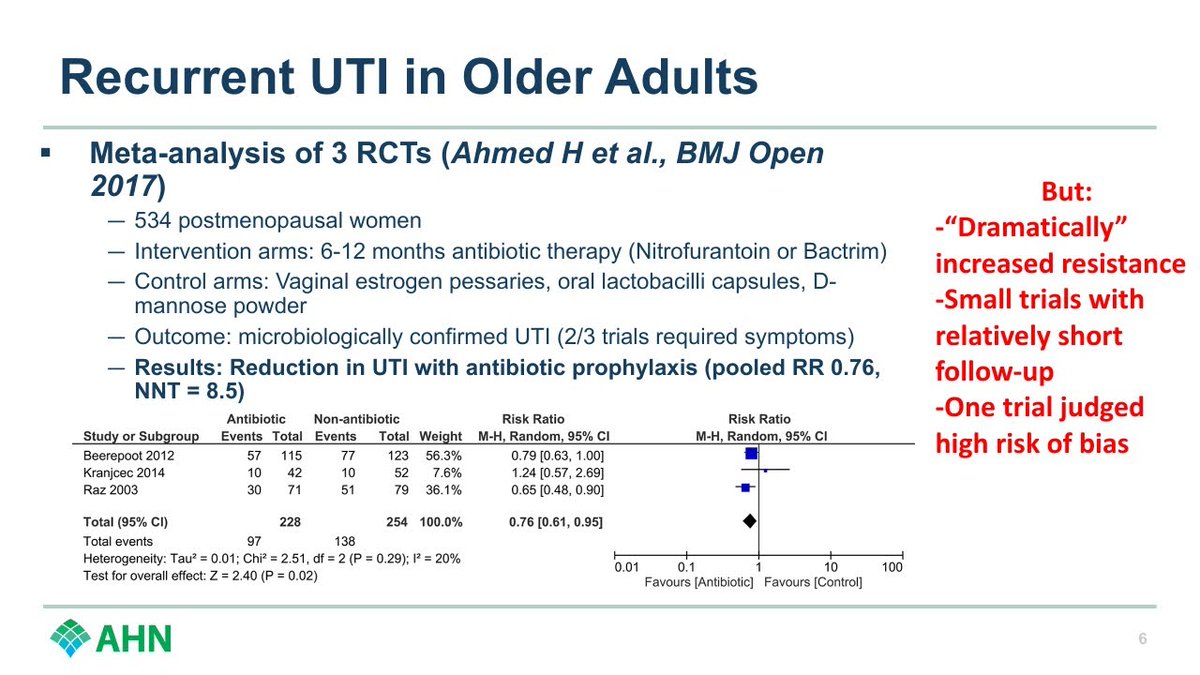
First, make sure it's truly recurrent UTI.
If it is, although there is a meta-analysis that may suggest benefit, was short follow up, had bias, and lots of resistance was seen.
Great work here from @BRxAD showing risks may outweigh benefits.
I don't recommend it.
15/



If it is, although there is a meta-analysis that may suggest benefit, was short follow up, had bias, and lots of resistance was seen.
Great work here from @BRxAD showing risks may outweigh benefits.
I don't recommend it.
15/




What can you do instead?
Consider non-antibiotic prophylaxis like topical estrogens or methenamine hippurate. Decent evidence for both.
16/
Consider non-antibiotic prophylaxis like topical estrogens or methenamine hippurate. Decent evidence for both.
16/

Ok, moving on from the urine.
Many of us were taught that Bactrim doesn't work for Group A strep.
Was that right?
17/
Many of us were taught that Bactrim doesn't work for Group A strep.
Was that right?
17/

First, quick overview of uncomplicated SSTIs.
Purulent
➡️ Usually MRSA/MSSA
➡️ I&D and culture
➡️ Bactrim
(RCTs on slide did longer, but I usually do 5 days after I&D)
18/
Purulent
➡️ Usually MRSA/MSSA
➡️ I&D and culture
➡️ Bactrim
(RCTs on slide did longer, but I usually do 5 days after I&D)
18/

Non-purulent
➡️ Usually beta-hemolytic strep
➡️ Cefadroxil (BID dosing easier than TID/QID of cephalexin)
Note dosing w/ ⬆️weight. Most failures I see were underdosed.
Pro tip: Look in between the toes. Bacteria have to get in somewhere. Treat tinea pedis if you find it.
19/

➡️ Usually beta-hemolytic strep
➡️ Cefadroxil (BID dosing easier than TID/QID of cephalexin)
Note dosing w/ ⬆️weight. Most failures I see were underdosed.
Pro tip: Look in between the toes. Bacteria have to get in somewhere. Treat tinea pedis if you find it.
19/


Ok, so does Bactrim cover Group A strep?
Yep, yep it does. Interesting why we thought it didn't.
@AshaBowen has done more than anyone to bust this myth.
20/

Yep, yep it does. Interesting why we thought it didn't.
@AshaBowen has done more than anyone to bust this myth.
20/


Clinical data supports it as well.
There is some Bactrim resistance in India, but fine in US, Europe, Australia.
Very local to me, we're about 99% susceptibile @AHNtoday. We'll publish that eventually. @ChristianCho @dnbrems
21/

There is some Bactrim resistance in India, but fine in US, Europe, Australia.
Very local to me, we're about 99% susceptibile @AHNtoday. We'll publish that eventually. @ChristianCho @dnbrems
21/


@SDoernberg did a great job busting this myth at #IDWeek2022
22/
https://twitter.com/NateShivelyMD/status/1583479966884597760?t=f9xwYbGFUsVwfaDvU18pkw&s=19
22/
First, quick overview of some of the forms.
Most common EM rash I see is a red circle, don't always have central clearing.
Just treat EM, don't test. New RCT evidence for 7 days doxy. #ShorterIsBetter
Bell's palsy in Western PA in the summer? Lyme until proven otherwise.
24/

Most common EM rash I see is a red circle, don't always have central clearing.
Just treat EM, don't test. New RCT evidence for 7 days doxy. #ShorterIsBetter
Bell's palsy in Western PA in the summer? Lyme until proven otherwise.
24/


We have solid evidence that PO doxycycline = IV Ceftriaxone for neurologic Lyme. No one needs to go home with a PICC.
In fact, guidelines support PO antibiotics for pretty much any form of Lyme disease. Don't let the "Lyme literate" folks convince your patients otherwise.
25/

In fact, guidelines support PO antibiotics for pretty much any form of Lyme disease. Don't let the "Lyme literate" folks convince your patients otherwise.
25/


Not enough tick talk for you?
Check out this talk from @matthewmof31 earlier this year.
26/
Check out this talk from @matthewmof31 earlier this year.
https://twitter.com/matthewmof31/status/1618992162544447490?t=28fPWnmPpv3978NNhIT5Tw&s=19
26/
Here's my take home slide from this year, but going to add some stuff from my talk last year just for fun.
27/
27/

Nope.
No evidence that it prevents prosthetic joint infections.
Guidelines have finally mostly evolved to that. Table from great paper from @idpharmd that reviews it.
29/

No evidence that it prevents prosthetic joint infections.
Guidelines have finally mostly evolved to that. Table from great paper from @idpharmd that reviews it.
29/


Generally still yes in some patients reviewed here.
But evidence is weak and some places don't do it.
31/
But evidence is weak and some places don't do it.
31/

Almost every time we look, we find #ShorterIsBetter
Love the campaign by @BradSpellberg and him tracking this for us.
(This is an old slide. Also some of these slides were stolen (with permission) from @matthewmof31).
33/
Love the campaign by @BradSpellberg and him tracking this for us.
(This is an old slide. Also some of these slides were stolen (with permission) from @matthewmof31).
33/

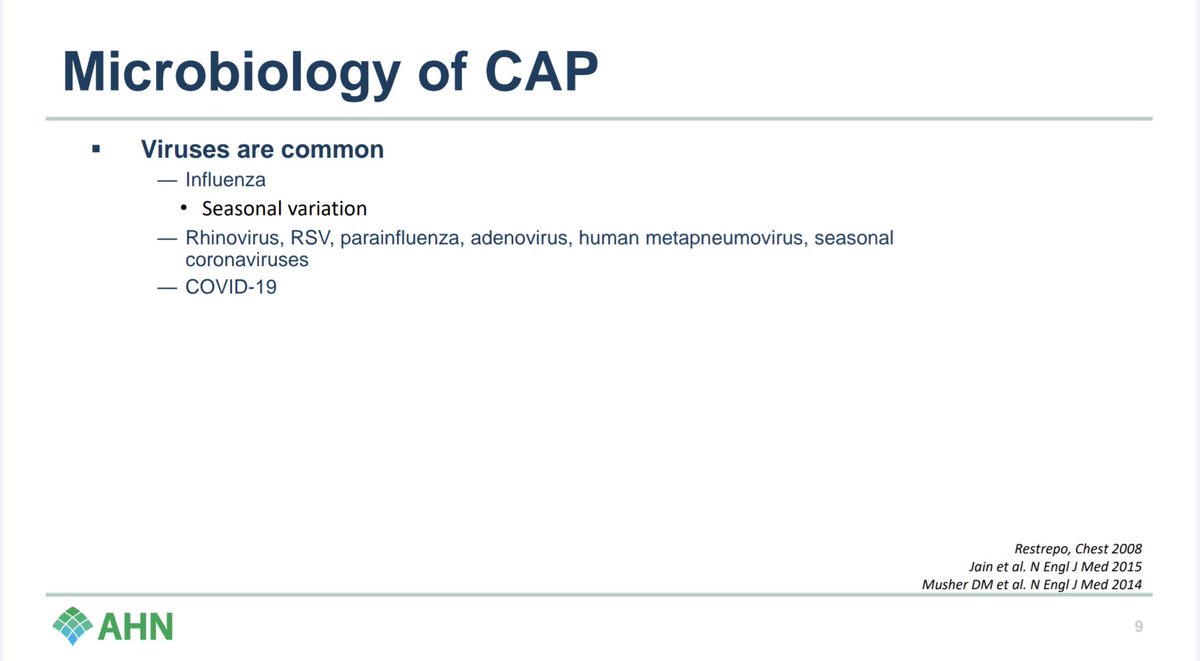
How long for Community Acquired Pneumonia?
5 days.
And maybe even shorter, we have RCT evidence for 3 days now too.
34/

5 days.
And maybe even shorter, we have RCT evidence for 3 days now too.
34/


If you want more on duration (and more entertainment), check out this talk from @matthewmof31
37/
https://twitter.com/matthewmof31/status/1571185548441620481?t=squndSxgY5gzbvK98n6Log&s=19
37/
Alright, that's it.
If you made it this far, thanks for reading.
Much of that isn't that "controversial," but it's the kind of stuff that comes up all the time in conversations and on rounds.
Hope some of it was useful.
#IDTwitter #MedTwitter
38/38
If you made it this far, thanks for reading.
Much of that isn't that "controversial," but it's the kind of stuff that comes up all the time in conversations and on rounds.
Hope some of it was useful.
#IDTwitter #MedTwitter
38/38
• • •
Missing some Tweet in this thread? You can try to
force a refresh