⚠️ TEN SECOND TRIAGE ⚠️
england.nhs.uk/publication/cl…
@NHSEngland have published the key training materials for #TenSecondTriage / #TST and MITT on their website (or sent it to your trust EPRR department)
🧵
/1
england.nhs.uk/publication/cl…
@NHSEngland have published the key training materials for #TenSecondTriage / #TST and MITT on their website (or sent it to your trust EPRR department)
🧵
/1

Users will be divided into:
Clinical Responders
🚑 🚁 🏥
or
Non-Clinical Responders
🚓 🚒
With specific materials available for each. The tool remains the same, but there are some subtle training nuances relevant to the various responsibilities of each user group
/2
Clinical Responders
🚑 🚁 🏥
or
Non-Clinical Responders
🚓 🚒
With specific materials available for each. The tool remains the same, but there are some subtle training nuances relevant to the various responsibilities of each user group
/2
Materials include:
1) High Res versions of the tool itself
2) PowerPoint presentation
3) Supplementary training material (acts as a trainer guide/presenter notes)
And this introductory video:
/3
1) High Res versions of the tool itself
2) PowerPoint presentation
3) Supplementary training material (acts as a trainer guide/presenter notes)
And this introductory video:
/3
This thread shall briefly summarise what I believe are the key nuances of the non-clinical responder approach to TST, using the uploaded ‘non-clinical responder’ presentation as an anchor point… for delivery, ensure to use the supplementary material relevant to your role
/4
/4
Firstly
TST is recommended as the first line triage tool for ***ALL*** at ***ANY*** multiple casualty incident
(small RTC or large high threat incident)
It allows all of us 🚑 🚓 🚒 to ensure:
1) Life Saving Interventions quickly
&
2) Extrication in priority order
/5
TST is recommended as the first line triage tool for ***ALL*** at ***ANY*** multiple casualty incident
(small RTC or large high threat incident)
It allows all of us 🚑 🚓 🚒 to ensure:
1) Life Saving Interventions quickly
&
2) Extrication in priority order
/5
It is designed to be natural & pragmatic…
If you watch @PoliceMedics deal with a multiple stabbing, they’ll prioritise those on the floor, manage any external bleeding, rapidly assess consciousness and search for any central penetrating injury (and report accordingly)
/6
If you watch @PoliceMedics deal with a multiple stabbing, they’ll prioritise those on the floor, manage any external bleeding, rapidly assess consciousness and search for any central penetrating injury (and report accordingly)
/6
Watch firefighters dealing with an RTC involving a van and an unconscious motorcyclist and they’ll prioritise the biker on the floor. They will manage any external bleeding, assess consciousness and open and maintain the airway
/6.5
/6.5
TST is designed to provide a simple framework, encouraging the rapid and repeated application of what we already know is the right thing to do in order to save life
(We also know it’s what people were likely to do in the real world anyway)
/7
(We also know it’s what people were likely to do in the real world anyway)
/7
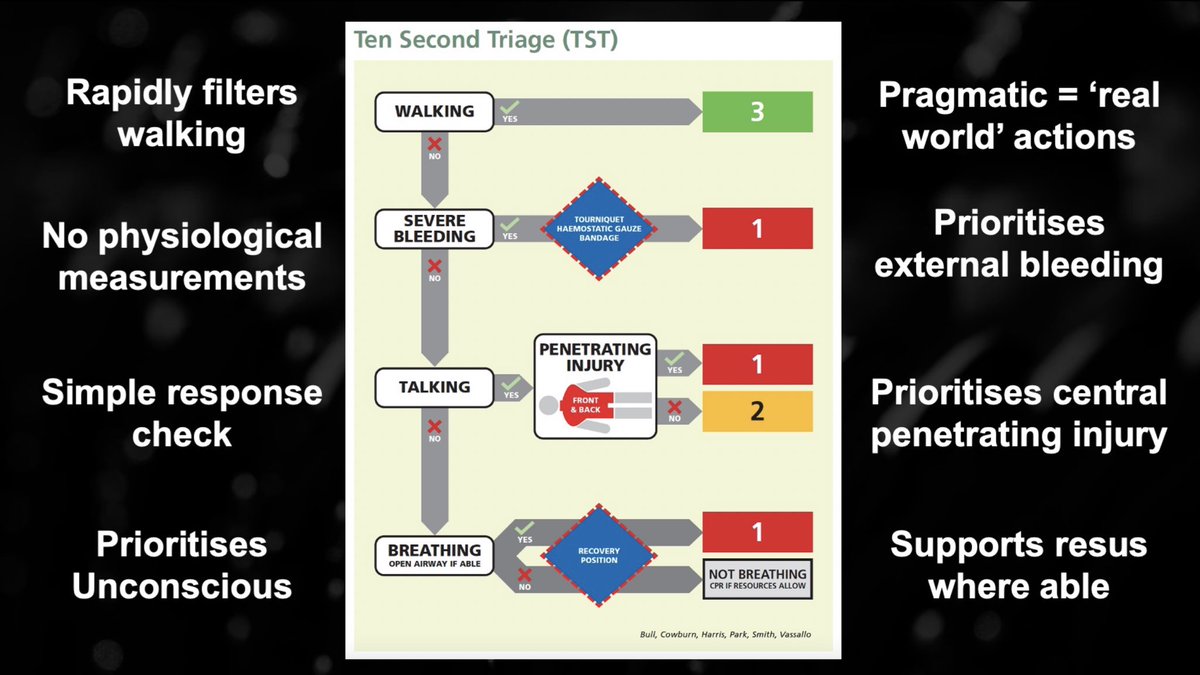
It quickly filters walking patients straight away (real world)
There are no physiological measurements (real world)
It prioritises the preventable causes of death and enables life saving interventions (save life)
It encourages resuscitation where appropriate (save life)
/8
There are no physiological measurements (real world)
It prioritises the preventable causes of death and enables life saving interventions (save life)
It encourages resuscitation where appropriate (save life)
/8
So. What are the life saving interventions?
- Direct *PRESSURE*
- Arterial *TOURNIQUETS*
- Junctional wound *PACKING*
- *AIRWAY MANAGEMENT*
/9
- Direct *PRESSURE*
- Arterial *TOURNIQUETS*
- Junctional wound *PACKING*
- *AIRWAY MANAGEMENT*
/9

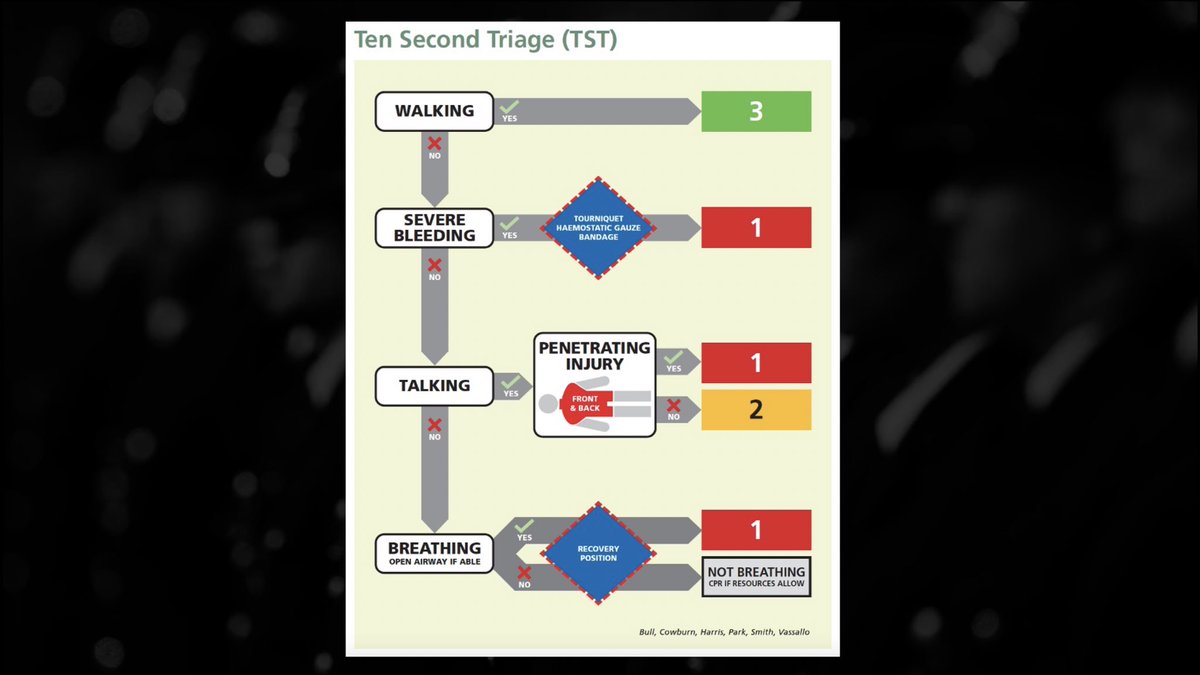
As with most triage systems/algorithms, TST has:
- Questions
- Answers
- Actions
- Triage Categories
/10
- Questions
- Answers
- Actions
- Triage Categories
/10
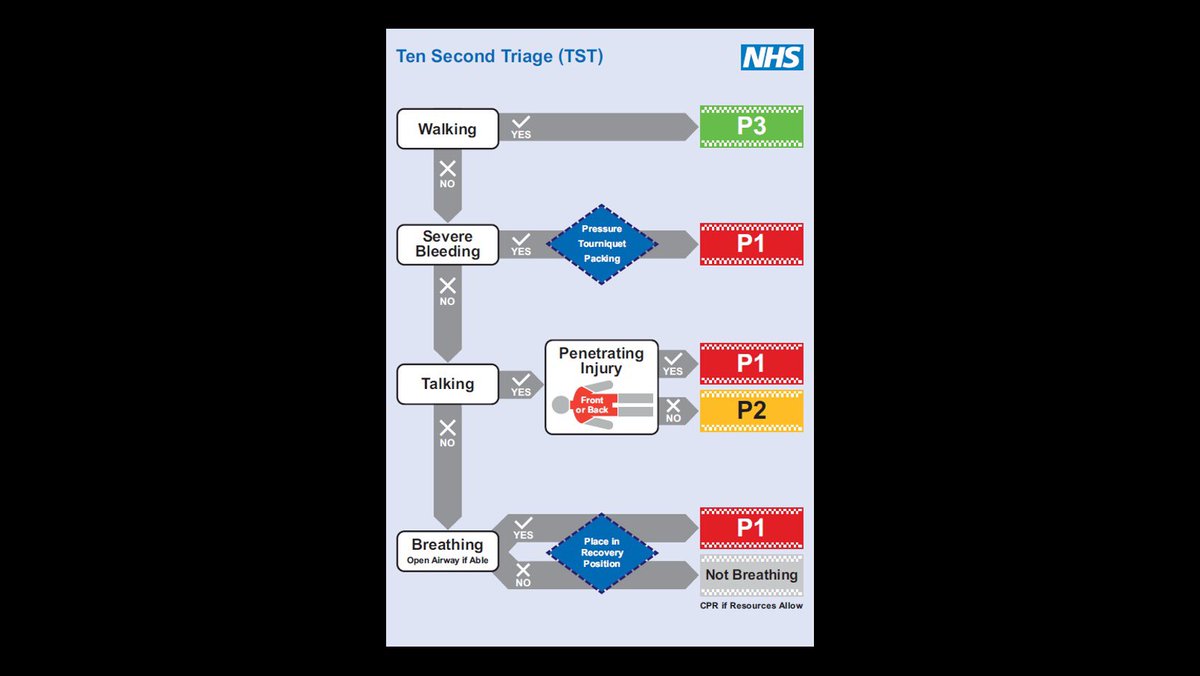
Let’s have a brief look at the actual TST algorithm
But! Be sure to read the supplementary material, as it really focuses in on the detail, the ‘what ifs’ and caveats of the whole process
england.nhs.uk/wp-content/upl…
/11
But! Be sure to read the supplementary material, as it really focuses in on the detail, the ‘what ifs’ and caveats of the whole process
england.nhs.uk/wp-content/upl…
/11
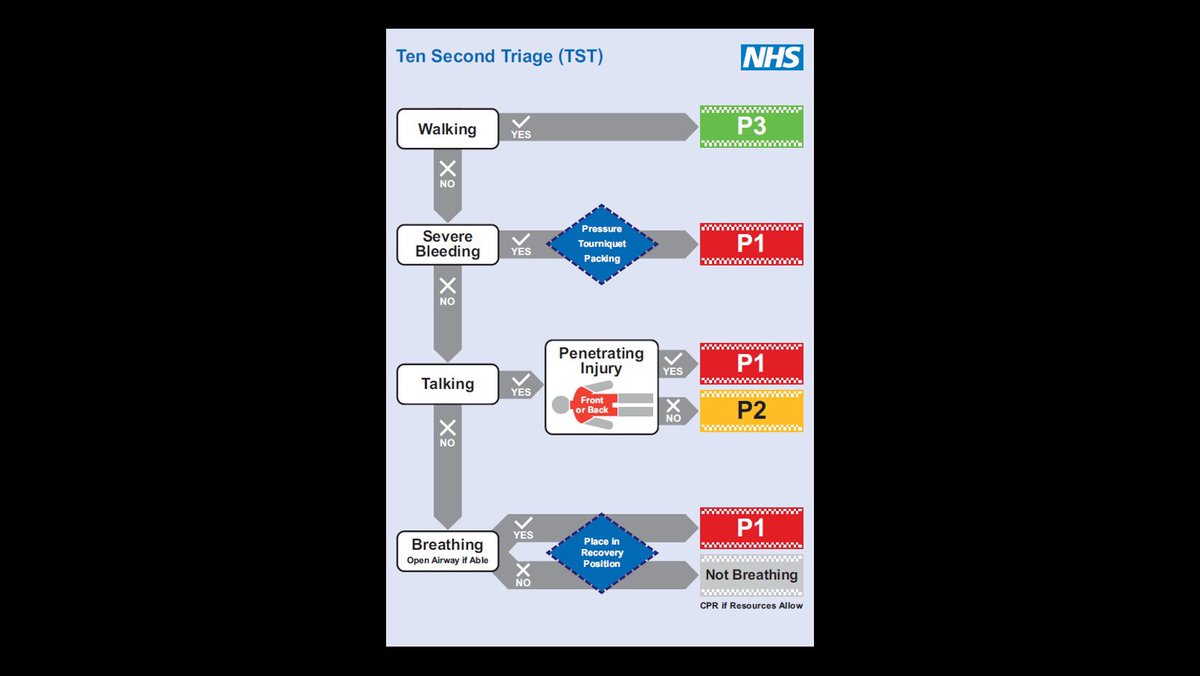
WALKING
This is intentionally filtered early, recognising pragmatic immediate actions, but for the first time acknowledges that not everyone can, will or should leave
In fact, we should consider how best to utilise those on scene to supplement our response @emedtox
/12
This is intentionally filtered early, recognising pragmatic immediate actions, but for the first time acknowledges that not everyone can, will or should leave
In fact, we should consider how best to utilise those on scene to supplement our response @emedtox
/12
and…
Not everyone who is walking is well
We shouldn’t routinely stop everyone on their feet, BUT if presented with a ‘walker’ with a critical injury then responders are emphatically encouraged to get involved
/13
Not everyone who is walking is well
We shouldn’t routinely stop everyone on their feet, BUT if presented with a ‘walker’ with a critical injury then responders are emphatically encouraged to get involved
/13

SEVERE BLEEDING
What about ‘catastrophic’ or ‘massive’!?
‘Severe’ is an intentional term. It lowers the threshold for intervention when indecision may be harmful
It hopefully broadsides the idea that life threatening bleeding must be pulsatile, spraying or up a wall
/14
What about ‘catastrophic’ or ‘massive’!?
‘Severe’ is an intentional term. It lowers the threshold for intervention when indecision may be harmful
It hopefully broadsides the idea that life threatening bleeding must be pulsatile, spraying or up a wall
/14
The interventions shouldn’t be a surprise
Pressure. Not to be sniffed at and if it’s all you’ve got - it will be life saving
Tourniquets. Yes. Limbs. Use them
Packing. For junctions. Indifferent about ‘what with’ due to broad capabilities within this group
/15
Pressure. Not to be sniffed at and if it’s all you’ve got - it will be life saving
Tourniquets. Yes. Limbs. Use them
Packing. For junctions. Indifferent about ‘what with’ due to broad capabilities within this group
/15
TALKING
I personally think this is pretty slick…
Are they talking?
Are they talking normally?
No?
Then they are probably quite sick
What about kids that are too young to talk (<2yrs)?
They are hard to assess and risky to get wrong, let’s prioritise them regardless
/16
I personally think this is pretty slick…
Are they talking?
Are they talking normally?
No?
Then they are probably quite sick
What about kids that are too young to talk (<2yrs)?
They are hard to assess and risky to get wrong, let’s prioritise them regardless
/16
PENETRATING INJURY
Non-compressible torso injury should be the preventable cause of death that we all lose sleep over
It cannot be effectively managed out of hospital so we should prioritise it accordingly
Check the front, back, neck, collars, armpits, groin and buttocks
/17
Non-compressible torso injury should be the preventable cause of death that we all lose sleep over
It cannot be effectively managed out of hospital so we should prioritise it accordingly
Check the front, back, neck, collars, armpits, groin and buttocks
/17

Any central penetrating injury = P1
Note - there is no prompt for chest seals
Good pieces of kit, but only designed to temporise open pneumothoraces (rare & slow)
No benefit in the dreaded non-compressible torso injury (common & fast)
/18
Note - there is no prompt for chest seals
Good pieces of kit, but only designed to temporise open pneumothoraces (rare & slow)
No benefit in the dreaded non-compressible torso injury (common & fast)
/18
Chest Seals are not in the same league of life saving interventions as bleeding or airway management
Useful, but not immediately. We need to provide them within our system, but our main priorities are clear:
-Stop bleeding
-Open airways
-Prioritise non-compressible torso
/19
Useful, but not immediately. We need to provide them within our system, but our main priorities are clear:
-Stop bleeding
-Open airways
-Prioritise non-compressible torso
/19
BREATHING
(With an open airway)
Yes or No
Yes - Sick
No - Identify them as ‘Not Breathing’ and consider what happens next
Trainers and users - I beg of you to read the supplemental materials, this is a professional, humanitarian and clinically appropriate change.
/20
(With an open airway)
Yes or No
Yes - Sick
No - Identify them as ‘Not Breathing’ and consider what happens next
Trainers and users - I beg of you to read the supplemental materials, this is a professional, humanitarian and clinically appropriate change.
/20
The days of apnoea+triage = DEAD are over
TST is recommend for all scales and types of incidents, static or dynamic
“CPR if resources allow” or 3/4 prone is the right thing to do
Decisions regarding death should not be made without appropriate consideration
/21
TST is recommend for all scales and types of incidents, static or dynamic
“CPR if resources allow” or 3/4 prone is the right thing to do
Decisions regarding death should not be made without appropriate consideration
/21
How big is the scene? How many casualties, responders, bystanders? How far into it are we?
Bad end of the scale = moving on
Good end = resus
The area in the middle allows us to make real-time decisions, empowering us to undertake scaled positive action until help arrives
/22
Bad end of the scale = moving on
Good end = resus
The area in the middle allows us to make real-time decisions, empowering us to undertake scaled positive action until help arrives
/22
Baring in mind this thread is aimed at ‘non-clinical responders’ it’s worth mentioning what happens next
Healthcare resources share the same key priorities during TST
1) Life Saving Interventions
2) Prioritised Evacuation
/23
Healthcare resources share the same key priorities during TST
1) Life Saving Interventions
2) Prioritised Evacuation
/23
They also have an additional third…
3) Re-assessment of ‘Not Breathing’ casualties
Where a casualty is considered to be amenable to resus, they can be retriaged as P1 and managed accordingly
If after appropriate consideration = futility, they can be recognised as dead
/24
3) Re-assessment of ‘Not Breathing’ casualties
Where a casualty is considered to be amenable to resus, they can be retriaged as P1 and managed accordingly
If after appropriate consideration = futility, they can be recognised as dead
/24
Nearly there! The cognitive short-cuts 🧠 are a nod to ‘System 1’ thinking
P1 by clinical presentation:
- Severe Bleeding
- Penetrating Injury to torso
- Impaired consciousness
P1 by intervention:
- Pressure, TQ, Packing
- What would have normally got a chest seal
- Airway
/25
P1 by clinical presentation:
- Severe Bleeding
- Penetrating Injury to torso
- Impaired consciousness
P1 by intervention:
- Pressure, TQ, Packing
- What would have normally got a chest seal
- Airway
/25
Phew!
Again, please make sure to head to england.nhs.uk/publication/cl… to get hold of the key material yourself
Sean.harris4@nhs.net
/end
Again, please make sure to head to england.nhs.uk/publication/cl… to get hold of the key material yourself
Sean.harris4@nhs.net
/end
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter