What do inkblots and puppies hugging teach us about the way the long tracts are organized in the spinal cord? Everything.
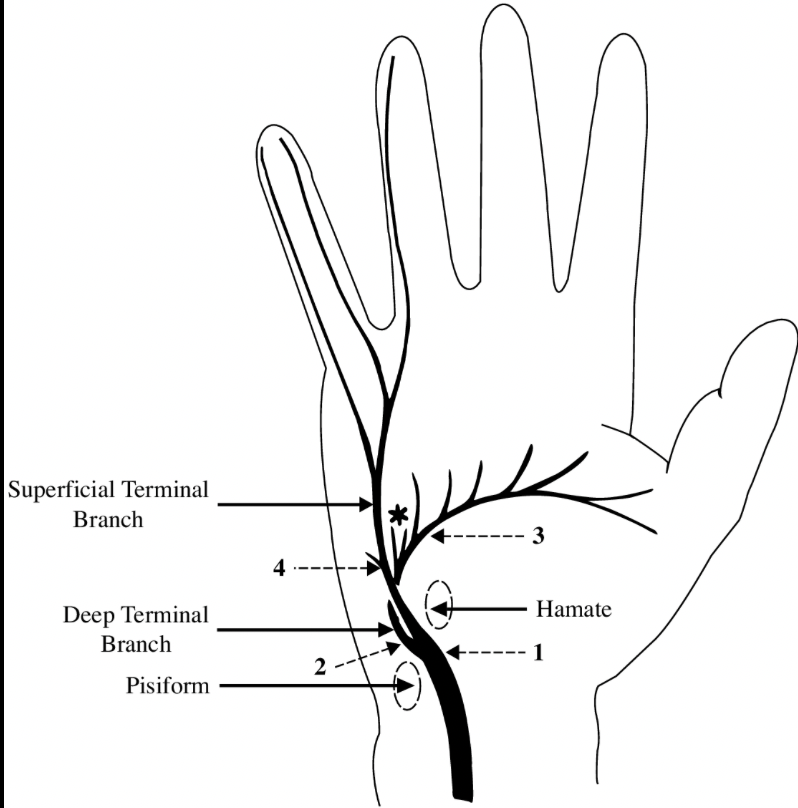
Behold, our favorite tracts in the cervical cord.
A = fibers to/from the arm
T = fibers to/from the trunk
L = fibers to/from the leg
#tweetorial
1/7
Behold, our favorite tracts in the cervical cord.
A = fibers to/from the arm
T = fibers to/from the trunk
L = fibers to/from the leg
#tweetorial
1/7
Now let's just look at the arm fibers. For all three tracts, they are right up against the grey matter.
Want a #mnemonic to help you remember that?
2/7
Want a #mnemonic to help you remember that?
2/7

Well, some say the grey matter looks like a butterfly.
You love butterflies, so what do you do when we see one? You hug it.
That's why your arm fibers are right up in there. For butterfly hugs.
3/7
You love butterflies, so what do you do when we see one? You hug it.
That's why your arm fibers are right up in there. For butterfly hugs.
3/7

But wait, an actual hug would crush a butterfly, wouldn't it? Good point.
(Had a picture of a squashed butterfly here, but I redacted it because it was too disturbing.)
Imagine instead that the grey matter is a beagle. A proud, noble beagle, who has been a very good boy. 4/7
(Had a picture of a squashed butterfly here, but I redacted it because it was too disturbing.)
Imagine instead that the grey matter is a beagle. A proud, noble beagle, who has been a very good boy. 4/7

One possible implication of this organization is that external compression of the cord may present with ascending symptoms, as the most lateral fibers are damaged first.
That's why someone with a C-spine lesion may present only with lower extremity symptoms.
6/7
That's why someone with a C-spine lesion may present only with lower extremity symptoms.
6/7

So next the psychologist asks you what you see in this inkblot, just say, "Something that spurs me to activate my medial descending corticospinal fibers as gently as possible so as not to damage the fragile little anterior horns."
And then see what diagnosis they give you!
7/7
And then see what diagnosis they give you!
7/7

• • •
Missing some Tweet in this thread? You can try to
force a refresh