Intro:
TMA syndromes are extraordinarily diverse❗️
They may be
-hereditary or acquired
-occur in children and adults
-onset can be sudden or gradual
BUT
despite their diversity, they are united by common, defining clinical and pathological features
2/16
TMA syndromes are extraordinarily diverse❗️
They may be
-hereditary or acquired
-occur in children and adults
-onset can be sudden or gradual
BUT
despite their diversity, they are united by common, defining clinical and pathological features
2/16
Features:
-Thrombopenia
👉platelet aggregation & thrombi
-microangiopathic haemolytic anaemia (MAHA)
👉RBC fragmentation (schistocytes)
-end organ damage
-LDH⬆️
👉tissue ischemia & cell lysis
-haptoglobin⬇️
👉binds to free Hb, hemolysis
-Coombs generally negative, PT/aPTT⬇️
4/16
-Thrombopenia
👉platelet aggregation & thrombi
-microangiopathic haemolytic anaemia (MAHA)
👉RBC fragmentation (schistocytes)
-end organ damage
-LDH⬆️
👉tissue ischemia & cell lysis
-haptoglobin⬇️
👉binds to free Hb, hemolysis
-Coombs generally negative, PT/aPTT⬇️
4/16

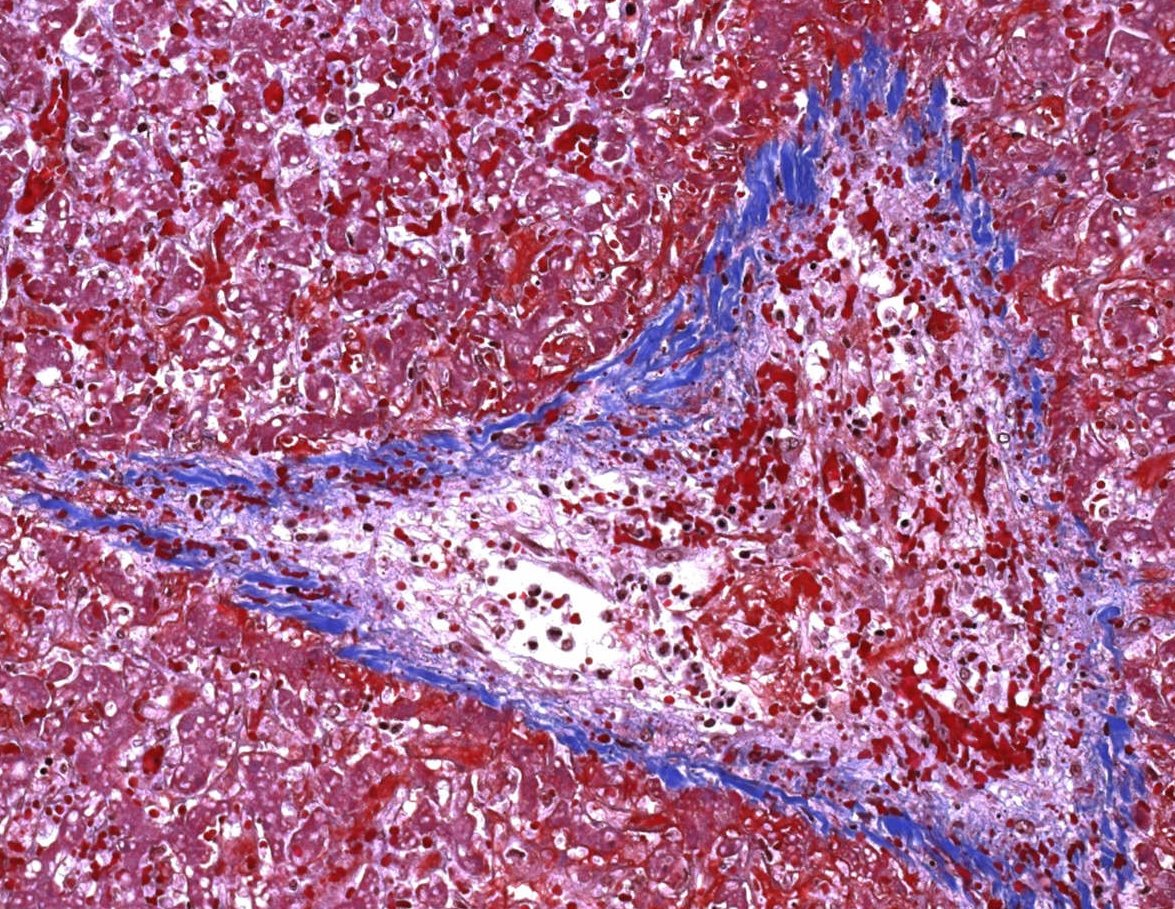
Pathology:
-For all primary TMA syndromes the same
- -renal arteriole occlusion with endotheliosis as well as lumen and vessel-wall fibrin
- -Proliferation in the myocyte layer (“onion skinning”) may also be present
5/16
-For all primary TMA syndromes the same
- -renal arteriole occlusion with endotheliosis as well as lumen and vessel-wall fibrin
- -Proliferation in the myocyte layer (“onion skinning”) may also be present
5/16

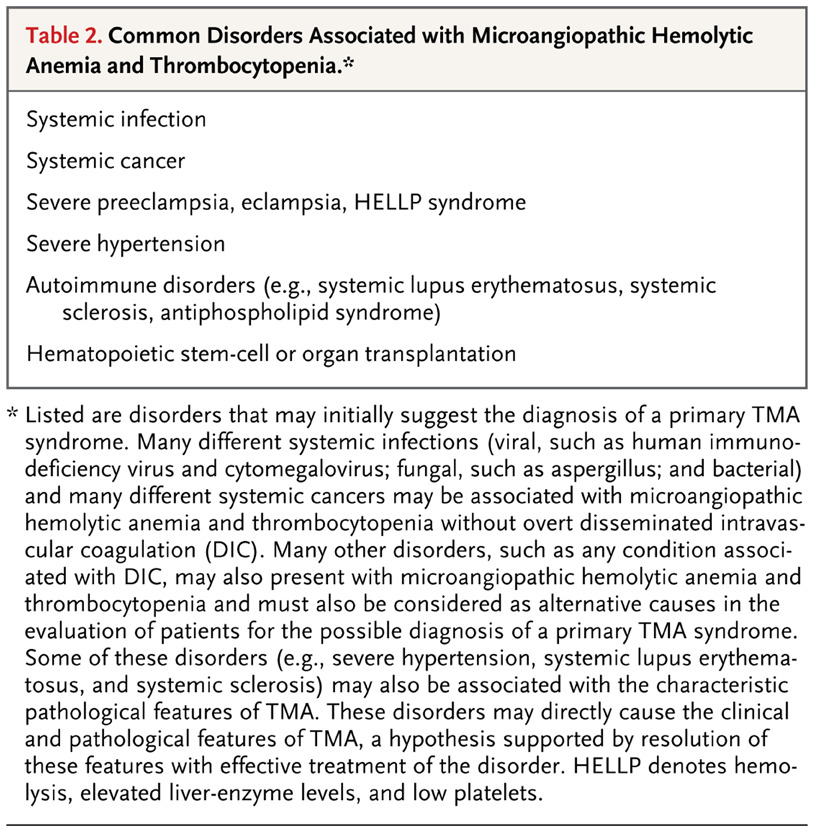
Think first before you act:
Before you start sophisticated lab tests and hypotheses, exclude common causes of MAHA and thrombocytopenia❗️
Remember, any condition associated with DIC can occur with MAHA and thrombocytopenia
👉rule out first
6/16
Before you start sophisticated lab tests and hypotheses, exclude common causes of MAHA and thrombocytopenia❗️
Remember, any condition associated with DIC can occur with MAHA and thrombocytopenia
👉rule out first
https://twitter.com/NicoGagelmann/status/1659249797864226823?s=20
6/16
Evaluate MAHA and thrombopenia:
-severity of kidney injury as distinguishing feature
-severe acute kidney injury
👉consider complement-mediated (acquired/hereditary)
-idiopathic disease in + 20%
-TTP is also called ADAMTS13 deficiency–mediated TMA
7/16
-severity of kidney injury as distinguishing feature
-severe acute kidney injury
👉consider complement-mediated (acquired/hereditary)
-idiopathic disease in + 20%
-TTP is also called ADAMTS13 deficiency–mediated TMA
7/16

Thrombotic thrombocytopenic purpura:
-rare systemic form of TMA
👉severe deficiency in ADAMTS13
👉disintegrin + metalloprotease with thrombospondin type 1 motif 13, which cleaves von Willebrand factor
For more, I refer to the legend @nihardesai7
8/16
-rare systemic form of TMA
👉severe deficiency in ADAMTS13
👉disintegrin + metalloprotease with thrombospondin type 1 motif 13, which cleaves von Willebrand factor
For more, I refer to the legend @nihardesai7
https://twitter.com/nihardesai7/status/1467368223142080512?s=20
8/16

Complement-mediated aHUS:
-0.4 cases per Mio per year
-acquired or inherited defects in the alternative pathway
-Extra-renal manifestations in 10-20%
-AKI more prominent than in TTP
-Genetic screening (CFH, CFI, C3, CFB, CD46, CFHR1) is essential, incl DGKE & MMACHC
9/16
-0.4 cases per Mio per year
-acquired or inherited defects in the alternative pathway
-Extra-renal manifestations in 10-20%
-AKI more prominent than in TTP
-Genetic screening (CFH, CFI, C3, CFB, CD46, CFHR1) is essential, incl DGKE & MMACHC
9/16

Shigatoxin-associated TMA:
-most common form, mainly occurring in children <5 years
-accounts for 90% of cases of HUS in children
-transmission
👉undercooked meat, unpasteurised dairy produce, direct contact, ingesting contaminated🥦🍅
-majority is self-limiting
10/16
-most common form, mainly occurring in children <5 years
-accounts for 90% of cases of HUS in children
-transmission
👉undercooked meat, unpasteurised dairy produce, direct contact, ingesting contaminated🥦🍅
-majority is self-limiting
10/16

Pregnancy-associated TMA:
-Pregnancy + postpartum high-risk periods for TTP and complement-mediated aHUS❗️
-typically in the 2nd + 3rd trimesters
-cause: maybe VWF production⬆️
-experience of caplacizumab limited
For more👉legend @nihardesai7
11/16
-Pregnancy + postpartum high-risk periods for TTP and complement-mediated aHUS❗️
-typically in the 2nd + 3rd trimesters
-cause: maybe VWF production⬆️
-experience of caplacizumab limited
For more👉legend @nihardesai7
11/16
https://twitter.com/nihardesai7/status/1589281532992450560?s=20
Transplant-associated (TA-) TMA:
-high mortality❗️
-etiology is myriad
-~8% of BMT patients
-historically, plasma exchange was mainstay of treatment
BUT
-with recognition that ADAMTS13 levels in TA-TMA are mostly normal, strategies have shifted away from this approach
12/16
-high mortality❗️
-etiology is myriad
-~8% of BMT patients
-historically, plasma exchange was mainstay of treatment
BUT
-with recognition that ADAMTS13 levels in TA-TMA are mostly normal, strategies have shifted away from this approach
12/16

TA-TMA treatment:
-Elucidation of complement in development of TA-TMA shifted treatment toward terminal complement inhibition with eculizumab and MASP-2 inhibition with narsoplimab
-Prospective data on eculizumab still limited to children
-more evidence needed
13/16
-Elucidation of complement in development of TA-TMA shifted treatment toward terminal complement inhibition with eculizumab and MASP-2 inhibition with narsoplimab
-Prospective data on eculizumab still limited to children
-more evidence needed
13/16

Narsoplimab for TA-TMA:
-IV once weekly for 4-8 weeks
-Response rate: 61%, similar across subgroups
-Improvement in organ function in 74%
-100-day survival after TA-TMA diagnosis was 94% in responders
14/16
-IV once weekly for 4-8 weeks
-Response rate: 61%, similar across subgroups
-Improvement in organ function in 74%
-100-day survival after TA-TMA diagnosis was 94% in responders
14/16

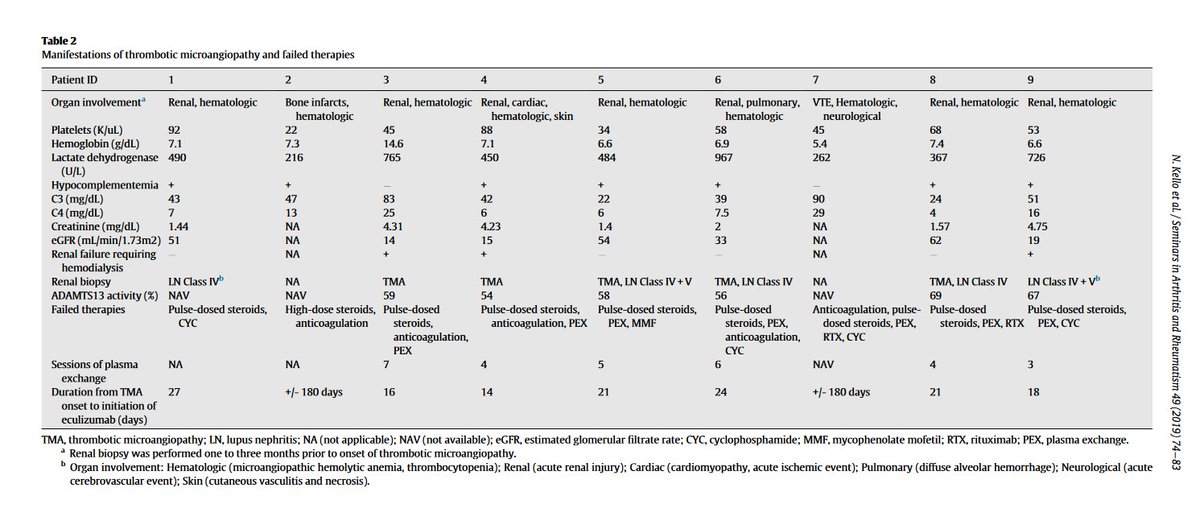
Autoimmune TMA:
-SLE, scleroderma renal crisis or catastrophic antiphospholipid syndrome (CAPS)
-Case reports describe use of eculizumab in SLE-TMA
-~30% of CAPS show renal TMA with 36% morality 👉glucocorticoids, anticoagulants + IVIG
For more👉legend @PanktiMehta24
15/16
-SLE, scleroderma renal crisis or catastrophic antiphospholipid syndrome (CAPS)
-Case reports describe use of eculizumab in SLE-TMA
-~30% of CAPS show renal TMA with 36% morality 👉glucocorticoids, anticoagulants + IVIG
For more👉legend @PanktiMehta24
15/16
Summary of TMA:
❗️Array of manifestations, CHALLENGING
❗️High morbidity + mortality
❗️Renal involvement is common
❗️Suspect: MAHA, thrombopenia
❗️rule out other causes
❗️rapid assessment, diagnosis + treatment essential
❗️TA-TMA very serious
❗️Eculizumab, narsoplimab new options
❗️Array of manifestations, CHALLENGING
❗️High morbidity + mortality
❗️Renal involvement is common
❗️Suspect: MAHA, thrombopenia
❗️rule out other causes
❗️rapid assessment, diagnosis + treatment essential
❗️TA-TMA very serious
❗️Eculizumab, narsoplimab new options
References and resources:
nejm.org/doi/10.1056/NE…
onlinelibrary.wiley.com/doi/10.1111/ij…
nature.com/articles/s4158…
sciencedirect.com/science/articl…
aerzteblatt.de/int/archive/ar…
pubmed.ncbi.nlm.nih.gov/35439028/
nejm.org/doi/10.1056/NE…
onlinelibrary.wiley.com/doi/10.1111/ij…
nature.com/articles/s4158…
sciencedirect.com/science/articl…
aerzteblatt.de/int/archive/ar…
pubmed.ncbi.nlm.nih.gov/35439028/
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter