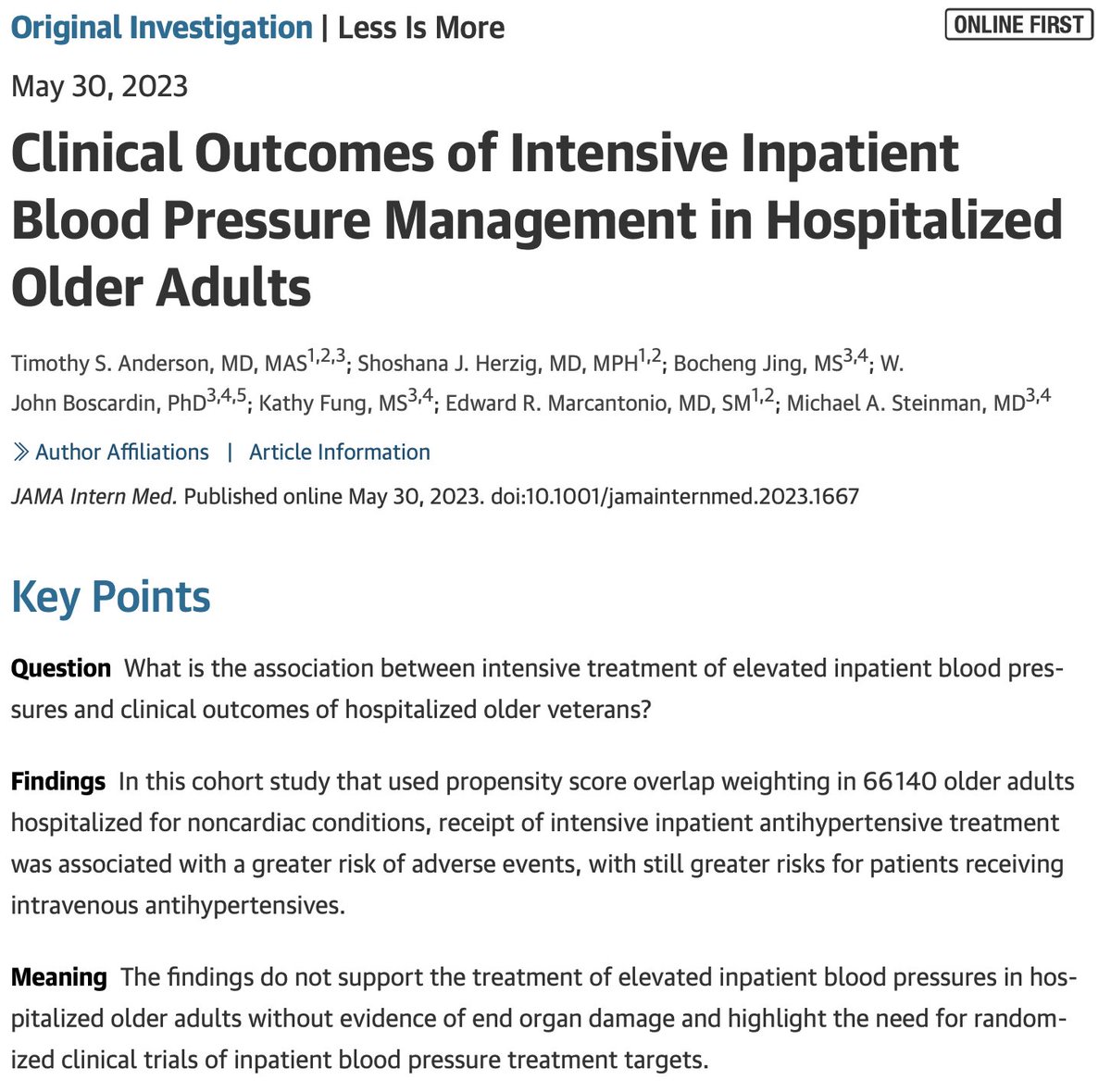
🚨New #Hypertension Paper in @JAMAInternalMed 🚨
Time for a Thread...
Link: jamanetwork.com/journals/jamai…
Time for a Thread...
Link: jamanetwork.com/journals/jamai…
The topic of managing chronic conditions & chronic medications in the hospital is a long-term interest of our group (prescribingwiselylab.org)
Why?
Why?

For starters, we check BP in the hospital all the time!
Mostly in an effort to detect low BPs.
Yet BPs fluctuate & most patients will have some high BPs during a 🏥stay.
Many causes: physiologic stress, meds, poor measurement, true hypertension & so on.
Mostly in an effort to detect low BPs.
Yet BPs fluctuate & most patients will have some high BPs during a 🏥stay.
Many causes: physiologic stress, meds, poor measurement, true hypertension & so on.
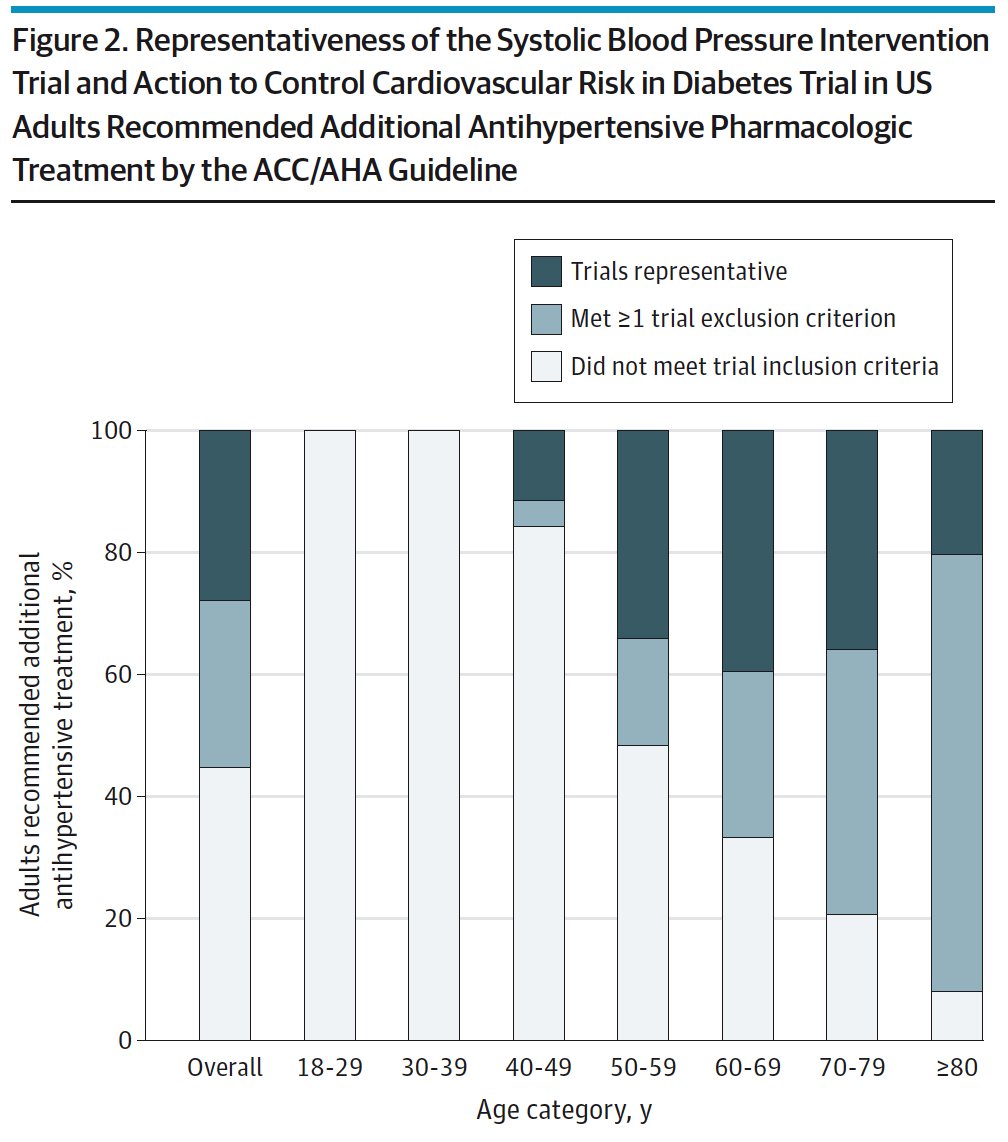
Presumably we treat high BPs to reduce the risk of CV events, applying outpatient evidence.
But in the clinic, the time to benefit from BP lowering is measured in months not hours.
Acutely lowering BP might lead to harm, particularly if BPs are lowered too far or too fast...
But in the clinic, the time to benefit from BP lowering is measured in months not hours.
Acutely lowering BP might lead to harm, particularly if BPs are lowered too far or too fast...
There is no randomized controlled trial data on managing BP in the hospital.
We don’t even know what a “good” BP for an acutely ill hospitalized patient is.
This is a conundrum as we don't treat asymptomatic sinus tachycardia in 🏥patients but we often do treat high BPs.
We don’t even know what a “good” BP for an acutely ill hospitalized patient is.
This is a conundrum as we don't treat asymptomatic sinus tachycardia in 🏥patients but we often do treat high BPs.
Without trials or guidelines, there is wide practice variation.
With some high BPs treated with intermittent IV 💉meds , some with new daily oral 💊, and some untreated.
With some high BPs treated with intermittent IV 💉meds , some with new daily oral 💊, and some untreated.
The ideal trial might assign patients to a high vs low inpatient BP targets (like SPRINT) but this is difficult to replicate retrospectively.
Nonetheless, practice heterogeneity gives us a chance to study outcomes, doing our best to emulate a clinical trial.
Nonetheless, practice heterogeneity gives us a chance to study outcomes, doing our best to emulate a clinical trial.
Using national @DeptVetAffairs health system data we created a cohort of ~66,000 older adults hospitalized for conditions not typically related to BP.
We classified patients with high BPs in the first 2 days of by whether or not they received new BP treatments.
We classified patients with high BPs in the first 2 days of by whether or not they received new BP treatments.
We assumed patients receiving BP treatment in the first 48 hours would continue to receive intensive treatment during hospitalization; an assumption that seems to have held out: 

We measured lots of variables and used overlap weighting to deal with measured confounding
We then assessed clinical outcomes in the remaining hospitalization period (beyond 48 hours) focused on outcomes plausibly related to BP…..
We then assessed clinical outcomes in the remaining hospitalization period (beyond 48 hours) focused on outcomes plausibly related to BP…..
Signals of harm were stronger in patients who received IV meds 💉
Associations were consistent across a variety of CV and geriatric subgroups and varying model specifications
Associations were consistent across a variety of CV and geriatric subgroups and varying model specifications

So is the case of what to do with high BP in the hospital settled?
Should we simply ignore it?
Should we simply ignore it?
This paper builds on studies from our group & others (@lama_ghazi @MRothbergMD) which consistently find no benefit from acute inpatient BP tx.
jamanetwork.com/journals/jamai…
bmj.com/content/362/bm…
jamanetwork.com/journals/jamai…
ahajournals.org/doi/10.1161/HY…
journals.lww.com/jhypertension/…
jamanetwork.com/journals/jamai…
bmj.com/content/362/bm…
jamanetwork.com/journals/jamai…
ahajournals.org/doi/10.1161/HY…
journals.lww.com/jhypertension/…
All of these studies are retrospective observational studies and at very real risk of selection bias / confounding by indication.
At this point, enough observational studies, randomized trials are needed.
This will be quite challenging (I’d love to find partners in this work)
At this point, enough observational studies, randomized trials are needed.
This will be quite challenging (I’d love to find partners in this work)
In the meantime, for clinicians, there is certainly clinical nuance here, but we propose two guiding principles: Avoiding IV treatment & focusing on managing underlying causes of high BP, not just treating the numbers. 

In @AnnalsofIM, @WrayCharles and I have written more about this clinical dilemma & have proposed a framework for hospitalists and trainees:
acpjournals.org/doi/10.7326/M2…?
(Great for rounding!)
acpjournals.org/doi/10.7326/M2…?
(Great for rounding!)
Team effort – championed by my long-term mentor @MikeSteinman & @BIDMC_Medicine mentors @ShaniHerzig @MarcantonioEd
& generously supported by @NIHAging over the past 5 years.
/END
& generously supported by @NIHAging over the past 5 years.
/END
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter