Thank you @jvipondmd for your impassioned presentation yesterday & the stimulating conversation at dinner. Your contribution to saving people & the planet by doing things right is inspiring.
👏👏👏



👏👏👏




Thank you Hospital Engineers for sharing your expertise to prevent infections during hospital construction.
Thank you for all you do to keep patients safe in all of our healthcare facilities all of the time.
Thank you for supporting @IPACCanada!
@CHES_SCISS

Thank you for all you do to keep patients safe in all of our healthcare facilities all of the time.
Thank you for supporting @IPACCanada!
@CHES_SCISS


Thank you Dr. Kowalski for your very detailed technical brief on UV.
It was fascinating to see the impact of genomics, orientation & medium on efficacy.
And it was thought provoking to see the modeling that shows UV could reduce COVID case waves by 98%.
@Sanuvox



It was fascinating to see the impact of genomics, orientation & medium on efficacy.
And it was thought provoking to see the modeling that shows UV could reduce COVID case waves by 98%.
@Sanuvox




Thank you @EdRubinstein for teaching us that Infection Prevention & Sustainability are not in tension - in fact implementing things like reusables & sophisticated engineered systems are key to both.
👏👏👏

👏👏👏


Thank you Dr. Titus Wong for your courage & insight to lead BC IPC in researching & implementing Engineered Infection Prevention solutions into Healthcare Facilties & mass transit.
mining.einnews.com/amp/pr_news/63…
mining.einnews.com/amp/pr_news/63…

Thank you, Dr Klompas, for encouraging us to challenge Dogma and to accept new paradigms as the evidence presents itself.
Thank you clearly laying out your personal journey to switch from "Droplet" to "Airborne" paradigm for SARS2 transmission.
👏👏👏
Thank you clearly laying out your personal journey to switch from "Droplet" to "Airborne" paradigm for SARS2 transmission.
👏👏👏

Thank you to @CanadamasQ, Swenco Medical, @PADMmedical @CAPPEM2 for donating Made in 🇨🇦 respirators & plant based medical masks to conference attendees.
👏👏👏

👏👏👏


Thank you @VicLeungIDdoc for teaching us about C auris.
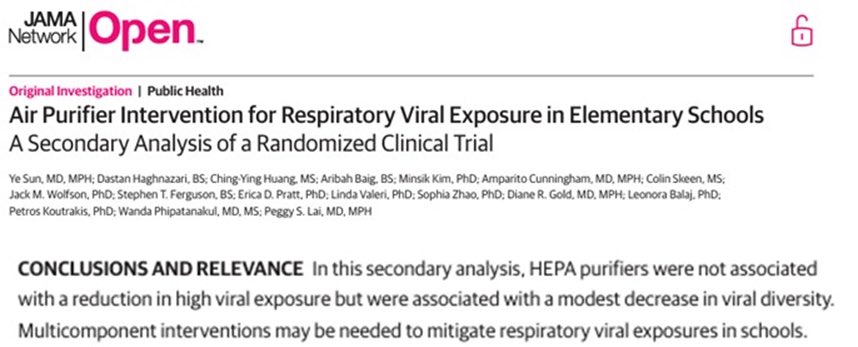
Thank you as well for your extraordinary leadership throughout the pandemic - teaching about airborne transmission, adding air purifiers to patient rooms, & moving vulnerable LTC residents into better ventilated spaces.

Thank you as well for your extraordinary leadership throughout the pandemic - teaching about airborne transmission, adding air purifiers to patient rooms, & moving vulnerable LTC residents into better ventilated spaces.


Many thanks to @keithmcglone55 for doing an excellent job on the Scientific Committee & for his professional moderation of many sessions.
👏👏👏
👏👏👏

Thank you to Kelli & Heather & Carly & all the organizers for a great conference.
A special thank you to Gerry, for her unwavering commitment to IPAC, to patients, to industry partners, to collaboration, to professionalism, to progress, & to always doing the right thing right.
A special thank you to Gerry, for her unwavering commitment to IPAC, to patients, to industry partners, to collaboration, to professionalism, to progress, & to always doing the right thing right.
It was great to catch up with so many ppl after 3 years.
It feels like such a privilege now, the things we took for granted before.
The renewed spirit was palpable & energizing.
It feels like such a privilege now, the things we took for granted before.
The renewed spirit was palpable & energizing.
I especially want to thank everyone who showed such keen interest & enthusiasm for Engineered Infection Prevention technologies & better masks & respirators Made in 🇨🇦.
You've certainly renewed my optimism for a better healthcare future & for that I can't thank you enough. ☺️
You've certainly renewed my optimism for a better healthcare future & for that I can't thank you enough. ☺️
• • •
Missing some Tweet in this thread? You can try to
force a refresh