1/n young adult presents to the ED with weakness, fatigue & LE edema. Cr 2.8 (base 1.0). Reports tarry stools. Initial clinical impression: ischemic ATN 2/2 GIB. #UrineMicroscopy is performed: crisp RBC casts and acanthocytes are identified in #UrinarySediment. Time to regroup. 



2/n pt had a bioprosthetic pulmonic valve from a remote tetralogy of Fallot repair. Radar now centered in the connection between heart valve disease and endocarditis-associated glomerulonephritis (SBE-GN). A transthoracic echocardiogram: no vegetations, no valvular insufficiency
3/n as part of the nephritic work up, PR3 returns with low titer positivity. Primary AAV? Actually, that finding strengthened the case for SBE-GN since it’s known that 20-40% of them are PR3+ link.springer.com/content/pdf/10… this @arkanalabs @renalpathdoc review is a must read 



4/n so, we suggest obtaining TEE. However TTE is deemed OK to visualize pulmonic valve. And no fever, no bacteremia thus far, so no TEE…
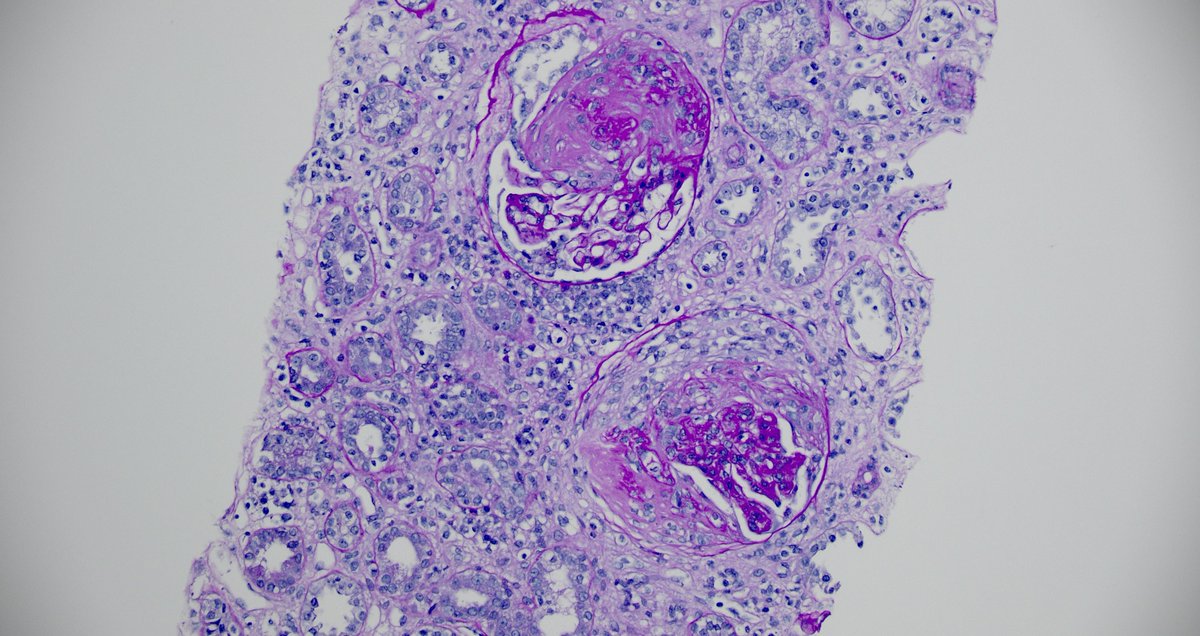
4/n the next day, pt spikes a fever, the following day, MRSA grows in one (1/6) blood culture. The story starts to build. A kidney biopsy is performed: pauci immune (only 1+ IgM) crescentic necrotizing non-proliferative GN. Morphologically, classic features of ANCA-mimic SBE-GN 




5/n so, MRSA coverage is started w/vanco (switched 2 dapto later due to AKI). Cr 3.2-3.4. All good? Wait, Staph-associated infective GNs tend to b IgA dominant, maybe C3 dominant. Pauci immune is <common. On the other hand after, Staph & Strep, 3rd most common bug: Bartonella sp 

6/n numerous case reports of PR3+ SBE-GN associated with Bartonella. Learned it years back with a case of a pacemaker wire infection. A couple of other cases here pubmed.ncbi.nlm.nih.gov/36158150/ pubmed.ncbi.nlm.nih.gov/30210883/
7/n another look at the #UrinarySediment, RBC casts all over, and waxy casts that seemed to originate from degraded RBC casts, no granular casts. 







8/n other RBC casts with fibrinous matrix are also found (see latest @jrseltzer post on @RenalFellowNtwk) and mixed WBC/RBC casts, highly consistent with the subsequent kidney biopsy findings. 







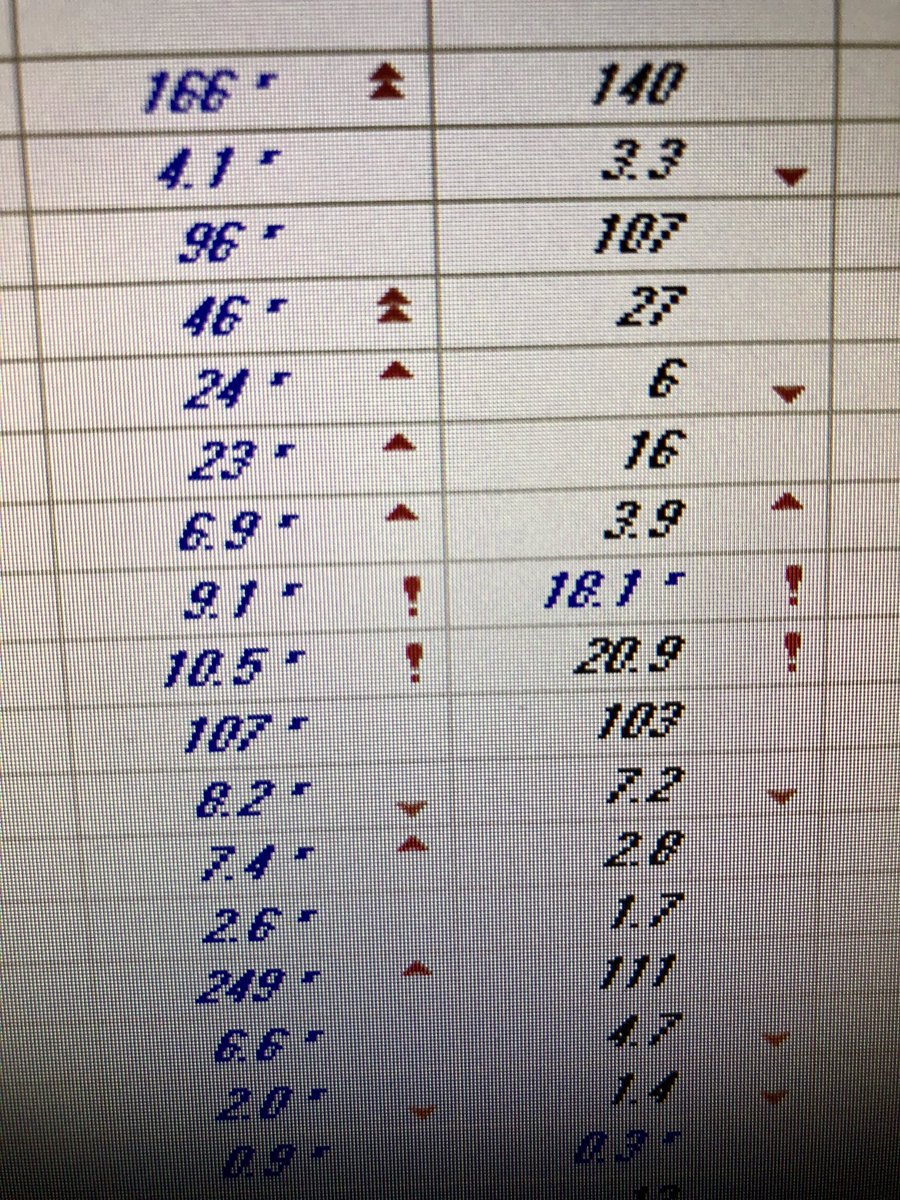
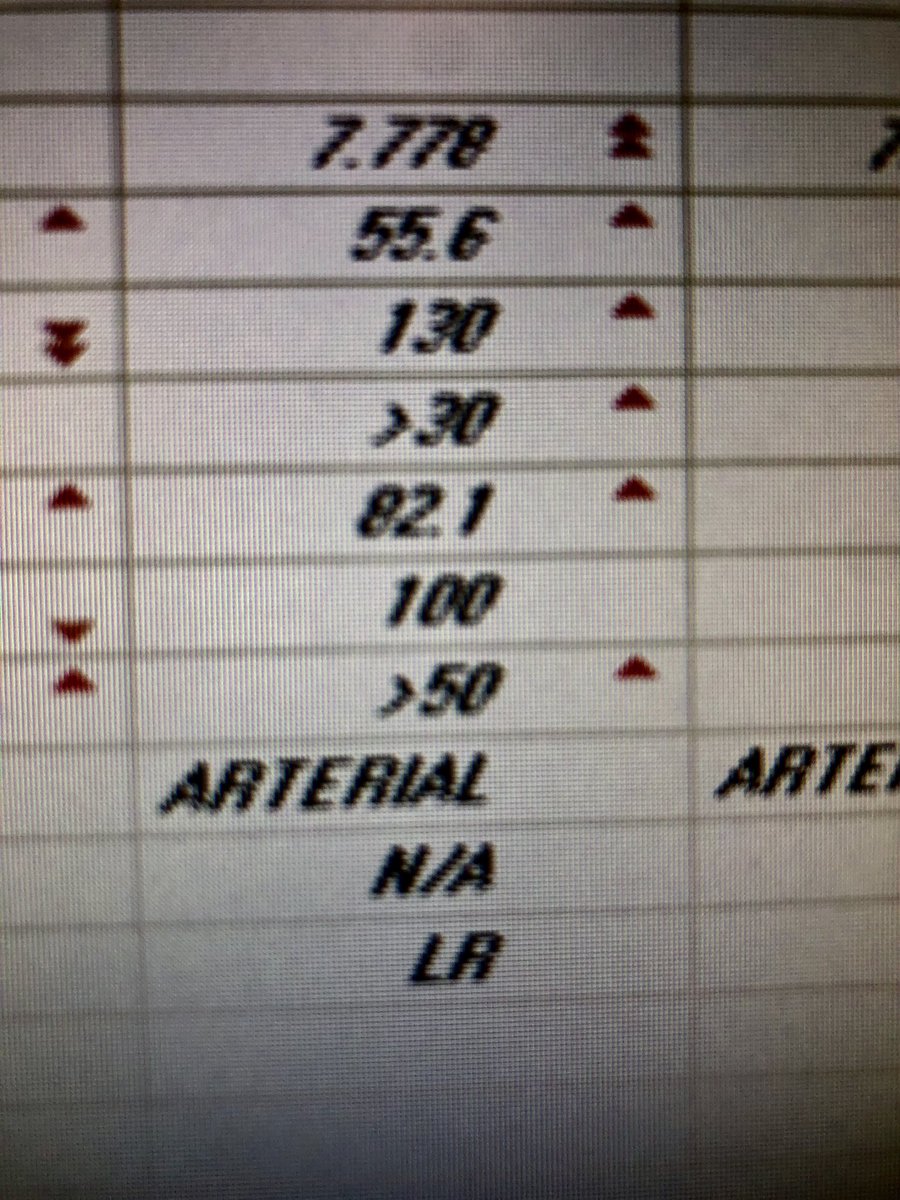
9/n I’m itchy. curbsided master diagnostician @martinr43087111 who points out that only 1/6 blood cultures + for MRSA is unusual. Bartonella IgM, IgG and PCR were ordered: 

10/n wait, 2 different species growing? Nope, it’s just cross-reactivity. pubmed.ncbi.nlm.nih.gov/8810011/ A repeat TTE is done and reports potential fibrin strands in the pulmonic valve, but not conclusive for SBE. So still not confirmed a source…
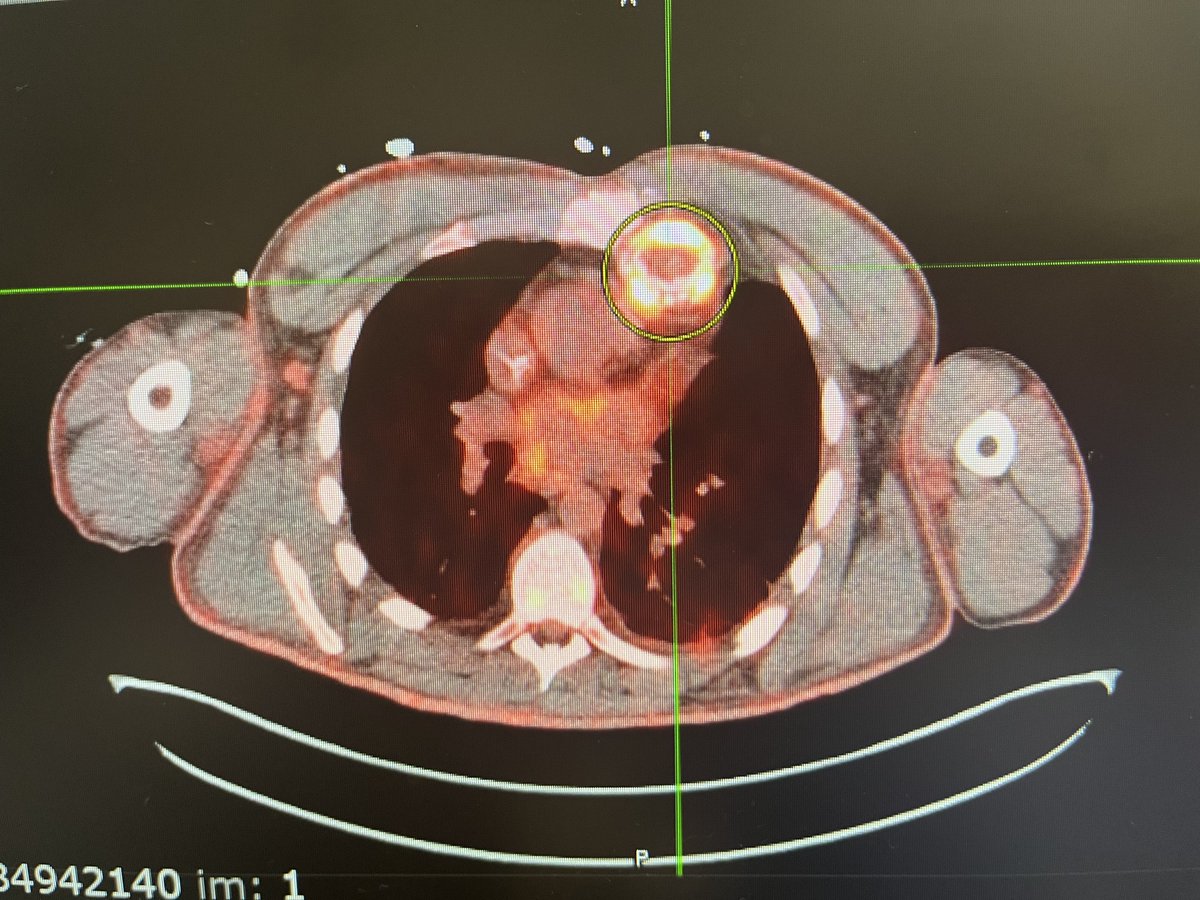
11/n any other way to catch the source that it’s not a TEE? 18-F FDG NM PET scan has been described as useful. pubmed.ncbi.nlm.nih.gov/34363148/
13/n Bartonella PCR comes back negative. However, sensitivity of PCR is low and treatment is warranted based on serology and Duke criteria. Doxy + rifampin + CFTX are started 



14/n how did the patient get infected? Upon further questioning by medical student @roxnonna23, pt had been exposed with cats with fleas weeks preceding the development of symptoms. Cat lovers, think again
15/n 5/6 blood culture specimens were tossed after 7 days of no growth. There is a reason why Bartonella is known as culture neg SBE. However, our astute ID team ordered more sensitive test for Bartonella DNA (clinicalmetagenomics.org/wp-content/upl…): positive! 

16/n pt d/c stable. We hope 4 good progress, learning points:
✅🔬RBC casts/acanthocytes can turn cases 180
✅PR3+ in SBE-GN is not rare➡️ should not lead to AAV IST
✅after Stap/Strep, think Bartonella in SBE-GN
✅Bartonella Ig crossreact
✅Karius > PCR for DNA
✅FDG PET useful
✅🔬RBC casts/acanthocytes can turn cases 180
✅PR3+ in SBE-GN is not rare➡️ should not lead to AAV IST
✅after Stap/Strep, think Bartonella in SBE-GN
✅Bartonella Ig crossreact
✅Karius > PCR for DNA
✅FDG PET useful
17/17 but perhaps the most important learning point: not settling with an unsatisfactory diagnostic work up is our duty. Be determined and objective to follow the clues. Who will benefit? The patient. @OchsnerNephro
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter