Academic Nephrologist @OchsnerNephro | @OchsnerHealth | Ochsner Clinical School-@UQMedicine Faculty
3 subscribers
How to get URL link on X (Twitter) App


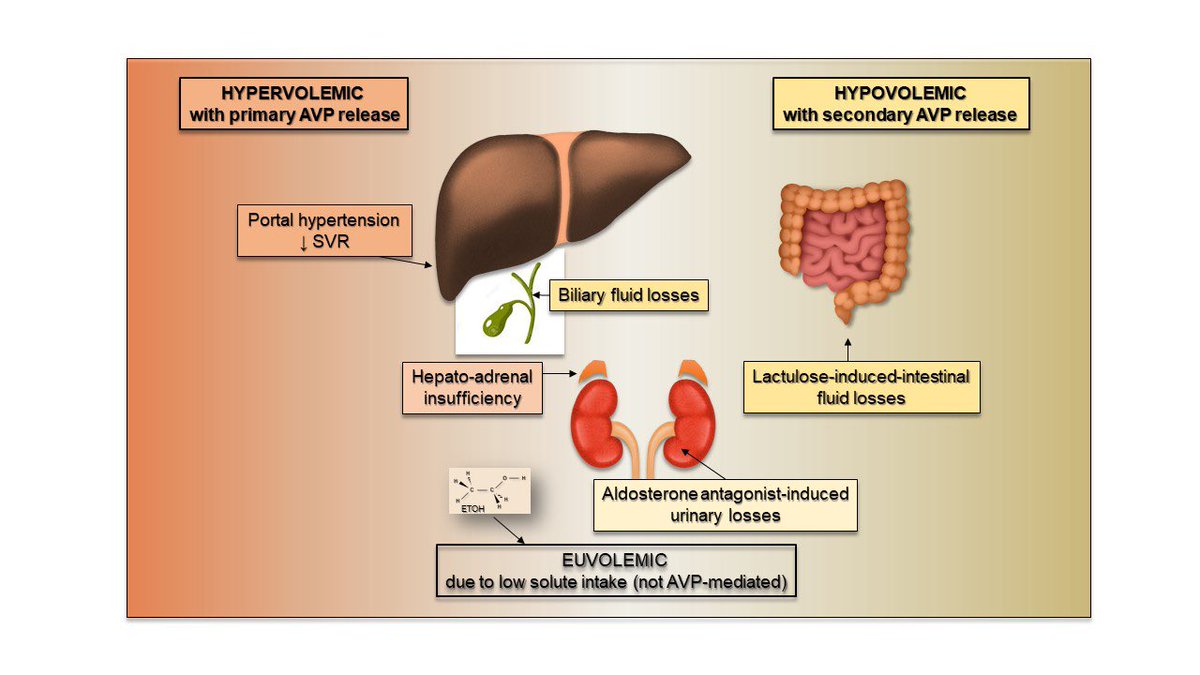
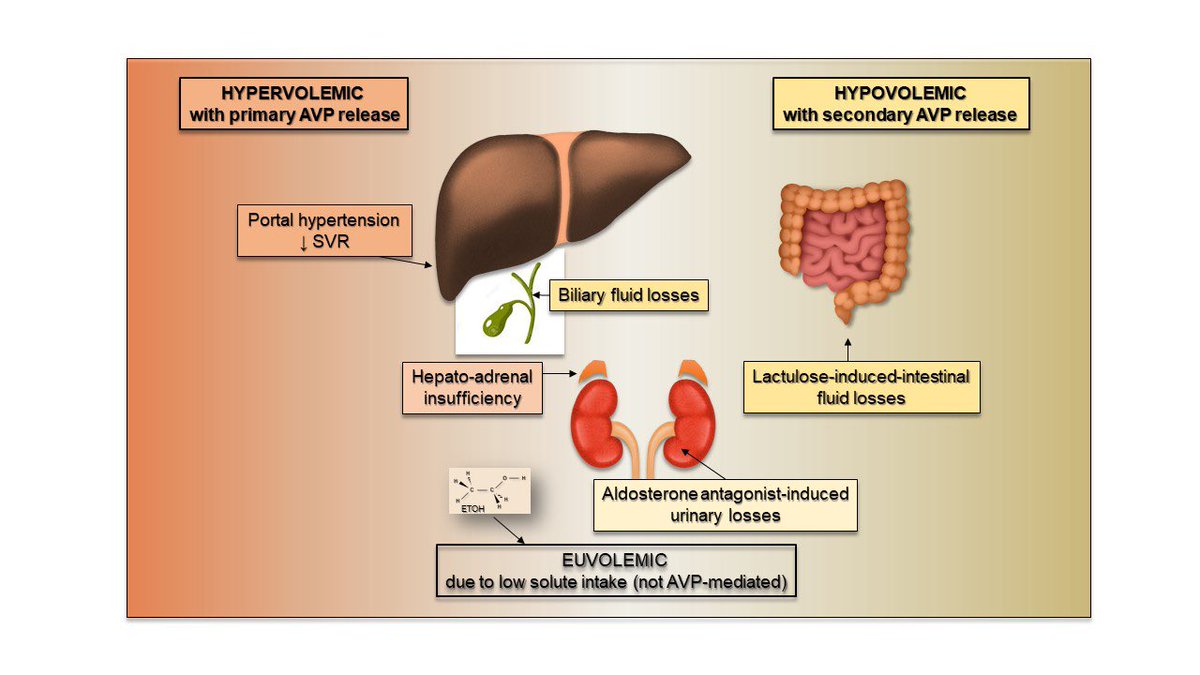 2/n…uNa 48 uOsm 456. No obvious hypervolemia. Dilemma: is uNa not <10 due to ongoing diuretics? History must prevail: exposure to diuretics/laxatives suggest volume depletion factor. Despite high uNa, diuretics are stopped, IV albumin 25 g QID started. 24 hrs later, sNa 129.
2/n…uNa 48 uOsm 456. No obvious hypervolemia. Dilemma: is uNa not <10 due to ongoing diuretics? History must prevail: exposure to diuretics/laxatives suggest volume depletion factor. Despite high uNa, diuretics are stopped, IV albumin 25 g QID started. 24 hrs later, sNa 129.


 2/n immediate reminder that while rhabdomyolysis CAUSES hyperkalemia, hypokalemia may CAUSE hypokalemia: K depletion causes muscle ischemia by preventing normal release of K from myocytes during contraction. Couple of case reports: https://t.co/lNxjqnEnJ2 https://t.co/Qel7WVXH3Ypubmed.ncbi.nlm.nih.gov/24352794/
2/n immediate reminder that while rhabdomyolysis CAUSES hyperkalemia, hypokalemia may CAUSE hypokalemia: K depletion causes muscle ischemia by preventing normal release of K from myocytes during contraction. Couple of case reports: https://t.co/lNxjqnEnJ2 https://t.co/Qel7WVXH3Ypubmed.ncbi.nlm.nih.gov/24352794/

 2/n pt had a bioprosthetic pulmonic valve from a remote tetralogy of Fallot repair. Radar now centered in the connection between heart valve disease and endocarditis-associated glomerulonephritis (SBE-GN). A transthoracic echocardiogram: no vegetations, no valvular insufficiency
2/n pt had a bioprosthetic pulmonic valve from a remote tetralogy of Fallot repair. Radar now centered in the connection between heart valve disease and endocarditis-associated glomerulonephritis (SBE-GN). A transthoracic echocardiogram: no vegetations, no valvular insufficiency




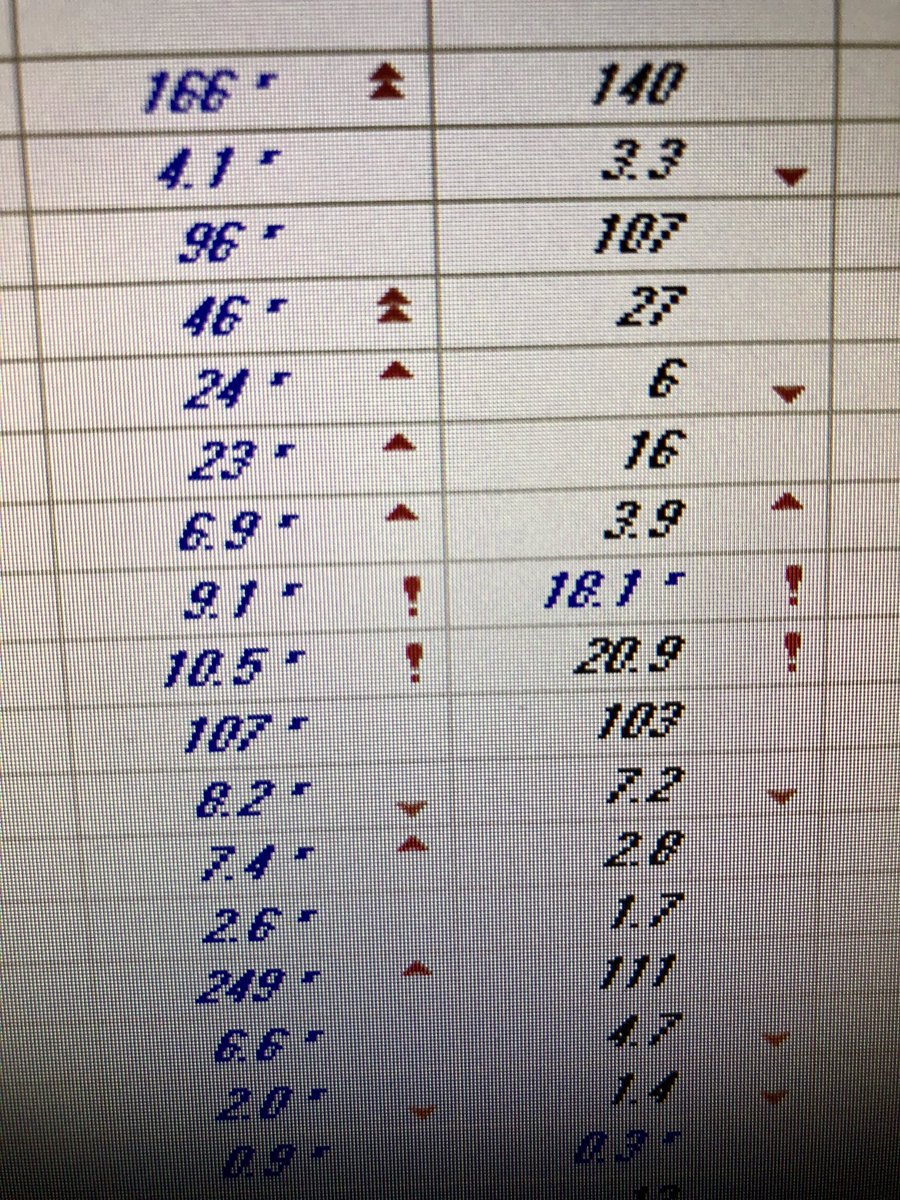
 2/x the high CO2 (46) suggests met alkalosis. Now, that’s unexpected in a pt with GI losses from supposedly a duodenal fistula. Could he just be a CO2 retainer? Well the ABG confirmed primary met alkalosis. Calculated HCO3 82! That’s a personal record. UOP <400cc/d; no diuretics
2/x the high CO2 (46) suggests met alkalosis. Now, that’s unexpected in a pt with GI losses from supposedly a duodenal fistula. Could he just be a CO2 retainer? Well the ABG confirmed primary met alkalosis. Calculated HCO3 82! That’s a personal record. UOP <400cc/d; no diuretics