Longish Thread 👇
Methylprednisolone eye drops, manufactured by Gujarat based Indiana Ophthalmics is suspected of causing infections of the eye in more than 35 people in Sri Lanka.
thewire.in/health/cdcso-i…
1/n
Methylprednisolone eye drops, manufactured by Gujarat based Indiana Ophthalmics is suspected of causing infections of the eye in more than 35 people in Sri Lanka.
thewire.in/health/cdcso-i…
1/n
2/n
This is not the first instance of eye drops causing harm to patients; recall that a few months ago, Global Pharma, another Indian manufacturer was cited for similar issues in the USA
usatoday.com/story/news/hea…
@foxerinr @annaedney
This is not the first instance of eye drops causing harm to patients; recall that a few months ago, Global Pharma, another Indian manufacturer was cited for similar issues in the USA
usatoday.com/story/news/hea…
@foxerinr @annaedney
3/n
While we see typical noises being made about the drug regulator inspecting the company for compliance with manufacturing standards. Lets take a look and see if our own drug labs have found similar issues with eye drops sold in our country, shall we?
ndtv.com/india-news/guj…
While we see typical noises being made about the drug regulator inspecting the company for compliance with manufacturing standards. Lets take a look and see if our own drug labs have found similar issues with eye drops sold in our country, shall we?
ndtv.com/india-news/guj…
4/n
A cursory search of the XLN database, which has state drug testing results from three states (although four additional states apparently have begun reporting data into this database) tells you the following:
A cursory search of the XLN database, which has state drug testing results from three states (although four additional states apparently have begun reporting data into this database) tells you the following:

5/n
A closer look at the reasons for failure in drug testing labs shows almost a third of these are related to sterility.
Lets understand what this means, when it comes to what are called “sterile formulations”. Eye drops, injections etc. fall within this category.
A closer look at the reasons for failure in drug testing labs shows almost a third of these are related to sterility.
Lets understand what this means, when it comes to what are called “sterile formulations”. Eye drops, injections etc. fall within this category.
6/n
Formulations like eye drops, injections etc. should be manufactured under “sterile” conditions.
The WHO guideline for sterile manufacturing says the following:
cdn.who.int/media/docs/def…
Formulations like eye drops, injections etc. should be manufactured under “sterile” conditions.
The WHO guideline for sterile manufacturing says the following:
cdn.who.int/media/docs/def…

7/n
The way we ensure sterility is to make sure that the facility has proper HVAC control (air flow control), aseptic preparation and filling, airlocks for physical separation, proper disinfection and controlled (DI) water systems.
The way we ensure sterility is to make sure that the facility has proper HVAC control (air flow control), aseptic preparation and filling, airlocks for physical separation, proper disinfection and controlled (DI) water systems.
8/n
As we recount in our book #truthpill, our lawmakers, under intense lobbying from the pharmaceutical industry, diluted reasonable and effective standards in the code, thereby allowing unscrupulous manufacturers to end-run globally accepted standards for sterile manufacturing.
As we recount in our book #truthpill, our lawmakers, under intense lobbying from the pharmaceutical industry, diluted reasonable and effective standards in the code, thereby allowing unscrupulous manufacturers to end-run globally accepted standards for sterile manufacturing.

9/n
And that is how we arrive here. If you look at the pharma manufacturers whose products have been suspect in the US and Sri Lanka, they fall squarely in the MSME category.
We have heard that most of these facilities are WHO cGMP compliant, this is an industry talking point.
And that is how we arrive here. If you look at the pharma manufacturers whose products have been suspect in the US and Sri Lanka, they fall squarely in the MSME category.
We have heard that most of these facilities are WHO cGMP compliant, this is an industry talking point.
10/n
Most of these manufacturing facilities do not comply with cGMP.
This is not to say that the large Gx manufacturers are better.
Recall the incident at the peak of the Covid pandemic where Remdesivir injections suspected of endotoxin contamination allegedly manufactured by
Most of these manufacturing facilities do not comply with cGMP.
This is not to say that the large Gx manufacturers are better.
Recall the incident at the peak of the Covid pandemic where Remdesivir injections suspected of endotoxin contamination allegedly manufactured by
11/n
a large pharma were linked to several deaths in Bihar.
@PriyankaPulla
livemint.com/science/health…
a large pharma were linked to several deaths in Bihar.
@PriyankaPulla
livemint.com/science/health…
12/n
In addition to not following cGMP for sterile manufacturing, the other large source of contamination in “sterile formulations” is the water used for making the product.
We know the quality of water that is prevalent in our country.
In addition to not following cGMP for sterile manufacturing, the other large source of contamination in “sterile formulations” is the water used for making the product.
We know the quality of water that is prevalent in our country.
13/n
Water for Injection (WFI) or Distilled/Deionized water is rarely used by our MSME sector when formulating these products. That is one of the biggest source of contaminants in our drug supply.
Water for Injection (WFI) or Distilled/Deionized water is rarely used by our MSME sector when formulating these products. That is one of the biggest source of contaminants in our drug supply.
14/n
Now lets turn to the capacity of the State Drug Labs to test these sterile products for contamination. A standard test which is used to detect microbial contamination is the Endotoxin test.
Now lets turn to the capacity of the State Drug Labs to test these sterile products for contamination. A standard test which is used to detect microbial contamination is the Endotoxin test.
15/n
In our survey, other than the Central Drug Labs, we found that most state drug labs have neither the equipment, nor the training of their analysts to conduct this test.
Therefore, you can surmise what the prevalence of contaminants is in our sterile injectables.
In our survey, other than the Central Drug Labs, we found that most state drug labs have neither the equipment, nor the training of their analysts to conduct this test.
Therefore, you can surmise what the prevalence of contaminants is in our sterile injectables.
16/n
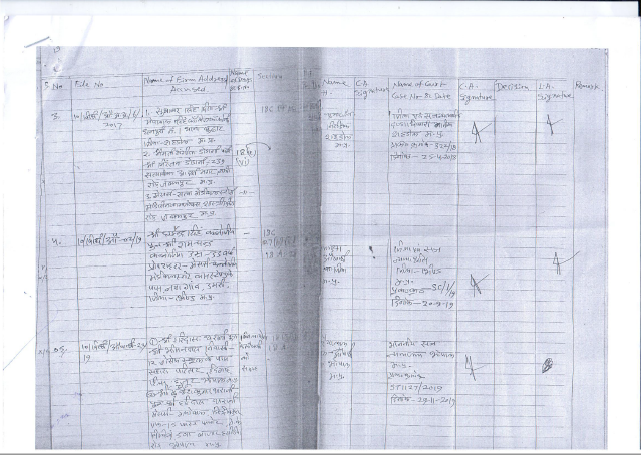
Finally, lets look at how our legal justice system treats those who are caught making medicines contaminated with bacteria.
The first example is that of M/s.Tamman Titoe Pharma Pvt. Ltd., from the COURT OF XV METROPOLITAN MAGISTRATE, GEORGETOWN, CHENNAI.
Finally, lets look at how our legal justice system treats those who are caught making medicines contaminated with bacteria.
The first example is that of M/s.Tamman Titoe Pharma Pvt. Ltd., from the COURT OF XV METROPOLITAN MAGISTRATE, GEORGETOWN, CHENNAI.
17/n
Here, the court found that the sample sourced by the state drug inspector failed BET (Bacterial Endotoxin Test).
dineshthakur.com/wp-content/upl…
However, the court, in its majesty awarded the following sentence to the manufacturer:
Here, the court found that the sample sourced by the state drug inspector failed BET (Bacterial Endotoxin Test).
dineshthakur.com/wp-content/upl…
However, the court, in its majesty awarded the following sentence to the manufacturer:

18/n
The second example is from COURT OF THE CHIEF JUDICIAL MAGISTRATE, THALASSERY where M/s. Modern Laboratories was convicted of manufacturing Ampicillin Injection IP 500 mg.
Again, the Court, in its wisdom and majesty imposed the following sentence on the erring manufacturer
The second example is from COURT OF THE CHIEF JUDICIAL MAGISTRATE, THALASSERY where M/s. Modern Laboratories was convicted of manufacturing Ampicillin Injection IP 500 mg.
Again, the Court, in its wisdom and majesty imposed the following sentence on the erring manufacturer
20/n
Mind you, the law says the sentence in such cases ought to be a minimum one year imprisonment with a maximum punishment of two years and a monetary penalty of Rs. 20,000
Mind you, the law says the sentence in such cases ought to be a minimum one year imprisonment with a maximum punishment of two years and a monetary penalty of Rs. 20,000
21/n
Do you still wonder why our drug supply is so substandard?
And these are exceptions; not many cases of manufacturing substandard medicine are actually prosecuted in a court of law in our country.
Do you still wonder why our drug supply is so substandard?
And these are exceptions; not many cases of manufacturing substandard medicine are actually prosecuted in a court of law in our country.
22/n
Let me close with a few thoughts for you to ponder.
XLN data shows a number of pharma manufacturers who sell their products to us in India have been cited for making substandard medicine, including sterility related issues. How many stories have you read about them?
Let me close with a few thoughts for you to ponder.
XLN data shows a number of pharma manufacturers who sell their products to us in India have been cited for making substandard medicine, including sterility related issues. How many stories have you read about them?
23/n
Or is that these things only matter when eye drops are exported? Do Indian lives not matter?
And why is that? Something to think about.
/end/
Or is that these things only matter when eye drops are exported? Do Indian lives not matter?
And why is that? Something to think about.
/end/
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter