1/ My time-to-tweet interval re: #ASCO23 myeloma abstracts is longer than my time-to-toci with CAR-T, but finally off 🏥 service and excited to tweet about a few #MMsm gems!
My research focuses on ⬇️ AEs, ⬇️ time tox, & improved workflows. Here are a few that stood out to me:
My research focuses on ⬇️ AEs, ⬇️ time tox, & improved workflows. Here are a few that stood out to me:
2/ @bhemato et al, CARTITUDE-4 (cilta-cel in #MMsm 1-3 prior lines).
Beyond dramatic PFS benefit, worth 🔨 home that CAR-T "one & done" (visits become ≤1x per month) vs DPd/VPd [even stronger DKd] always ≥1x visit/month.
Time tox advantage to CAR-T!
meetings.asco.org/abstracts-pres…
Beyond dramatic PFS benefit, worth 🔨 home that CAR-T "one & done" (visits become ≤1x per month) vs DPd/VPd [even stronger DKd] always ≥1x visit/month.
Time tox advantage to CAR-T!
meetings.asco.org/abstracts-pres…

3/ @adamssperling et al, PHE885 rapidly manufactured CAR-T with ⬇️ T-cell exhaustion.
Bridging before #MMsm CAR-T unlikely to ≥PR but likely to worsen cytopenias.
⬇️ vein-to-vein time to ~2 weeks: less bridging, happier bone marrow, happier patients!
meetings.asco.org/abstracts-pres…
Bridging before #MMsm CAR-T unlikely to ≥PR but likely to worsen cytopenias.
⬇️ vein-to-vein time to ~2 weeks: less bridging, happier bone marrow, happier patients!
meetings.asco.org/abstracts-pres…

4/ @AjayNookaMD et al, KPd maintenance for high-risk #MMsm
Ideally Kyprolis will be q2wk and #downwithdex in RRMM (cc @jmikhaelmd), but pom less temperamental than len in CKD plus (?) ⬇️ risk of SPMs... so I'm all in!
Why else I love this abstract 👇

Ideally Kyprolis will be q2wk and #downwithdex in RRMM (cc @jmikhaelmd), but pom less temperamental than len in CKD plus (?) ⬇️ risk of SPMs... so I'm all in!
Why else I love this abstract 👇
https://twitter.com/RahulBanerjeeMD/status/1663546012626202626?s=20

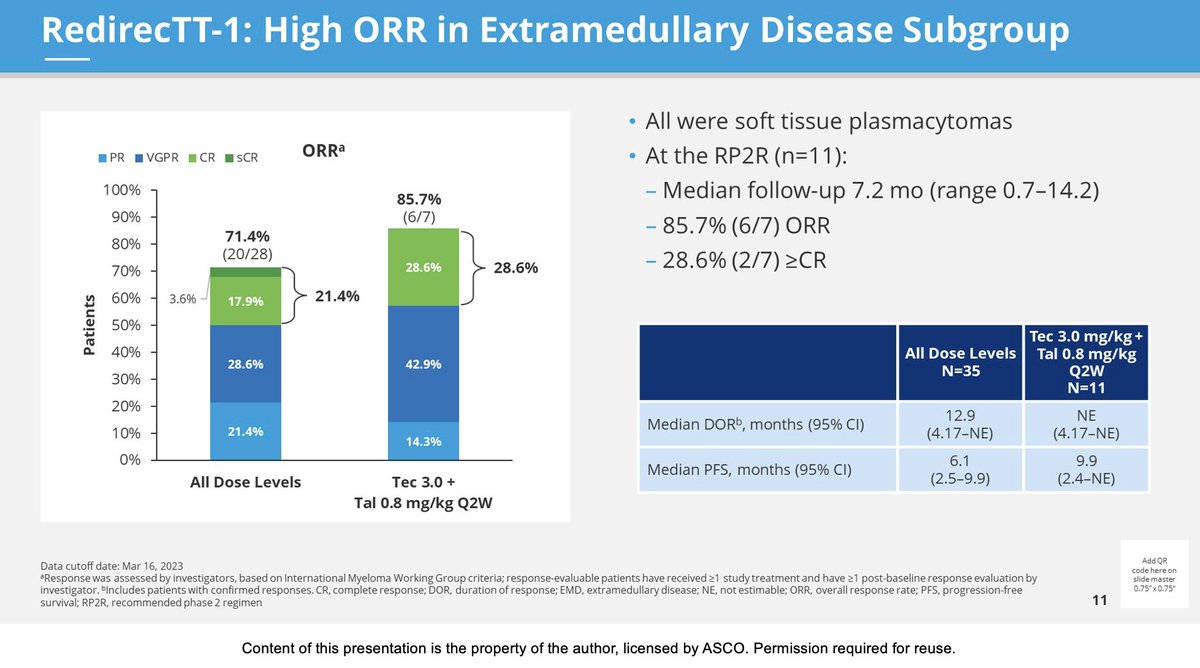
5/ Y Cohen et al, RedirecTT-1 of tec/tal in #MMsm.
bsAbs targeting BCMA and GPRC5D at once. Infxns manageable. Look at these responses & duration in EMD!
P.S. Doubly impressive because authors were EMD purists, i.e. only soft-tissue = "extra"medullary.
meetings.asco.org/abstracts-pres…
bsAbs targeting BCMA and GPRC5D at once. Infxns manageable. Look at these responses & duration in EMD!
P.S. Doubly impressive because authors were EMD purists, i.e. only soft-tissue = "extra"medullary.
meetings.asco.org/abstracts-pres…
6/ @DholariaMD et al, TRIMM-2 of talq + dara.
"Flogging T cells to attack B-lineage cells" is a crude description of BCMA bsAb given weekly until #MMsm PD.
In grand multiverse, a BCMA-free combo exists: def lower infection rates than I'd have expected!
meetings.asco.org/abstracts-pres…
"Flogging T cells to attack B-lineage cells" is a crude description of BCMA bsAb given weekly until #MMsm PD.
In grand multiverse, a BCMA-free combo exists: def lower infection rates than I'd have expected!
meetings.asco.org/abstracts-pres…

7/ Switching to posters: @RoswellPark study of T-cell phenotype before & after 6-month physical activity intervention.
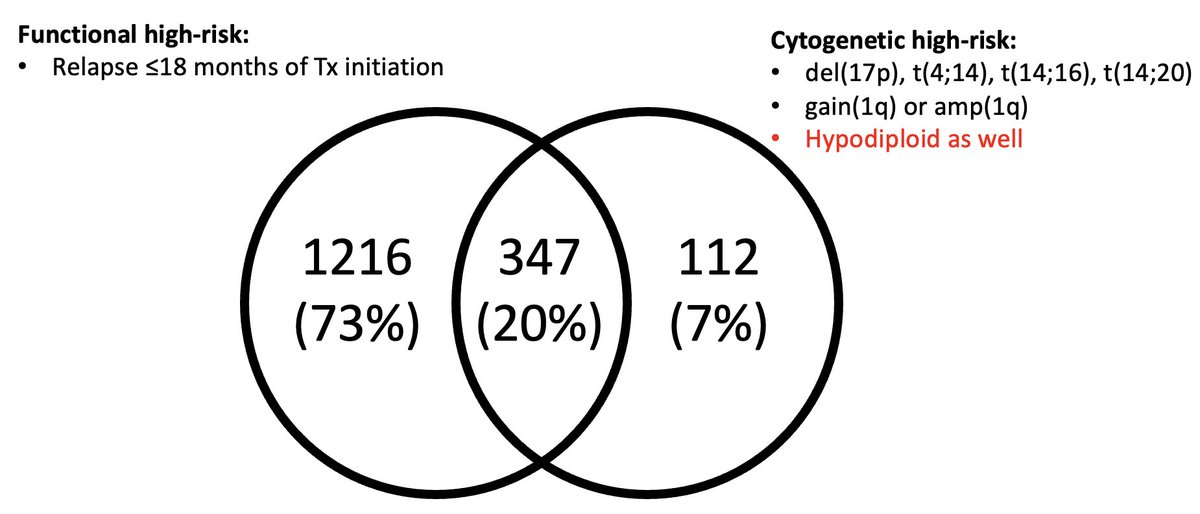
Great way to shed some pounds, but more importantly shed PD-L1 & TIGIT! Exhausted T cells may contribute to functional high risk #MMsm.
meetings.asco.org/abstracts-pres…
Great way to shed some pounds, but more importantly shed PD-L1 & TIGIT! Exhausted T cells may contribute to functional high risk #MMsm.
meetings.asco.org/abstracts-pres…

8/ @Radhika_Bansl @YiLinMDPhD outpatient teclistamab in #MMsm using day hospital and RPM #cellphonesandcelltherapies
98% of 155 tec doses safely given as outpt 🤯
⬇️ costs of care, ⬇️ monster 10-day LOS, happier patients (no 🛌 better than one's own!)
meetings.asco.org/abstracts-pres…
98% of 155 tec doses safely given as outpt 🤯
⬇️ costs of care, ⬇️ monster 10-day LOS, happier patients (no 🛌 better than one's own!)
meetings.asco.org/abstracts-pres…

9/ @KimmelCancerCtr retrospective analysis of time to Zometa in new Dx #MMsm.
Definitely some confounders, e.g. pre-existing access to dentist probably = ⬆️ SES.
But maybe we - myself included! - are overemphasizing need for dental 'clearance' in all...
meetings.asco.org/abstracts-pres…
Definitely some confounders, e.g. pre-existing access to dentist probably = ⬆️ SES.
But maybe we - myself included! - are overemphasizing need for dental 'clearance' in all...
meetings.asco.org/abstracts-pres…

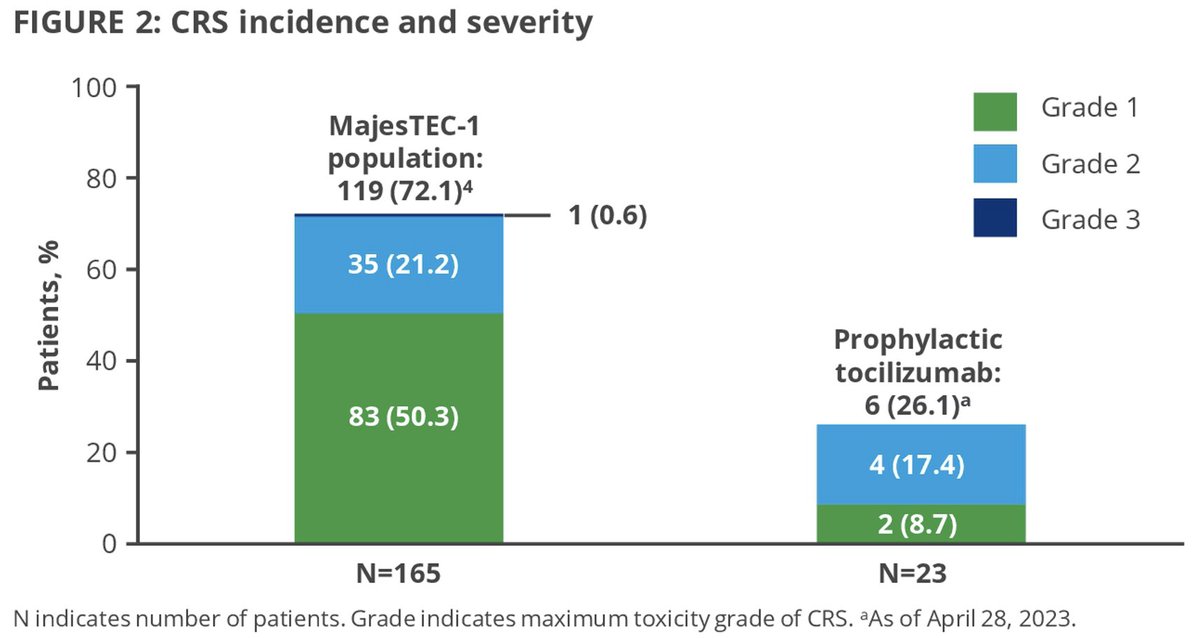
10/ van de Donk et al with PPx toci before teclistamab in #MMsm.
Any-grade CRS less than half of MajesTEC-1, similar to #ASH23 oral with cevostamab by Trudel & colleagues. ⬇️ CRS = ⬇️ time in hospital!
Now if only we can get a subQ version of toci...
meetings.asco.org/abstracts-pres…
Any-grade CRS less than half of MajesTEC-1, similar to #ASH23 oral with cevostamab by Trudel & colleagues. ⬇️ CRS = ⬇️ time in hospital!
Now if only we can get a subQ version of toci...
meetings.asco.org/abstracts-pres…
11/ @AhlstromJenny et al: @HealthTree survey of 325 pts.
Although my research interests are ⬇️ AEs / time tox, our #MMsm pts bravely willing to put up with a LOT if it'll help.
Bottom two 👇 less "trade-offable": fin tox & caregiver research important!
meetings.asco.org/abstracts-pres…
Although my research interests are ⬇️ AEs / time tox, our #MMsm pts bravely willing to put up with a LOT if it'll help.
Bottom two 👇 less "trade-offable": fin tox & caregiver research important!
meetings.asco.org/abstracts-pres…

• • •
Missing some Tweet in this thread? You can try to
force a refresh