The long awaited #COVIDOUT RCT is now in @TheLancet:
- high risk adults randomized to either metformin (MET), ivermectin (IVM), fluvoxamine (FLV) or placebo.
- MET reduced the risk of long COVID (6.3% vs 10.4%; NNT = 24)
- no benefit with IVM or FLV
thelancet.com/journals/lanin…
1/



- high risk adults randomized to either metformin (MET), ivermectin (IVM), fluvoxamine (FLV) or placebo.
- MET reduced the risk of long COVID (6.3% vs 10.4%; NNT = 24)
- no benefit with IVM or FLV
thelancet.com/journals/lanin…
1/

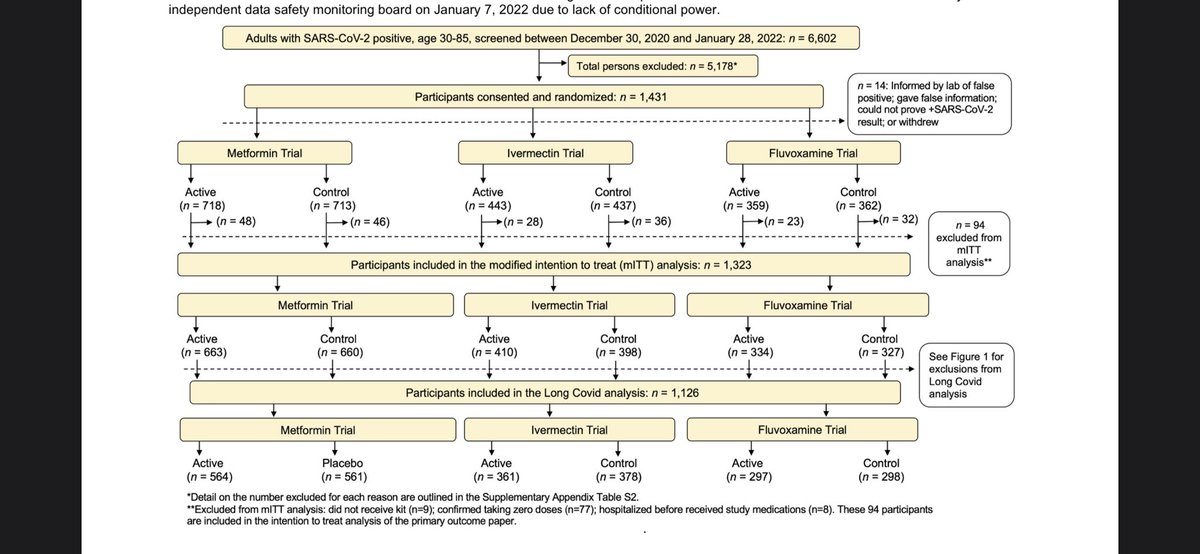
COVID-OUT was a large blinded multicenter RCT looking at repurposed oral meds.
The primary outcome was severe COVID; this was one of the *MANY* negative RCTs of ivermectin. (See 🧵👇)
The current study is a planned secondary analysis, looking at the incidence of long COVID.
2/
The primary outcome was severe COVID; this was one of the *MANY* negative RCTs of ivermectin. (See 🧵👇)
The current study is a planned secondary analysis, looking at the incidence of long COVID.
2/
https://twitter.com/nickmmark/status/1560272414323249152
COVID-OUT was a factorial design enabling efficient evaluation of multiple oral medications in various combinations.
After diagnosis, subjects received meds by next day mail. They were followed up to 300 days (10 months).
Diagnosis of long COVID was made by a synonym survey
3/


After diagnosis, subjects received meds by next day mail. They were followed up to 300 days (10 months).
Diagnosis of long COVID was made by a synonym survey
3/



The subjects who received metformin were well matched to controls.
The patients (across all treatment arms) who developed long COVID were more likely to:
- be female
- be unvaccinated
- have a higher BMI
- have been symptomatic for >3 days at diagnosis
4/

The patients (across all treatment arms) who developed long COVID were more likely to:
- be female
- be unvaccinated
- have a higher BMI
- have been symptomatic for >3 days at diagnosis
4/


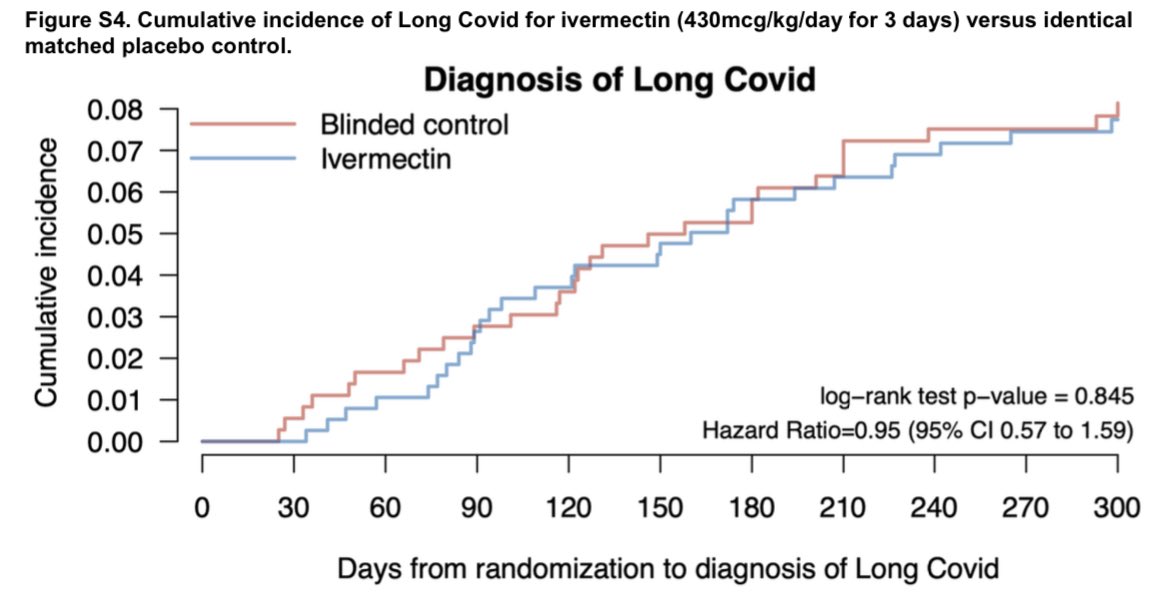
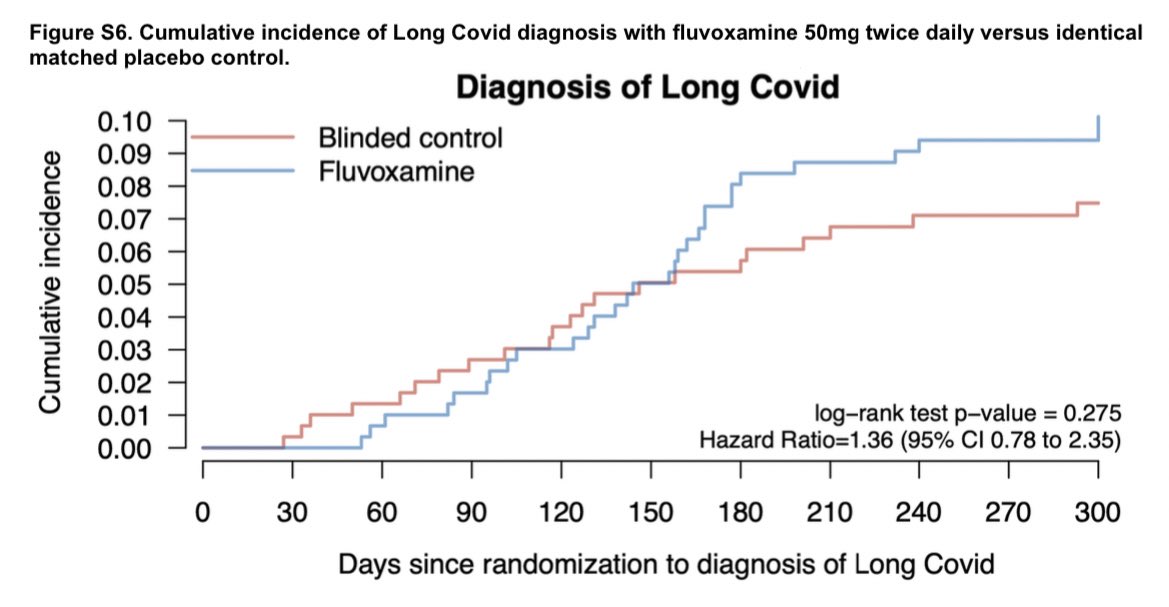
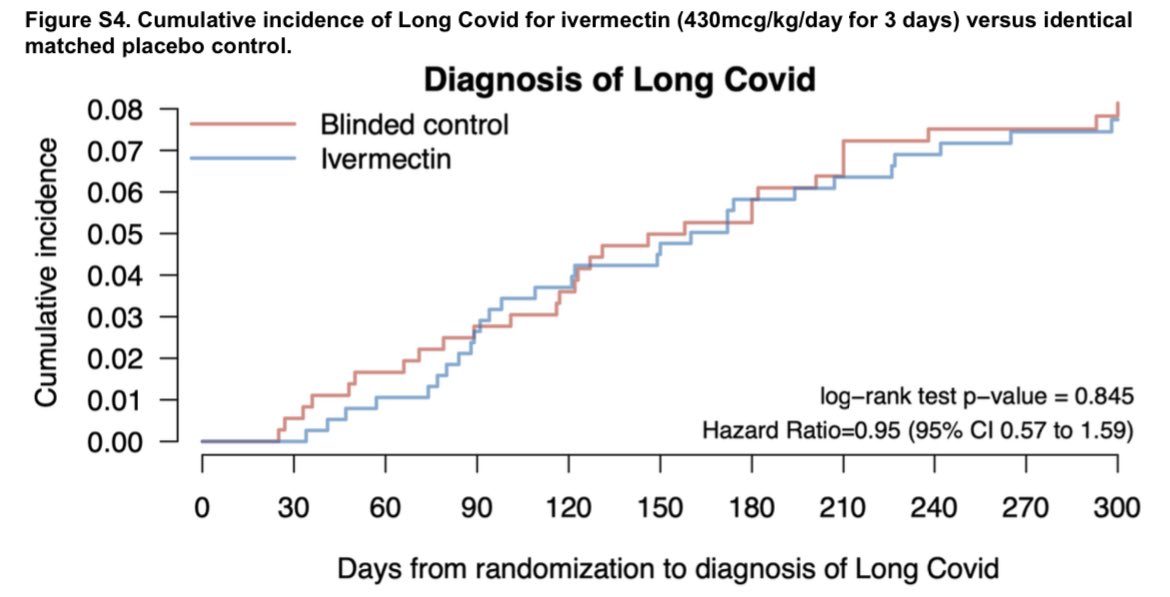
Two of the three meds - IVM & FLV - struck out completely:
Neither Ivermectin (HR 0.95, 95% CI 0.57–1.59) nor fluvoxamine (HR 1·36, 95% CI 0·78–2·35) reduced the incidence of long COVID compared to matched placebo.
They also failed across *ALL* pre-specified subgroups.
5/



Neither Ivermectin (HR 0.95, 95% CI 0.57–1.59) nor fluvoxamine (HR 1·36, 95% CI 0·78–2·35) reduced the incidence of long COVID compared to matched placebo.
They also failed across *ALL* pre-specified subgroups.
5/



Metformin on the other 🤚, had a statistically & clinically significant effect on long COVID:
- substantially fewer symptoms
- fewer symptoms affecting subjects ability to work
- overall lower incidence of long COVID (6.3% vs 10.4%)
6/


- substantially fewer symptoms
- fewer symptoms affecting subjects ability to work
- overall lower incidence of long COVID (6.3% vs 10.4%)
6/



Notably, among subject who had been vaccinated & boosted the incidence of long COVID was also much lower!
- placebo 10.4%
- metformin 6.6%
- vaccinated 6.6%
- vaccinated + boosted 1.8%
7/
- placebo 10.4%
- metformin 6.6%
- vaccinated 6.6%
- vaccinated + boosted 1.8%
7/
🟩Metformin appeared to be *more beneficial* if given earlier & in younger patients.
🟥Also worth pointing out that the combination of metformin & other drugs was actually *LESS* effective!
(The combination with IVM removed the benefit! Don’t tell those FLCCC quacks 🦆)
8/
🟥Also worth pointing out that the combination of metformin & other drugs was actually *LESS* effective!
(The combination with IVM removed the benefit! Don’t tell those FLCCC quacks 🦆)
8/

Bottom line:
- this analysis of the COVID-OUT RCT suggests that metformin treatment DOES reduce the risk of long COVID, at least in high risk unvaccinated people.
- BUT the benefit is LOST if combined with IVM or fluvoxamine
- and getting vaxxed + boosted works even better!
9/9
- this analysis of the COVID-OUT RCT suggests that metformin treatment DOES reduce the risk of long COVID, at least in high risk unvaccinated people.
- BUT the benefit is LOST if combined with IVM or fluvoxamine
- and getting vaxxed + boosted works even better!
9/9
• • •
Missing some Tweet in this thread? You can try to
force a refresh
































