1/ #ContinuumCase!!
A 50 yo man presented to the ED with acute onset aphasia. He is not able to report a history, but BP Is 215/95.
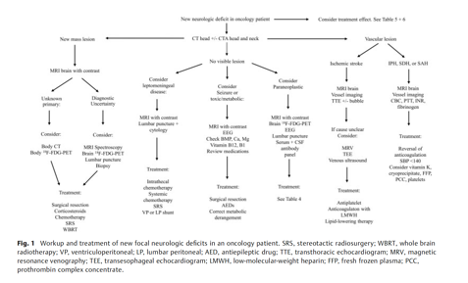
Non-contrast HCT reveals this bleed…
What do you want to see next?
A 50 yo man presented to the ED with acute onset aphasia. He is not able to report a history, but BP Is 215/95.
Non-contrast HCT reveals this bleed…
What do you want to see next?
2/
What do you most want next?
What do you most want next?
3/
Cortical bleeds are IMHO way more fun than basal ganglia hemorrhages.
Even though BP was elevated, that is true of many patients who have non-hypertensive etiologies of their bleeds!
In these patients you must consider:
🩸CAA
🩸Endocarditis
🩸Atypical aneurysms
🩸RCVS....
Cortical bleeds are IMHO way more fun than basal ganglia hemorrhages.
Even though BP was elevated, that is true of many patients who have non-hypertensive etiologies of their bleeds!
In these patients you must consider:
🩸CAA
🩸Endocarditis
🩸Atypical aneurysms
🩸RCVS....
4/
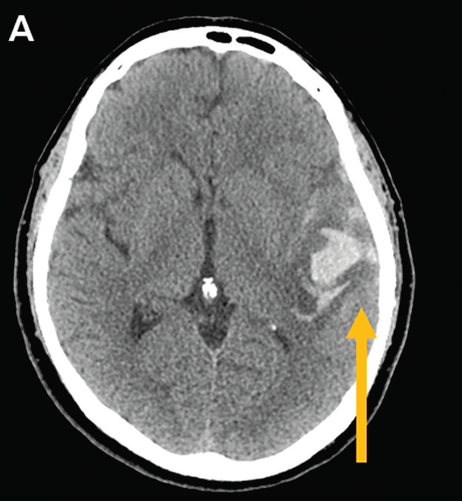
And ... Venous Sinus Thrombosis!
In this case, even just a closer review of the non-con provides a very important clue.
A cord sign! A hyperdense signal within a venous sinus (in this case transverse / sigmoid sinus)
And ... Venous Sinus Thrombosis!
In this case, even just a closer review of the non-con provides a very important clue.
A cord sign! A hyperdense signal within a venous sinus (in this case transverse / sigmoid sinus)
5/
Note that there are numerous venous variants, but the two important cortical veins to remember are the Vein of Trolard (top) drains to saggital sinus; and Vein of Labbe (low) drains to transverse sinus.
Note that there are numerous venous variants, but the two important cortical veins to remember are the Vein of Trolard (top) drains to saggital sinus; and Vein of Labbe (low) drains to transverse sinus.

6/
Intracerebral hemorrhage is present in 1/3 of patients.
But you should think of CVT if the IPH is:
➡️Multiple
➡️Ill-defined w/ surrounding edema
➡️Non-arterial territories
➡️ Involve bilateral basal ganglia or thalami
➡️ Cortical
Intracerebral hemorrhage is present in 1/3 of patients.
But you should think of CVT if the IPH is:
➡️Multiple
➡️Ill-defined w/ surrounding edema
➡️Non-arterial territories
➡️ Involve bilateral basal ganglia or thalami
➡️ Cortical
7/
While both CTV and MRV with contrast (NOT TOF MRV, poor resolution, proned to artifacts) offer high sensitivity for CVT detection, contrasted MRI can better demonstrate the parenchymal changes.
While both CTV and MRV with contrast (NOT TOF MRV, poor resolution, proned to artifacts) offer high sensitivity for CVT detection, contrasted MRI can better demonstrate the parenchymal changes.
8/
You may even find a brush sign on paramagnetic-sensitive MRI sequences, particularly if there is a deep CVT!
You may even find a brush sign on paramagnetic-sensitive MRI sequences, particularly if there is a deep CVT!

9/
In this case, both CTV and MRV demonstrated thrombus within the transverse sinus, sigmoid sinus, IJ, and vein of Labbe.
In this case, both CTV and MRV demonstrated thrombus within the transverse sinus, sigmoid sinus, IJ, and vein of Labbe.

10/
A thoughtful approach to laboratory testing and further workup is detailed in the @ContinuumAAN article, which you should check out!
But let’s skip to treatment. Whats your next move:
A thoughtful approach to laboratory testing and further workup is detailed in the @ContinuumAAN article, which you should check out!
But let’s skip to treatment. Whats your next move:
11/
While there is mounting evidence for the safety of efficacy of DOACs in CVT, guildelines recommend starting with a parenteral anticoagulant.
The ESO guidelines have a weak recommendation for LMWH > heparin for a non-sig trend towards 🔼 functional outcomes & 🔽 mortality.
While there is mounting evidence for the safety of efficacy of DOACs in CVT, guildelines recommend starting with a parenteral anticoagulant.
The ESO guidelines have a weak recommendation for LMWH > heparin for a non-sig trend towards 🔼 functional outcomes & 🔽 mortality.
12/
With unfractionated heparin, the goal should be to have the drug in the therapeutic range quickly, even if ICH Is present.
With unfractionated heparin, the goal should be to have the drug in the therapeutic range quickly, even if ICH Is present.
13/
For patients who worsen despite medical treatment, EVT is an option although the exact efficacy is still debated.
TO-ACT, a trial of endovascular therapy, has been difficult to interpret due to a small sample size.
For patients who worsen despite medical treatment, EVT is an option although the exact efficacy is still debated.
TO-ACT, a trial of endovascular therapy, has been difficult to interpret due to a small sample size.
14/
For an incredible discussion about this fascinating and rare form of stroke, check out Dr Liberman’s (@ava_liberman) review, which is available in the latest issue of @ContinuumAAN
journals.lww.com/continuum/Full…
For an incredible discussion about this fascinating and rare form of stroke, check out Dr Liberman’s (@ava_liberman) review, which is available in the latest issue of @ContinuumAAN
journals.lww.com/continuum/Full…
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter