1/Having trouble remembering what you should look for in vascular dementia on imaging?
Almost everyone worked up for #dementia has infarcts. Which ones are important?
Here’s THE FULL #tweetorial this time on the key findings in vascular dementia
#meded #medtwitter #neurotwitter
Almost everyone worked up for #dementia has infarcts. Which ones are important?
Here’s THE FULL #tweetorial this time on the key findings in vascular dementia
#meded #medtwitter #neurotwitter
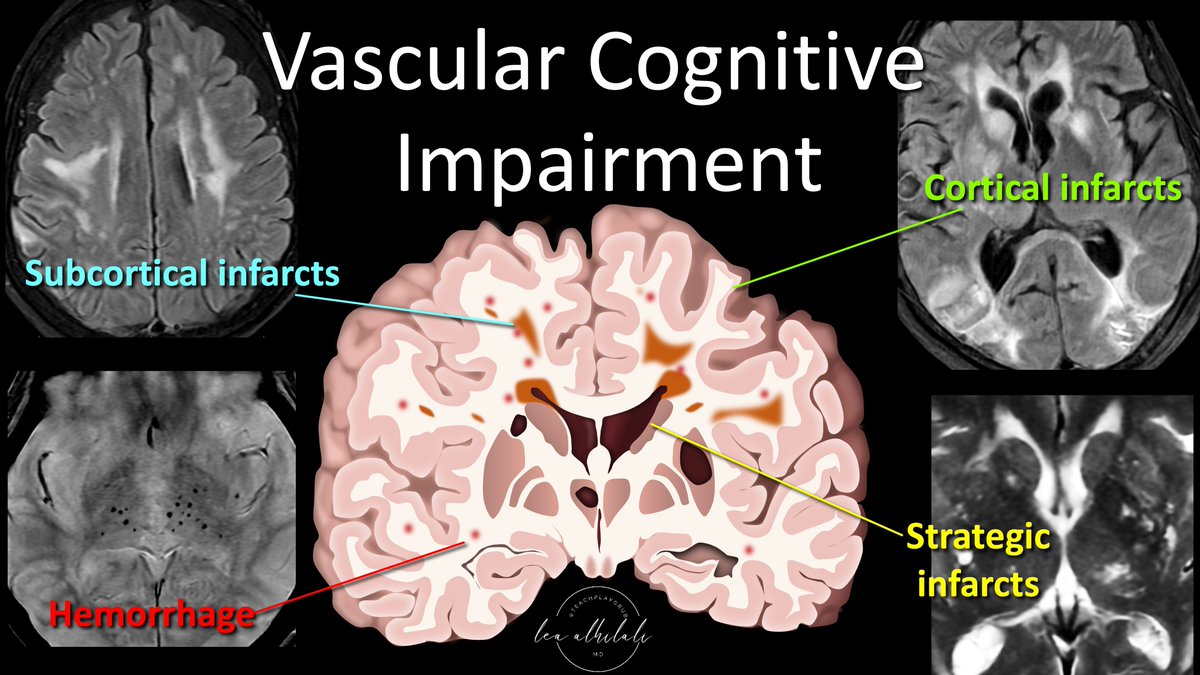
2/Vascular cognitive impairment, or its most serious form, vascular dementia, used to be called multi-infarct dementia.
It was thought dementia directly resulted from brain volume loss from infarcts, w/the thought that 50-100cc of infarcted related volume loss caused dementia
It was thought dementia directly resulted from brain volume loss from infarcts, w/the thought that 50-100cc of infarcted related volume loss caused dementia

3/But that’s now outdated. We now know vascular dementia results from diverse pathologies that all share a common vascular origin.
It’s possible to lose little volume from infarct & still result in dementia.
So if infarcts are common—which contribute to vascular dementia?
It’s possible to lose little volume from infarct & still result in dementia.
So if infarcts are common—which contribute to vascular dementia?

4/To understand which findings are key in vascular dementia, think of a vascular insult to the brain like a punch
Just as each punch does damage, so does each infarct
Not all punches are created equal—nor is every infarct as devastating--& both infarcts & punches are cumulative
Just as each punch does damage, so does each infarct
Not all punches are created equal—nor is every infarct as devastating--& both infarcts & punches are cumulative

5/So every if every punch/infarct causes injury, think of dementia as a knock out—enough damage to overwhelm the brain so that it out of the fight.
The same injuries that cause a knock out are the same ones that can cause vascular dementia. So how do you knock someone out?
The same injuries that cause a knock out are the same ones that can cause vascular dementia. So how do you knock someone out?

6/Classic way is to just beat the daylights out of them. It’s how most fights ends—if there is enough damage, they just can’t stand.
This is multi-infarct dementia, but it’s thought of bit differently than it was in the old days
Volume makes an impact, but it’s not everything
This is multi-infarct dementia, but it’s thought of bit differently than it was in the old days
Volume makes an impact, but it’s not everything
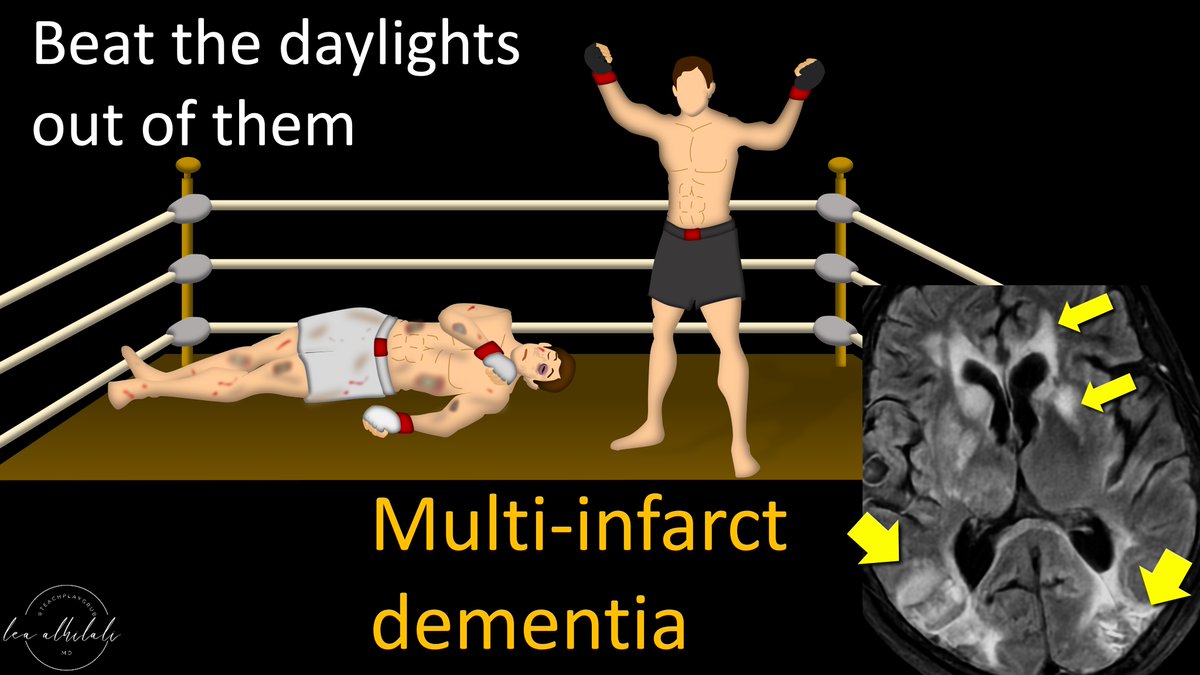
7/It’s like a machine gun shooting at a target. You don’t need good aim, eventually something’s going to hit something important enough to take it down
The new concept of multi-infarct dementia is that it’s not volume per se, but enough volume eventually hits something important
The new concept of multi-infarct dementia is that it’s not volume per se, but enough volume eventually hits something important

8/We used to think that dementia was a direct relationship w/volume lost, but some infarcts are more impactful than others.
But if you have enough infarcts, you will eventually have impactful ones.
So the overall severity of infarcts does still matter.
But if you have enough infarcts, you will eventually have impactful ones.
So the overall severity of infarcts does still matter.

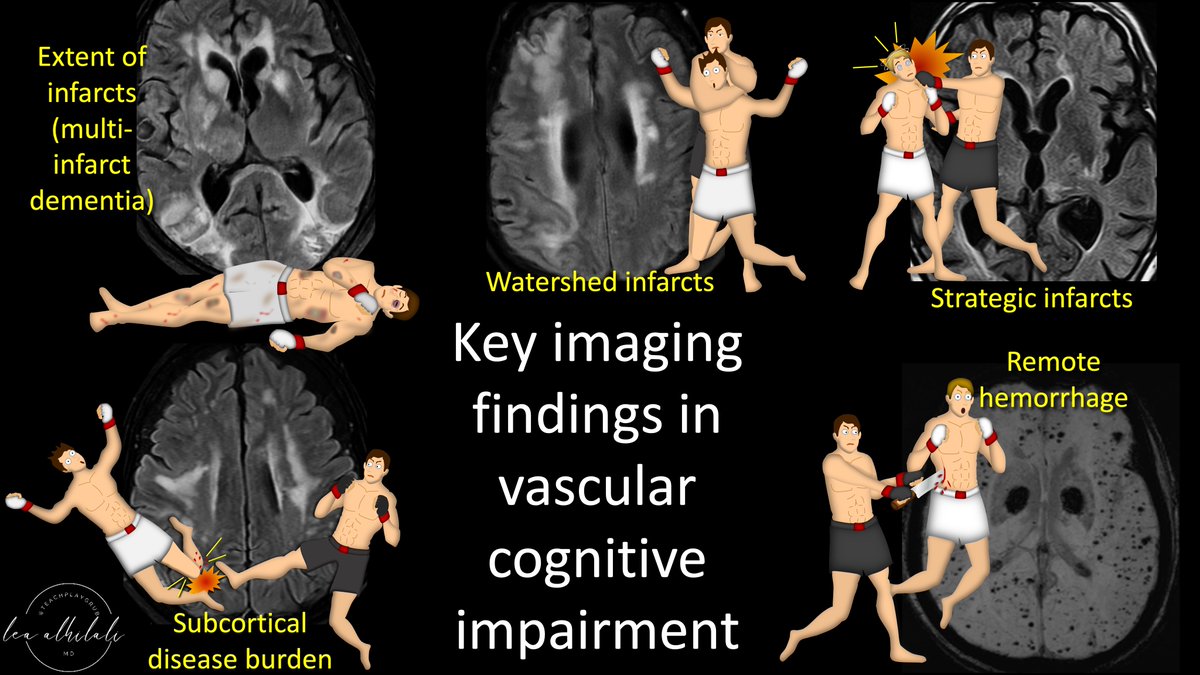
9/Next way to take someone down? The chokehold--hypoperfusion.
Signs of hypoperfusion on imaging are infarcts in the borderzone or watershed distributions.
This is typically from a large (ICA) or medium (MCA) stenosis or occlusion.
Signs of hypoperfusion on imaging are infarcts in the borderzone or watershed distributions.
This is typically from a large (ICA) or medium (MCA) stenosis or occlusion.

10/But it’s not just these infarcts that cause dementia. They are just a sign of the underlying disease.
If there is hypoperfusion, there isn’t just macro hypoperfusion, but also chronic neuronal hypoperfusion at a cellular level that causes damage, dysfunction & dementia
If there is hypoperfusion, there isn’t just macro hypoperfusion, but also chronic neuronal hypoperfusion at a cellular level that causes damage, dysfunction & dementia

11/But we can’t see the damage on a cellular level. We can only see the macroscopic signs on imaging—borderzone infarcts.
Remember the major vascular territories are shaped like a butterfly—infarcts at the butterfly junction are borderzone. These indicate hypoperfusion
Remember the major vascular territories are shaped like a butterfly—infarcts at the butterfly junction are borderzone. These indicate hypoperfusion

12/Next way to take someone down? A knock out punch. A one & done.
These are strategic infarcts.
These are infarcts located in structures directly related to cognition. So damage to these structures results in dementia without any other significant volume loss.
These are strategic infarcts.
These are infarcts located in structures directly related to cognition. So damage to these structures results in dementia without any other significant volume loss.

13/Now, rather than shooting a machine gun at a target, you a like a ninja. Just one shot right to the heart to take it down.
Just one infarct in one of these important structures can cause dementia like a shot to the heart.
So which structures are these?
Just one infarct in one of these important structures can cause dementia like a shot to the heart.
So which structures are these?

14/There are many structures that have been implicated in strategic infarct dementia.
But the main ones are hippocampus, internal capsule (ant & genu), thalamus (paramedian) & caudate.
I remember this w/the mnemonic:
One HIT CAUses dementia
But the main ones are hippocampus, internal capsule (ant & genu), thalamus (paramedian) & caudate.
I remember this w/the mnemonic:
One HIT CAUses dementia

15/Next way to take someone down? Break important connections. Breaking a leg means they ain’t getting up.
Same w/infarcts, small vessel disease or subcortical vascular encephalopathy breaks important white matter connections between parts of the brain so they can’t function
Same w/infarcts, small vessel disease or subcortical vascular encephalopathy breaks important white matter connections between parts of the brain so they can’t function

16/These small vessel infarcts disrupt connections between the frontal lobe & deep gray & parietal lobe, resulting in decreased executive function, attention & memory.
The more small vessel disease, the more impact. So always comment on the severity of small vessel disease
The more small vessel disease, the more impact. So always comment on the severity of small vessel disease

17/The final way to take someone down? Play dirty & make them bleed—hemorrhagic infarcts.
These are a sign of both hypertensive & amyloid small vessel disease.
Amyloid angiopathy has a very strong correlation w/dementia
These are a sign of both hypertensive & amyloid small vessel disease.
Amyloid angiopathy has a very strong correlation w/dementia

18/In fact, amyloid angiopathy has such a strong correlation w/dementia that some say it should be thought of more as a neurodegenerative disorder that occasionally causes hemorrhage/stroke—neurodegeneration is its day job. 
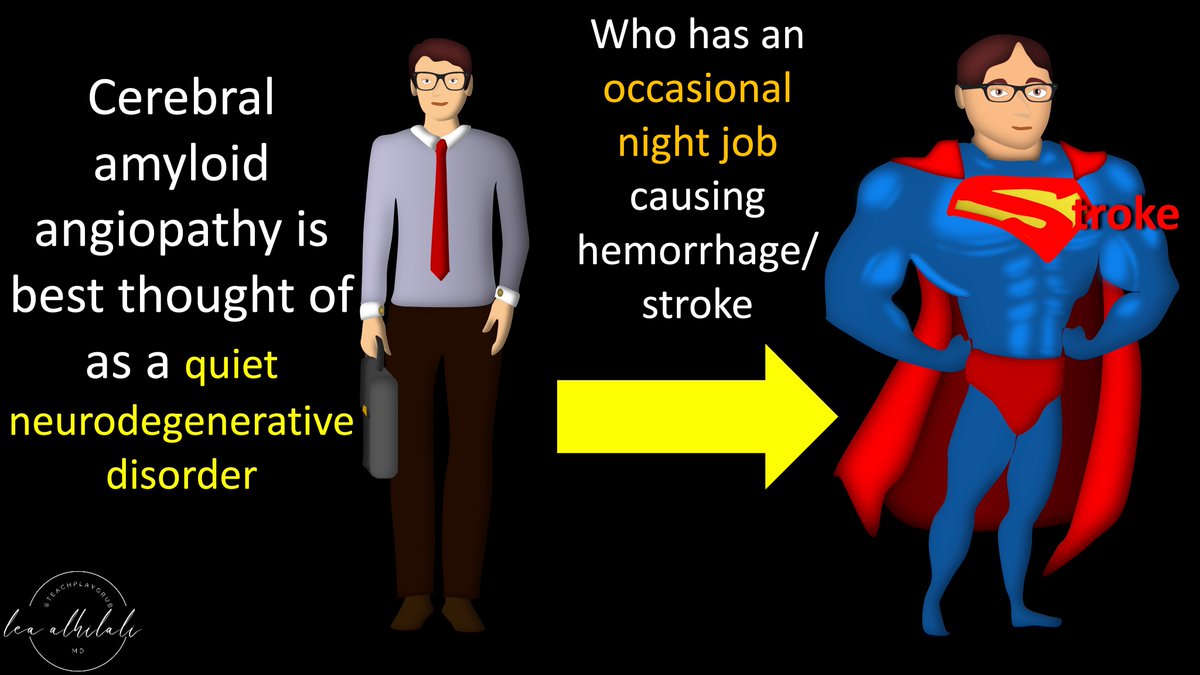
19/It causes both neurodegeneration & stroke by build up of amyloid proteins in the vessel wall & surrounding perivascular space.
In the vessel wall, it causes weakening that can lead to rupture & hemorrhage
In the perivascular space, it causes clogging & decreased clearance
In the vessel wall, it causes weakening that can lead to rupture & hemorrhage
In the perivascular space, it causes clogging & decreased clearance

20/It’s like having a bathtub you never clean
Perivascular spaces get clogged like a drain leading to clouded water (dementia).
And stagnant water is bad for the pipes so they rust & burst—just like vessels hemorrhage
So always mention microhemorrhage/signs of amyloid
Perivascular spaces get clogged like a drain leading to clouded water (dementia).
And stagnant water is bad for the pipes so they rust & burst—just like vessels hemorrhage
So always mention microhemorrhage/signs of amyloid

21/So now you know the important signs to look for when you are reading a study for vascular dementia.
You now can make all the findings so your report is a knock out!
You now can make all the findings so your report is a knock out!
• • •
Missing some Tweet in this thread? You can try to
force a refresh






















