I used #ChatGPT4 to appeal #Medicare claims to a judge. Here’s how a 🧵
Step one ask “As you are knowledgeable in medical billing, with your expert opinion give me the step by step process to appeal a Medicare claim at all levels”
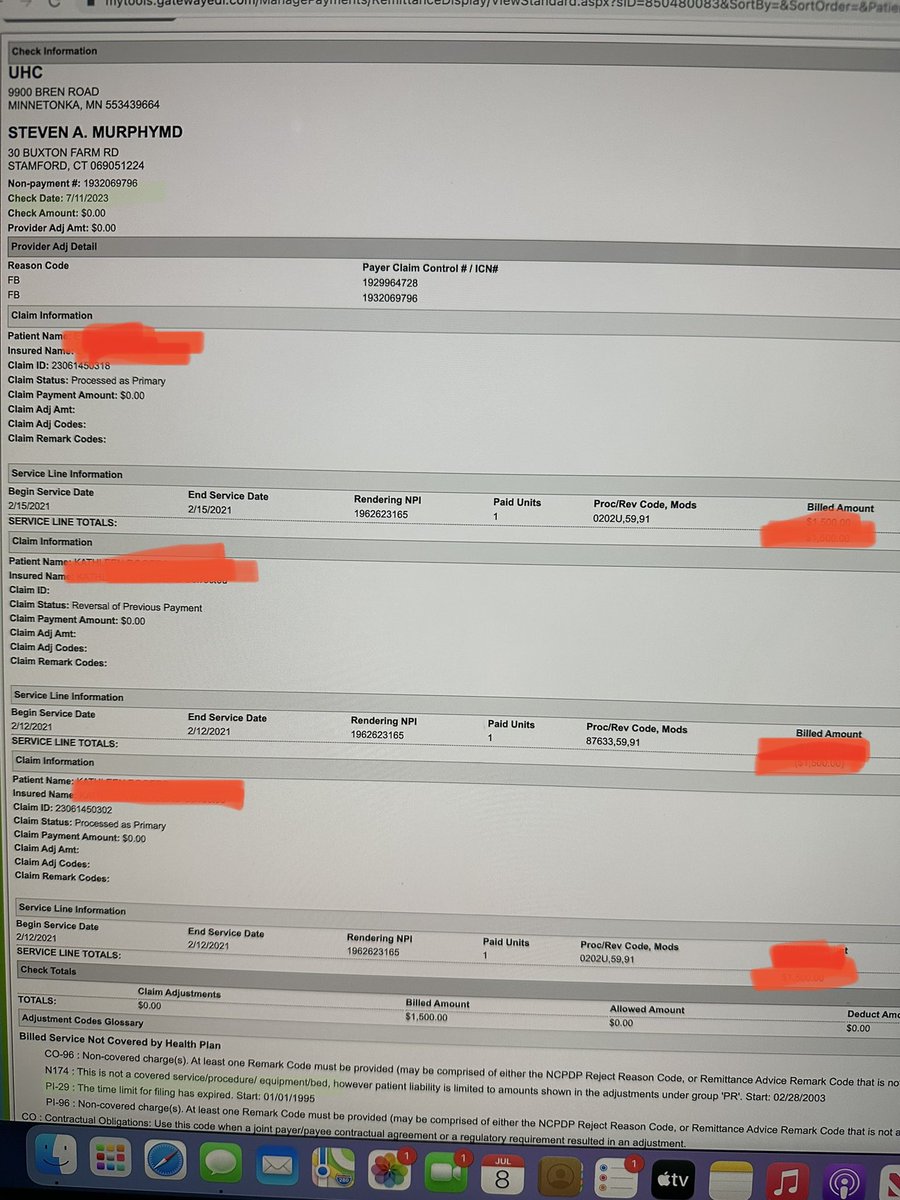
This will produce a list for each step. Most people don’t know, there are 5 levels of hell (appeal) for a denied Medicare claim. Who denies these? Well, NOT MEDICARE. They outsource it to low level business people AKA MEDICARE ADMINISTRATIVE CONTRACTORS (MACs)incentivized to deny claims. In this case @NGSMedicare You can find your MAC by looking on this website
You then need to fill out at appeal at their level. The MAC (step one) filling out a form CMS-20027 But beware you have a limited time to do this 120 days from the initial claim! Also beware the MAC can dismiss your request for appeal. So if the MAC slow walks your claim you may not have enough time to appeal. You can review the details in this 103 page chapter of the Medicare Claims Processing Manual cms.gov/Medicare/CMS-F…
Assuming you are successful and the MAC applies a redetermination it can be favorable (they’ll pay you) or unfavorable (they won’t) follow the thread for the next level of Hell (appeals) in our case we went past Level two. But if they say “UNFAVORABLE” you get to learn about the next acronym, the QIC…
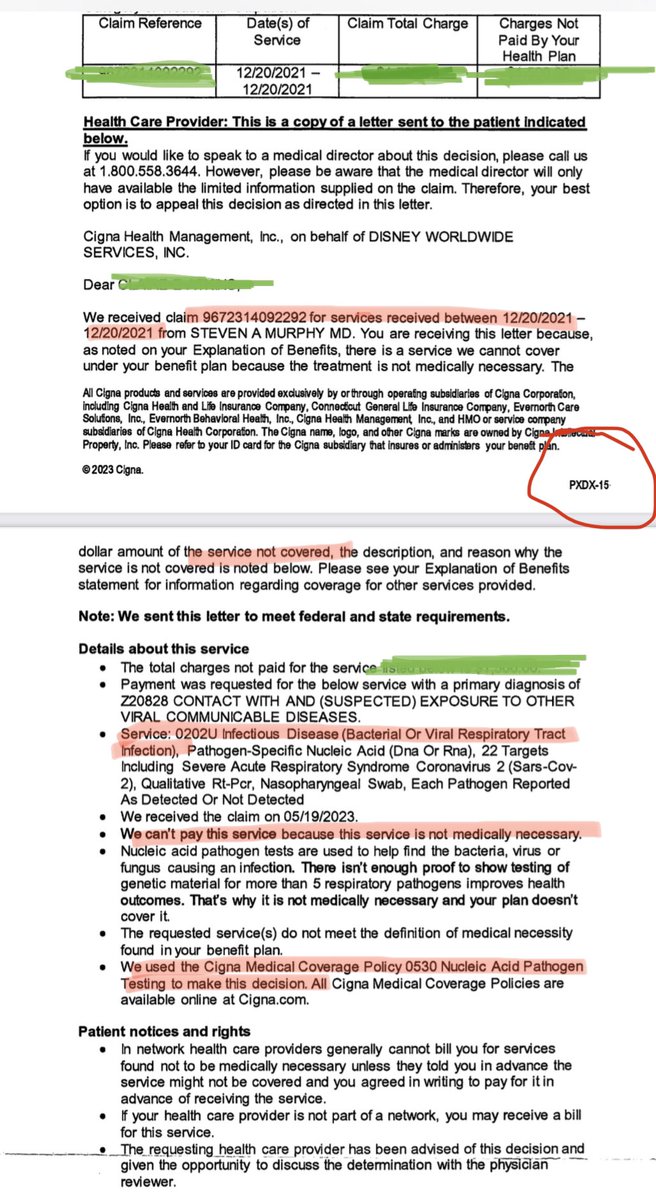
QIC stands for Qualified Independent Contractor. I often wonder, who “qualifies” them. And how do the become a “Contractor” rather than an elected and accountable administrator. Third they are anything but independent. They rely on the MAC. So how do you get to this special level?
FIRST BEWARE YOU ONLY HAVE 60 days (weekends included) to enter this special hell. You must find out WHO YOUR QIC IS. THEN You must fill out the CMS 20033 a second level appeal to yet another unelected unaccountable administrator. They then will issue their judgement.cms.gov/medicare/appea…
cms.gov/medicare/cms-f…

cms.gov/medicare/cms-f…
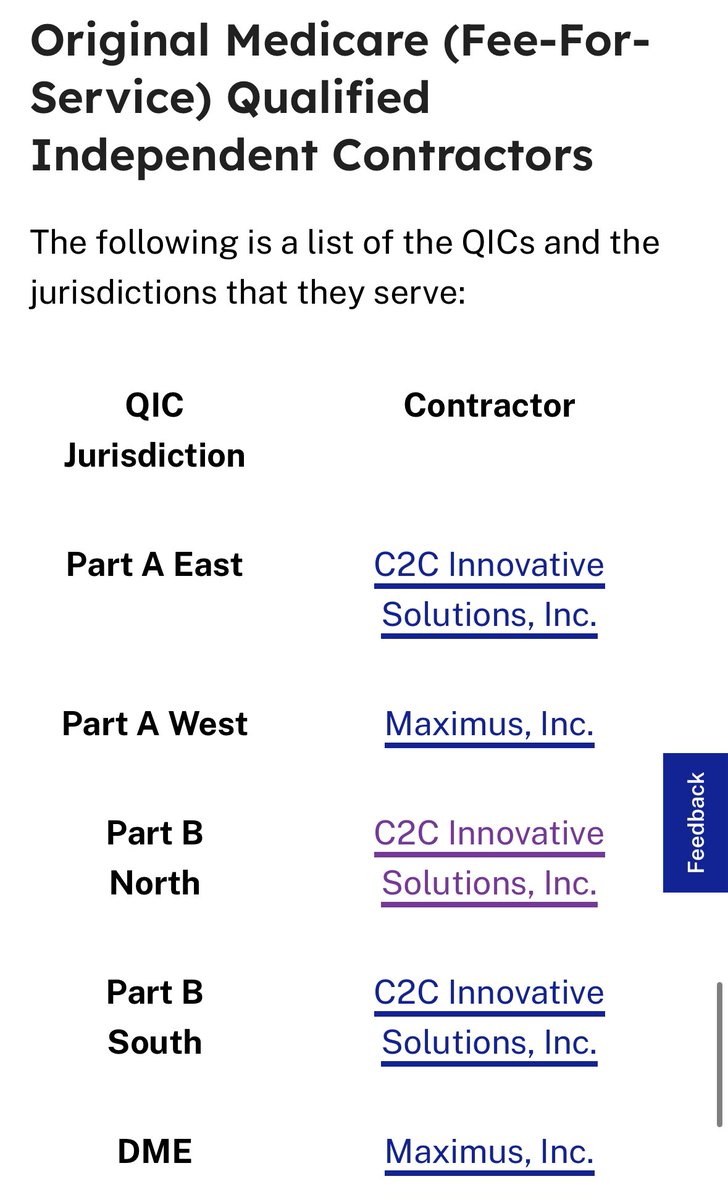
If that also is UNFAVORABLE AS OURS WAS, you then need to enlist a Medicare Administrative Law Judge. These are indeed the first Medicare Administrator you encounter with denials. Can you imagine? Well, the form for you is located here: and is always attached to the QIC “unfavorable” decisions. The chickens don’t like to call it a denial. Once you send the form, you will receive notification of request and a hearing date. ALWAYS REQUEST A HEARING, NEVER WAIVE THAT RIGHT!hhs.gov/sites/default/…
So what happens in a hearing? Takes listen. Even a judge doesn’t understand why a #RPP testing for #SARSCoV2 is a #covidtest.
So what happened today? I got this in the mail. It basically says, the two levels of unaccountable medicare administrators were wrong. Despite 2.5 years passing and bills coming due Medicare Administrators/Contractors didn’t care about following the law. 
“The Appellant provided the COVID-19 testing at issue during the global pandemic at a time when wide-spread vaccination was still not available.” “The record, however, shows that the COVID-19 (biofire) testing was furnished in accordance with CMS-5531-IFC” I’d like to thank @EdGainesIII @alexmeshkin @DrAlexUrology @mass_marion @JJWUrology and @GallaherCaren for all the moral support during this heated battle. You’ll have to follow this thread for the next 2 levels!

• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter