Summary thread of the oral-vascular-pulmonary model of #COVID-19 lung disease, why this is important and what to do about it.
Also potentially relevant in #LongCOVID
@SpringerNature review -
1/21 bit.ly/3ME7LtC

Also potentially relevant in #LongCOVID
@SpringerNature review -
1/21 bit.ly/3ME7LtC
2/21
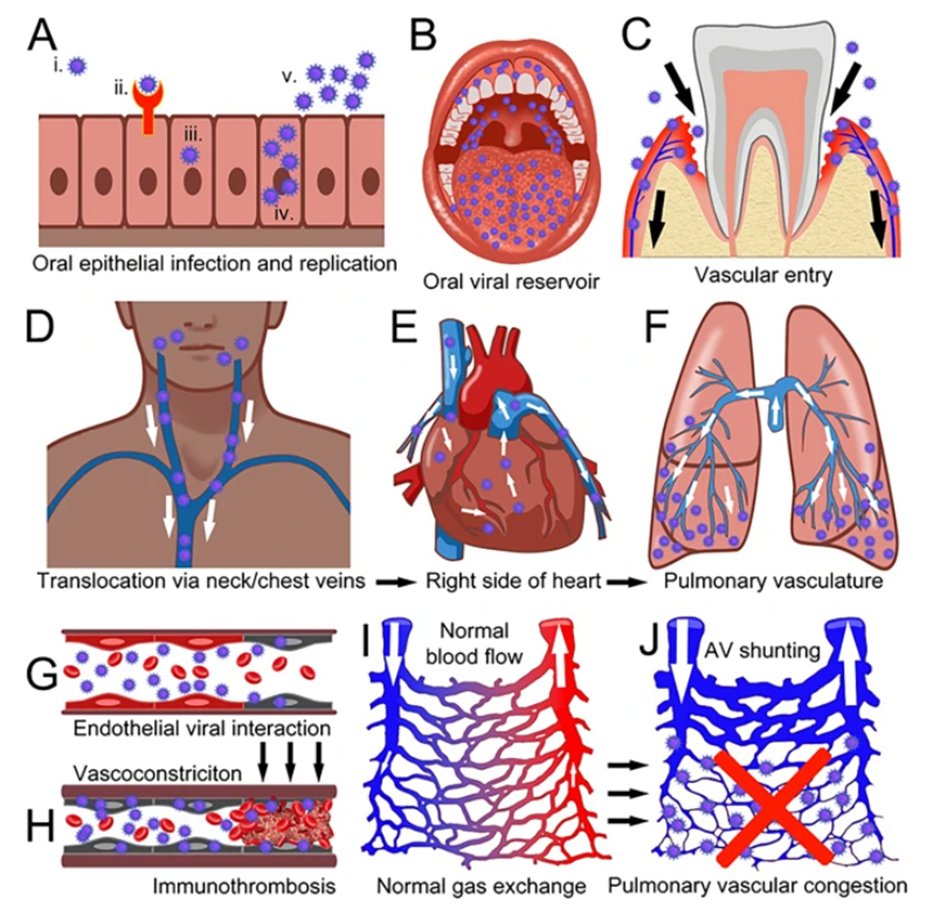
Initial viral infection of epithelial lining of the upper respiratory tract mucosa (nose and mouth) ...
Initial viral infection of epithelial lining of the upper respiratory tract mucosa (nose and mouth) ...

3/21
Viral replication (copying) and reservoir formation in the mouth (saliva, gingival crevicular fluid, dental plaque, periodontal tissues, minor salivary glands) ...
Viral replication (copying) and reservoir formation in the mouth (saliva, gingival crevicular fluid, dental plaque, periodontal tissues, minor salivary glands) ...

4/21
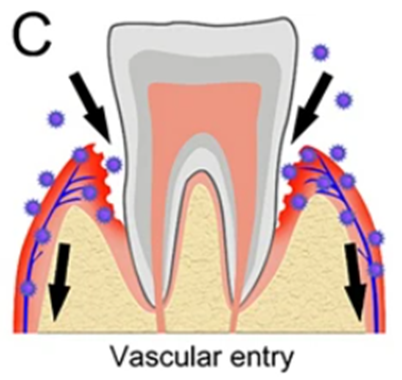
Transfer of viral particles/elements into the gingival venous drainage facilitated by micro-ulceration of the sulcular/pocket-lining epithelium due to gingivitis or periodontitis ...
Transfer of viral particles/elements into the gingival venous drainage facilitated by micro-ulceration of the sulcular/pocket-lining epithelium due to gingivitis or periodontitis ...
5/21
Intravascular passage of viral particles (or procoagulant viral elements) from the venous drainage of the mouth to the neck and chest veins (jugulars and superior vena cava) …
Intravascular passage of viral particles (or procoagulant viral elements) from the venous drainage of the mouth to the neck and chest veins (jugulars and superior vena cava) …

7/21
… into the pulmonary circulation via the pulmonary artery, dominantly in the highly vascularized gravity-dependent lung peripheries ...
… into the pulmonary circulation via the pulmonary artery, dominantly in the highly vascularized gravity-dependent lung peripheries ...

8/21
Direct interaction of viral particles/elements with endothelial cells of the pulmonary microvasculature, with intravascular pro-coagulant and pro-inflammatory viral interactions ...
Direct interaction of viral particles/elements with endothelial cells of the pulmonary microvasculature, with intravascular pro-coagulant and pro-inflammatory viral interactions ...

9/21
... leading to vasoconstriction, endothelial dysfunction and intravascular thrombosis/immunothrombosis
(Immunothrombosis = blood vessel inflammation with clotting within small blood vessels) ...
... leading to vasoconstriction, endothelial dysfunction and intravascular thrombosis/immunothrombosis
(Immunothrombosis = blood vessel inflammation with clotting within small blood vessels) ...

10/21
Damage to the normal capillary network in the lungs (normal blood flow and normal gas exchange) ...
Damage to the normal capillary network in the lungs (normal blood flow and normal gas exchange) ...

11/21
... with vascular congestion and impaired lung perfusion leading to lung damage, dominantly in the lung peripheries, with upstream pulmonary arteriovenous (AV) shunting and dilated proximal blood vessels ...
... with vascular congestion and impaired lung perfusion leading to lung damage, dominantly in the lung peripheries, with upstream pulmonary arteriovenous (AV) shunting and dilated proximal blood vessels ...

12/21
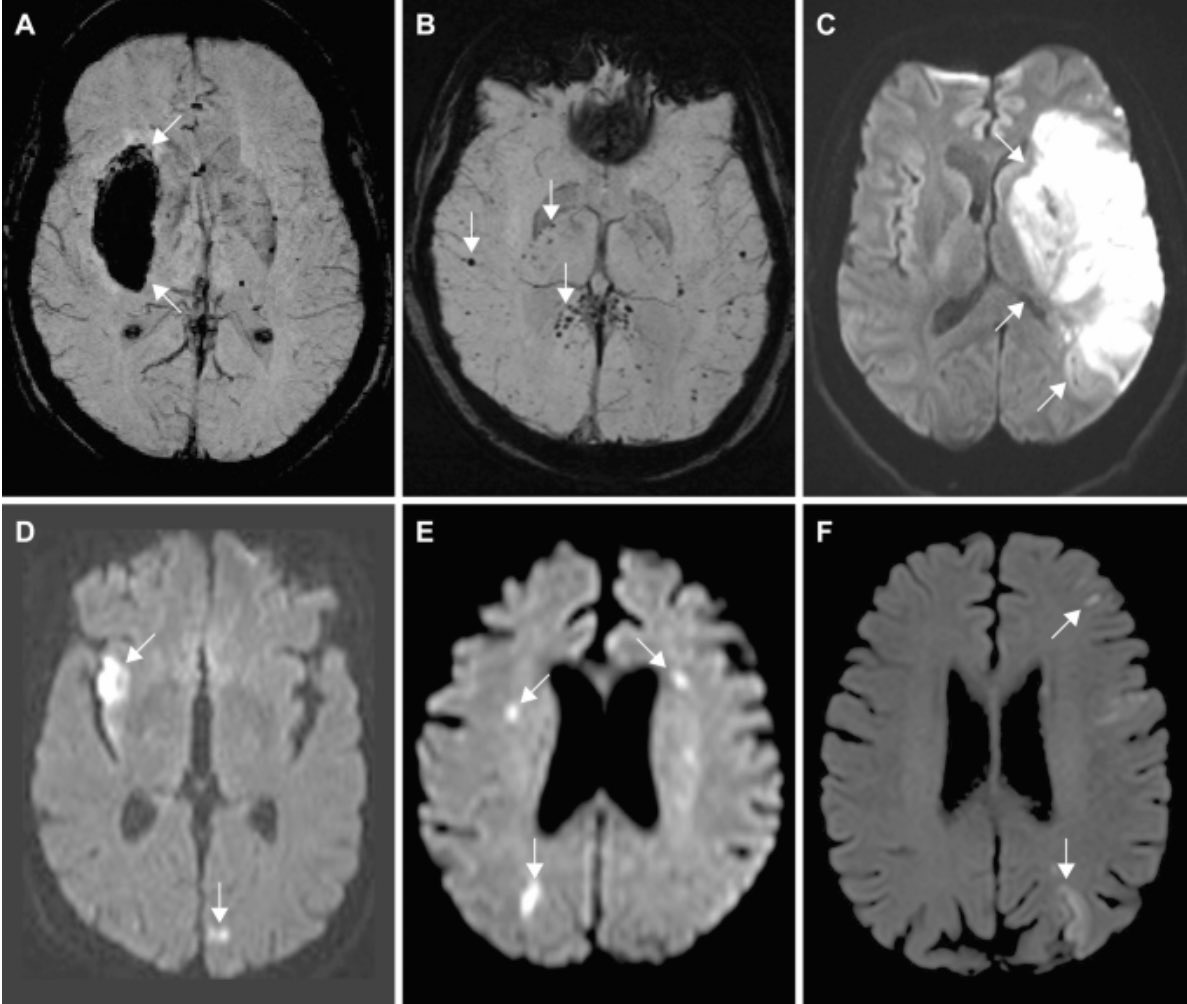
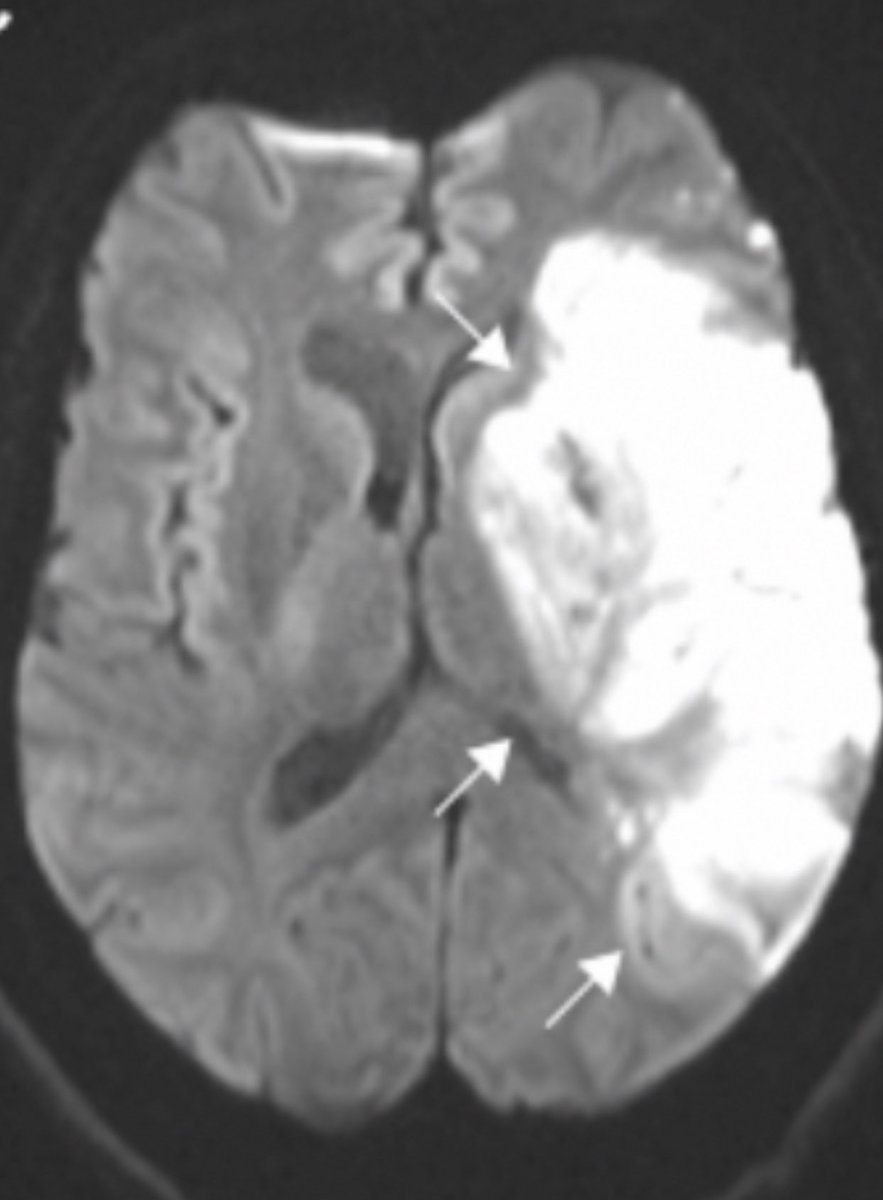
This model of disease development explains the vascular characteristics and vascular distribution of disease visible radiologically...
Green arrows = dilated/damaged blood vessels
Yellow arrows = lung tissue damage
(for this fig. please see original hypothesis - link below)
This model of disease development explains the vascular characteristics and vascular distribution of disease visible radiologically...
Green arrows = dilated/damaged blood vessels
Yellow arrows = lung tissue damage
(for this fig. please see original hypothesis - link below)

13/21
... and it explains the dominant histological/autopsy findings of pulmonary vascular congestion with clotting in the lungs at microscopic level.
doi.org/10.1016/S1473-…
... and it explains the dominant histological/autopsy findings of pulmonary vascular congestion with clotting in the lungs at microscopic level.
doi.org/10.1016/S1473-…
14/21
Read our full @SpringerNature review - here
👇👇👇👇👇👇👇
(Published November 3rd 2023) bit.ly/3ME7LtC

Read our full @SpringerNature review - here
👇👇👇👇👇👇👇
(Published November 3rd 2023) bit.ly/3ME7LtC

15/21
Original scientific hypothesis published April 2021 is accessible here
With thanks to my co-authors @l_chapple @dentalsurgeon__ and Carla Pontes (@ dr.carlapontes on Instagram) radiologymasterclass.co.uk/documents/the_…

Original scientific hypothesis published April 2021 is accessible here
With thanks to my co-authors @l_chapple @dentalsurgeon__ and Carla Pontes (@ dr.carlapontes on Instagram) radiologymasterclass.co.uk/documents/the_…

16/21
Why is this so important?
It means that it makes sense to care for your mouth if you have #COVID
Here is the mouth care guidance we offer our #COVID-19 patients @SalisburyNHS UK. It includes provision of an antiviral mouthwash against #SARS2
salisbury.nhs.uk/coronavirus/co…

Why is this so important?
It means that it makes sense to care for your mouth if you have #COVID
Here is the mouth care guidance we offer our #COVID-19 patients @SalisburyNHS UK. It includes provision of an antiviral mouthwash against #SARS2
salisbury.nhs.uk/coronavirus/co…

17/21
Based on evidence that specific mouthwash ingredients eradicate #SARS2 in vitro and make it undetectable in the mouth for a prolonged period
See this systematic review of CPC mouthwash I wrote with Italian colleagues @DrFDamico/@MMarmiere
et al
onlinelibrary.wiley.com/doi/full/10.11…
Based on evidence that specific mouthwash ingredients eradicate #SARS2 in vitro and make it undetectable in the mouth for a prolonged period
See this systematic review of CPC mouthwash I wrote with Italian colleagues @DrFDamico/@MMarmiere
et al
onlinelibrary.wiley.com/doi/full/10.11…
18/21
And evidence that use of mouthwash in the setting of acute COVID-19 reduces intensive care admission and mortality!
See this research paper published in @Nature
nature.com/articles/s4159…
And evidence that use of mouthwash in the setting of acute COVID-19 reduces intensive care admission and mortality!
See this research paper published in @Nature
nature.com/articles/s4159…
19/21
For a deeper dive please take a look at this presentation relating to the vascular nature of acute COVID-19 lung disease. (From November 2020)
For a deeper dive please take a look at this presentation relating to the vascular nature of acute COVID-19 lung disease. (From November 2020)
20/21
And this presentation which expands on the connections between oral health, COVID-19 and other diseases. (From March 2022)
And this presentation which expands on the connections between oral health, COVID-19 and other diseases. (From March 2022)
21/21
Here's my brief summary of how to care for the mouth
1 - Stop smoking/vaping
2 - Stop eating free sugar in all its forms (sugary/fruit drinks, cake, sweets)
3 - Learn how to brush your teeth properly
4 - Visit the dentist/hygienist preventatively (before things go wrong)
Here's my brief summary of how to care for the mouth
1 - Stop smoking/vaping
2 - Stop eating free sugar in all its forms (sugary/fruit drinks, cake, sweets)
3 - Learn how to brush your teeth properly
4 - Visit the dentist/hygienist preventatively (before things go wrong)
• • •
Missing some Tweet in this thread? You can try to
force a refresh