When "Mr SARS-COV-2" 🤢 meets "Mrs INFLUENZA" 🥶 (1st part)
This is a fascinating subject because we sometimes see, COVID-19 which seems blocking the progression of respiratory diseases, or sometimes giving the impression of contributing to their development. What about it?
This is a fascinating subject because we sometimes see, COVID-19 which seems blocking the progression of respiratory diseases, or sometimes giving the impression of contributing to their development. What about it?

2) In a first study, Japanese researchers investigated the impact of COVID-19 on influenza activity.
They compared the number of cases positive for COVID-19 and for influenza across 22 representative countries.
onlinelibrary.wiley.com/doi/10.1111/ir…

They compared the number of cases positive for COVID-19 and for influenza across 22 representative countries.
onlinelibrary.wiley.com/doi/10.1111/ir…

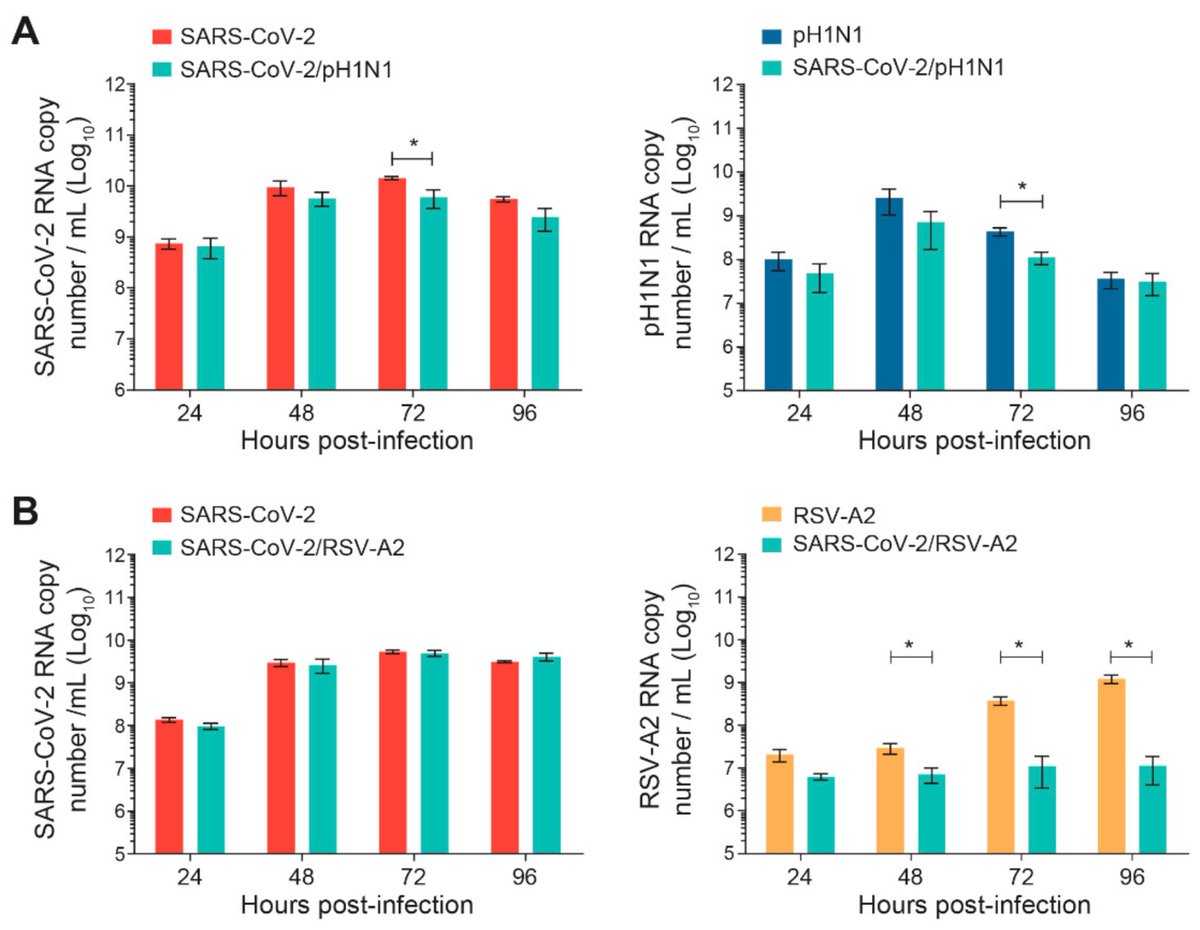
4) In this 2nd study, researchers showed that during simultaneous infection, SARS-CoV-2 interferes with RSV-A2 but not with A(H1N1)pdm09 replication. The prior infection of nasal airway epithelium with SARS-CoV-2 ...
mdpi.com/1999-4915/14/2…

mdpi.com/1999-4915/14/2…
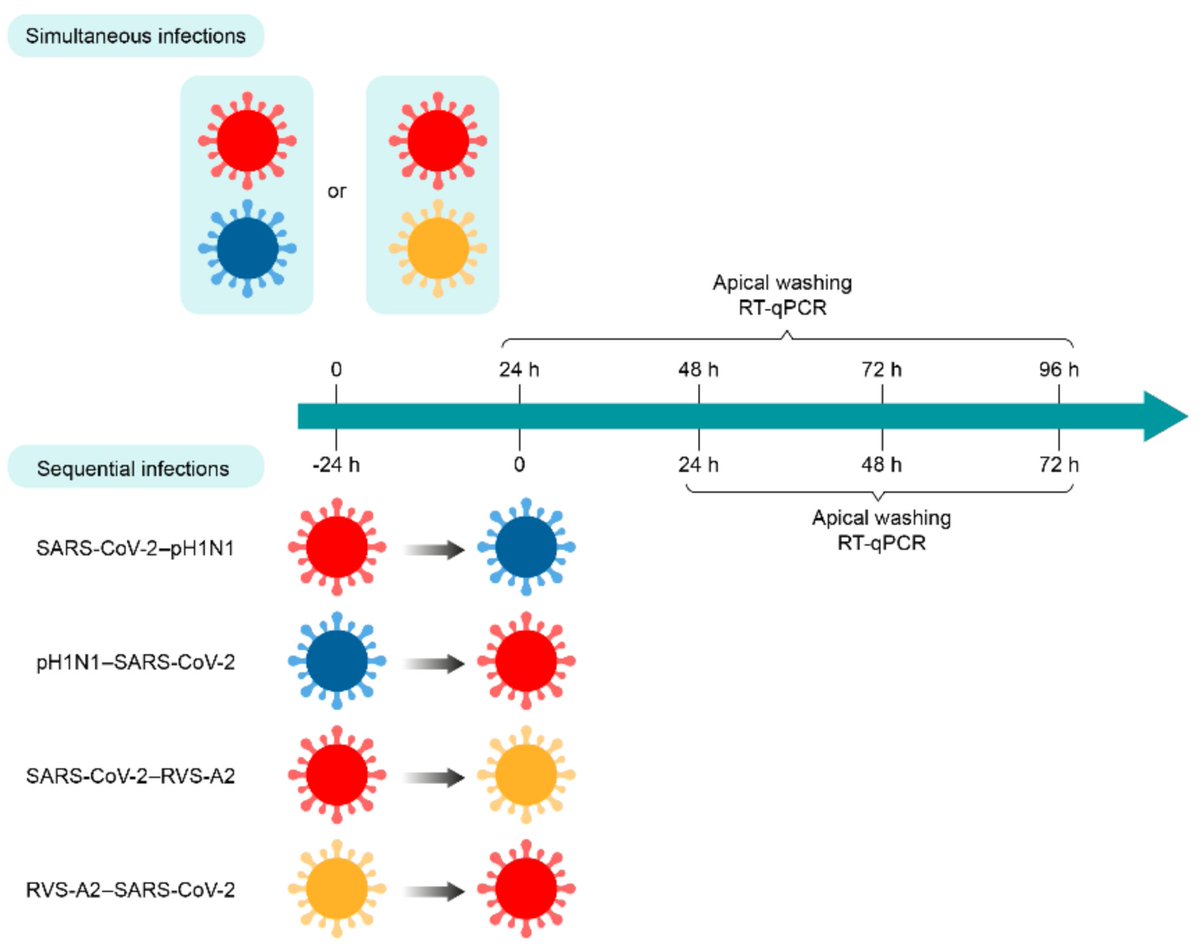
5) ... reduces the replication kinetics of both respiratory viruses. SARS-CoV-2 replication is decreased by a prior infection with A(H1N1)pdm09 but not with RSV-A2. 
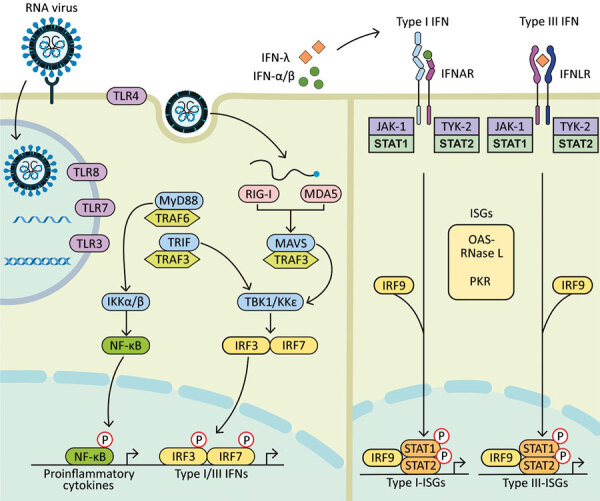
6) In this 3rd study, researchers explained that "a likely mechanism is the interferon response that could confer a temporary nonspecific immunity to the host."
pubmed.ncbi.nlm.nih.gov/35075991/

pubmed.ncbi.nlm.nih.gov/35075991/
• • •
Missing some Tweet in this thread? You can try to
force a refresh