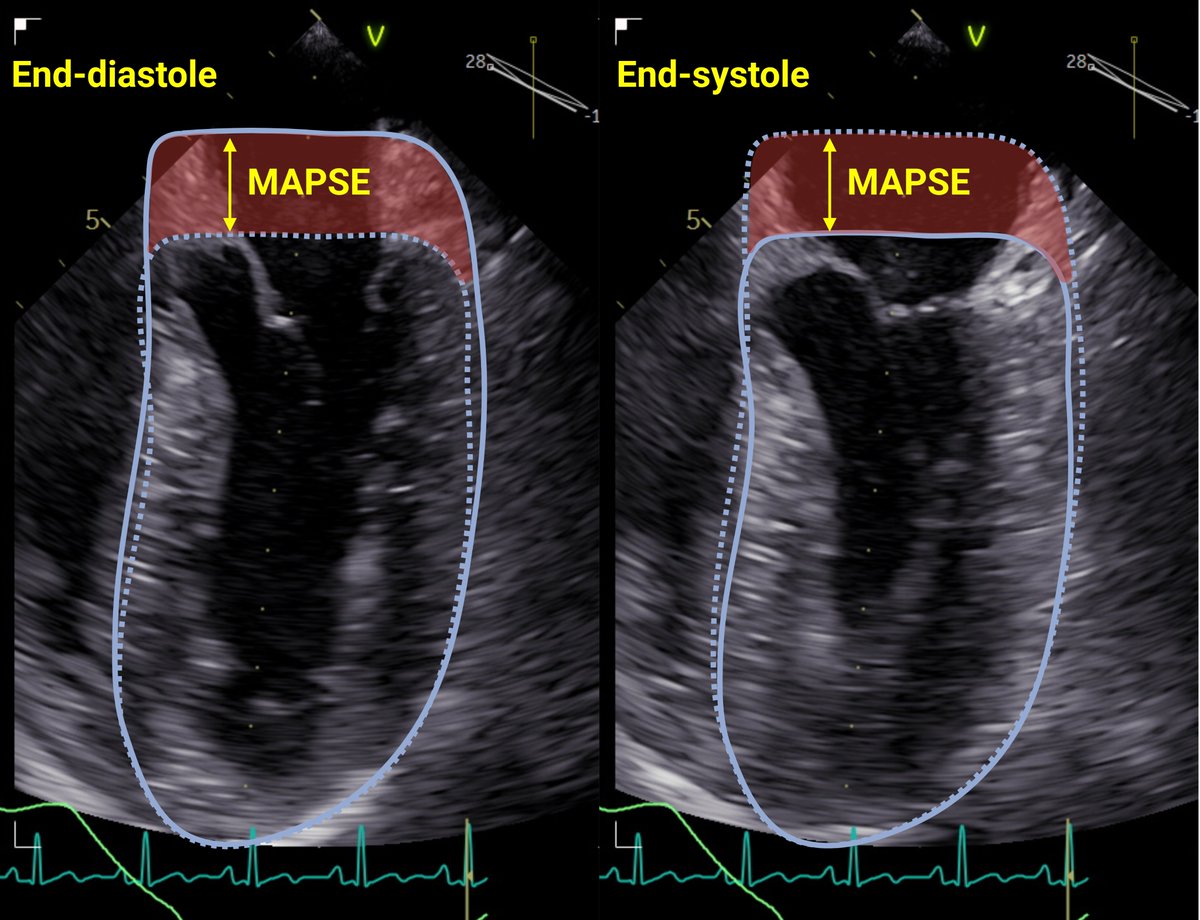
🚨Automatic measurement of LV function in #ICU is possible by automatic measurement of #MAPSE using TEE and AI #AutoMAPSE
🔓
1/🧵Still, many prefer EF for LV function. How does MAPSE compare to EF, and is MAPSE better?
#EchoFirst #POCUS #FOAMed rdcu.be/dxsEU

🔓
1/🧵Still, many prefer EF for LV function. How does MAPSE compare to EF, and is MAPSE better?
#EchoFirst #POCUS #FOAMed rdcu.be/dxsEU

2/ #MAPSE and EF are highly correlated. EF reflects SV/EDV, while MAPSE reflect SV/outer cross-sectional area.
Appreciate their relationship in this figure⬇️ doi.org/10.1152/ajphea…

Appreciate their relationship in this figure⬇️ doi.org/10.1152/ajphea…

3/ In heart failure with⬇️EF, the LV dilates, and both EF and #MAPSE falls from increases EDV and outer cross-sectional area.
The figure shows that both EF and MAPSE falls during LV dilatation. #CardioTwitter
The figure shows that both EF and MAPSE falls during LV dilatation. #CardioTwitter

4/ In heart failure with preserved EF, LV dysfunction from concentric remodeling reduces #MAPSE. Since EDV is maintained or even reduced, EF is unaffected.
The figure shows that MAPSE is reduced, but EF is maintained when EDV is reduced. #CardioTwitter
The figure shows that MAPSE is reduced, but EF is maintained when EDV is reduced. #CardioTwitter

5/ #MAPSE is reduced for both HFpEF and HFrEF. This was shown many years ago:
This relationship may also explain that MAPSE show superiority in #ICU: doi.org/10.1136/heart.…
doi.org/10.1186/1476-7…

This relationship may also explain that MAPSE show superiority in #ICU: doi.org/10.1136/heart.…
doi.org/10.1186/1476-7…

6/ In #ICU, EDV is commonly reduced from vasodilatation and hypovolemia. In this setting, EF is usually normal or even increased if ⬇️MAP. Despite a "hyperdynamic EF", hypovolemia decreases #MAPSE.
The figure shows reduced MAPSE and high EF during hypovolemia. #FOAMcc
The figure shows reduced MAPSE and high EF during hypovolemia. #FOAMcc

7/ SV is normal or increased during vasodilatation. This would tend to increase #MAPSE. Perhaps normal MAPSE in shock could aid the diagnosis of vasodilatation.
The figure shows how normal MAPSE during shock suggests vasodilatation. However, patient data is lacking.
The figure shows how normal MAPSE during shock suggests vasodilatation. However, patient data is lacking.

8/ EF by Simpson's is often unfeasible in #ICU, while #MAPSE is highly feasible. Thus, EF is usually qualitative, while MAPSE is quantitative, and quantitative data always offers more information and is necessary for true monitoring.
https://twitter.com/dritsyk/status/1751654442414276705
9/ #MAPSE is an underappreciated hero. #MAPSE measures LV longitudinal function (like GLS), and has shown better sensitivity than EF for detecting LV dysfunction.
...and #MAPSE can now be assessed automatically in #ICU😎📜
rdcu.be/dxsEU
...and #MAPSE can now be assessed automatically in #ICU😎📜
rdcu.be/dxsEU
https://twitter.com/dritsyk/status/1732144466499383795
unroll @threadreaderapp
• • •
Missing some Tweet in this thread? You can try to
force a refresh