The foods everyone tells you to eat but are wrecking your digestion.
FIBER - why it’s RUINING your gut, and CAUSING constipation:
FIBER - why it’s RUINING your gut, and CAUSING constipation:

EVERY SINGLE PERSON was CURED of every single digestive symptom, by completely removing fiber from their diets in this study.
Yes, even their constipation.
It sounds crazy, but it’s the truth.
Yes, even their constipation.
It sounds crazy, but it’s the truth.

These people entered the study with symptoms of straining, bowel movements less than every 3 days, distension, pain, bloating, and even anal bleeding.
They cut out all fiber: vegetables, cereals, fruits, wholemeal bread and brown rice for 2 weeks, but were allowed juices, white rice, white bread and animal proteins.
They cut out all fiber: vegetables, cereals, fruits, wholemeal bread and brown rice for 2 weeks, but were allowed juices, white rice, white bread and animal proteins.
Those who COMPLETELY STOPPED fiber intake went from one bowel movement every 4 days to one every single day.
Those put on a reduced fiber diet increased their bowel movements to one every 2 days compared with 1 every 4 days on the high fiber diet.
Those who continued with high dietary fiber intake had one bowel movement per WEEK.
Completely the opposite of the mainstream narrative.
Those put on a reduced fiber diet increased their bowel movements to one every 2 days compared with 1 every 4 days on the high fiber diet.
Those who continued with high dietary fiber intake had one bowel movement per WEEK.
Completely the opposite of the mainstream narrative.

Abdominal pain in the subjects was again, 100% CURED by completely cutting out ALL fiber.
They also cured their anal bleeding and bloating, and eliminated the need to strain for movements.
Every. Single. Person.
Do you understand how insane this is?
Why is no one talking about this?
They also cured their anal bleeding and bloating, and eliminated the need to strain for movements.
Every. Single. Person.
Do you understand how insane this is?
Why is no one talking about this?

People on a reduced fiber diet improved all of their digestive symptoms as well.
Nearly all of these patients chose to continue on a reduced fiber diet, with most maintaining the zero fiber diet.
A handful continued on a high fiber diet, for various reasons including being vegetarians or inability to stop consuming dietary fiber "due to constant media and peer pressure to increase dietary fiber."
The brainwashing runs deep.
Nearly all of these patients chose to continue on a reduced fiber diet, with most maintaining the zero fiber diet.
A handful continued on a high fiber diet, for various reasons including being vegetarians or inability to stop consuming dietary fiber "due to constant media and peer pressure to increase dietary fiber."
The brainwashing runs deep.
Another study showed that a fiber restricted diet (<10 grams per day) was again a life changing therapy for IBS patients.
HALF of IBS patients reported SIGNIFICANT improvement (>60% improvement), with 9% reporting COMPLETE RESOLUTION of all symptoms
Diarrhea, gas, bloating, pain, and yes, even constipation.

HALF of IBS patients reported SIGNIFICANT improvement (>60% improvement), with 9% reporting COMPLETE RESOLUTION of all symptoms
Diarrhea, gas, bloating, pain, and yes, even constipation.


This is repeatedly found in the research, yet no doctor seems to know it.
The few that do have noted in clinical practice that increasing fiber can CAUSE symptoms.
HALF of people refuse to do it because of the symptoms it causes.
“Patients’ compliance with the use of fiber supplements is poor because of their side effects, which include flatulence, distention, bloating, and unpleasant taste.”
"Compliance with increasing dietary fiber and use of fiber supplements, however, is estimated to be as low as 50%"
“Many patients with more severe constipation get worse symptoms when increasing dietary fiber intake.”

The few that do have noted in clinical practice that increasing fiber can CAUSE symptoms.
HALF of people refuse to do it because of the symptoms it causes.
“Patients’ compliance with the use of fiber supplements is poor because of their side effects, which include flatulence, distention, bloating, and unpleasant taste.”
"Compliance with increasing dietary fiber and use of fiber supplements, however, is estimated to be as low as 50%"
“Many patients with more severe constipation get worse symptoms when increasing dietary fiber intake.”


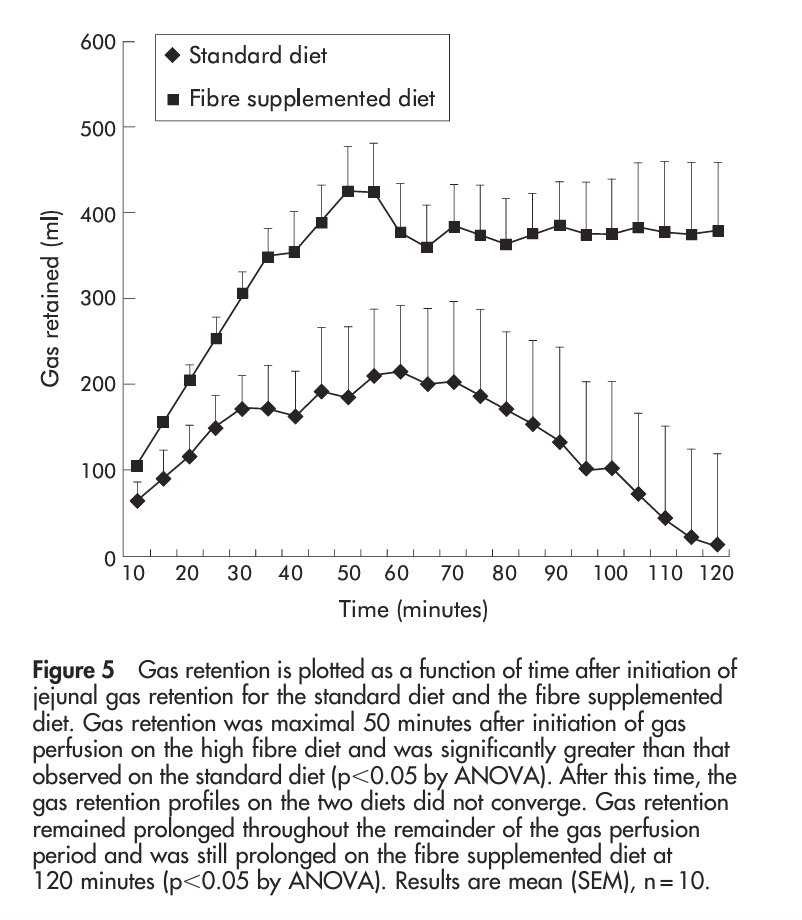
Soluble dietary fiber is fermented by gut bacteria, which produce gasses like hydrogen and carbon dioxide.
This happens even in gut bacteria that are considered “good.”
More classically “bad” bacteria produce methane gas.
This gas buildup puts pressure on different parts of the gut, leading to pain, bloating and distention.
Methane is also a well known inhibitor of gut motility, being ubiquitous in constipation.
This is at least one way that it can cause problems.
This happens even in gut bacteria that are considered “good.”
More classically “bad” bacteria produce methane gas.
This gas buildup puts pressure on different parts of the gut, leading to pain, bloating and distention.
Methane is also a well known inhibitor of gut motility, being ubiquitous in constipation.
This is at least one way that it can cause problems.

One study showed that a reduced fiber diet dramatically improved gut symptoms and gas production:
“maximum rates of gas excretion (mainly hydrogen) were much greater in IBS patients than in controls.
On an exclusion diet, which significantly improved symptoms, gas excretion (hydrogen and methane) fell dramatically, but no such change occurred in controls.
Our findings are consistent with the suggestion that the IBS may be caused by abnormal colonic fermentation”
“maximum rates of gas excretion (mainly hydrogen) were much greater in IBS patients than in controls.
On an exclusion diet, which significantly improved symptoms, gas excretion (hydrogen and methane) fell dramatically, but no such change occurred in controls.
Our findings are consistent with the suggestion that the IBS may be caused by abnormal colonic fermentation”

Another study on IBS patients gave them either antibiotics or fiber free diets to reduce bacterial driven fermentation.
Again, the reduction of fiber reduced gas and improved their symptoms.
“Antibiotics significantly reduced the 24-hr excretion of hydrogen and total gas and the maximum rate of gas excretion, as did a no-fiber diet, with a significant improvement in abdominal symptoms.”
“IBS may be associated with rapid excretion of gaseous products of fermentation, whose reduction may improve symptoms.”
Again, the reduction of fiber reduced gas and improved their symptoms.
“Antibiotics significantly reduced the 24-hr excretion of hydrogen and total gas and the maximum rate of gas excretion, as did a no-fiber diet, with a significant improvement in abdominal symptoms.”
“IBS may be associated with rapid excretion of gaseous products of fermentation, whose reduction may improve symptoms.”

A review of 20 studies showed that while insoluble fiber made stool bigger and increased colonic motility, these individuals still experienced less frequent stools and slower bowel movements compared to those without constipation, regardless of fiber consumption.
The use of fiber supplements resulted in an increase of only 1 to 1.4 bowel movements per week!
Pretty negligible in the grand scheme of things.

The use of fiber supplements resulted in an increase of only 1 to 1.4 bowel movements per week!
Pretty negligible in the grand scheme of things.


Another review found that fiber barely affected overall symptom relief and constipation for IBS.
The impact of soluble versus insoluble fiber on IBS symptoms varies, but insoluble fiber sometimes exacerbates symptoms.
In general fiber tends to WORSEN abdominal pain.
The impact of soluble versus insoluble fiber on IBS symptoms varies, but insoluble fiber sometimes exacerbates symptoms.
In general fiber tends to WORSEN abdominal pain.

Insoluble fiber literally works by being an indigestible irritant.
Its actions can be mimicked by eating PLASTIC.
No joke.
If your intestine is sensitive, this is possibly the worst thing you can do!
Its actions can be mimicked by eating PLASTIC.
No joke.
If your intestine is sensitive, this is possibly the worst thing you can do!

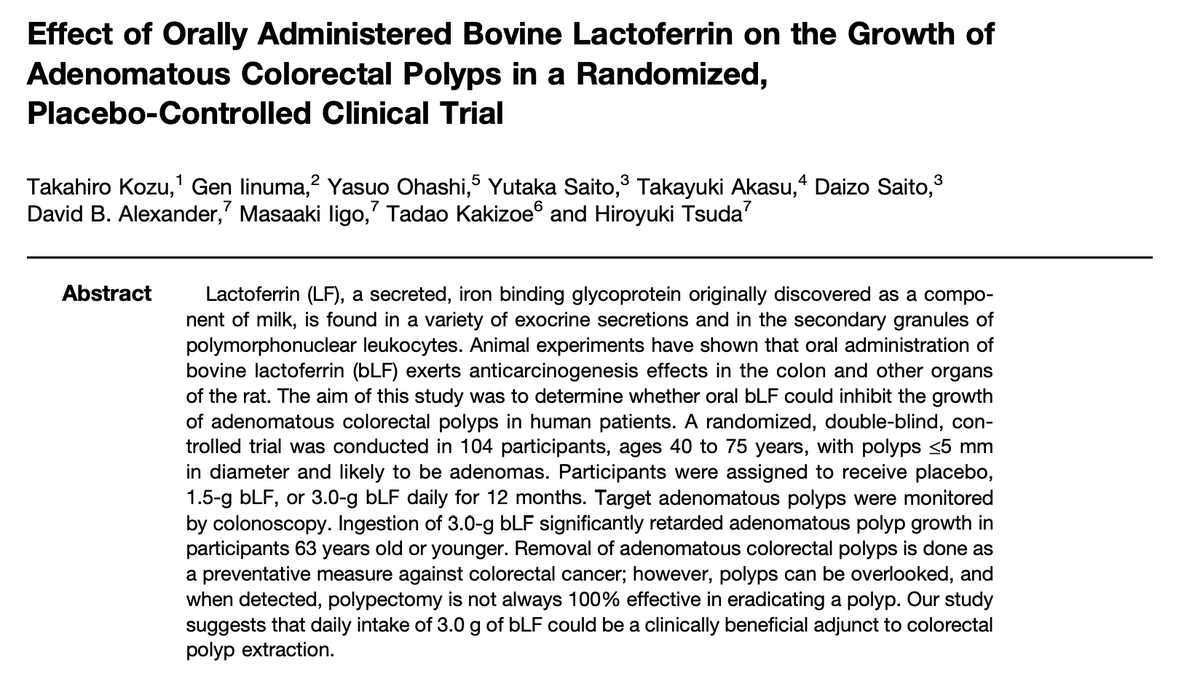
Avoiding all fiber is used clinically to induce REMISSION even for YEARS in inflammatory digestive conditions like Crohn’s disease, being as effective as some of the top drugs.
It is also known that a low fiber is the best option for patients experiencing pain during diverticulitis, a condition of an inflamed gut.



It is also known that a low fiber is the best option for patients experiencing pain during diverticulitis, a condition of an inflamed gut.




Even the major institutions all acknowledge that restricting dietary fiber is critical in treating these severe gut issues.
That’s because fiber is either fermentable and contributes to the bacterial inflammation, or it is a direct irritant.
Avoiding it when your gut is compromised is crucial.


That’s because fiber is either fermentable and contributes to the bacterial inflammation, or it is a direct irritant.
Avoiding it when your gut is compromised is crucial.



If you have IBS or other gut problems, your odds of getting Crohn’s, Diverticulitis or Ulcerative Colitis skyrockets, up to a 15 FOLD increased risk!
These serious conditions are simply the more advanced version of gut problems your doctors will tell you not to worry about.
In BOTH cases, REDUCING or even eliminating fiber can be a Godsend.
These serious conditions are simply the more advanced version of gut problems your doctors will tell you not to worry about.
In BOTH cases, REDUCING or even eliminating fiber can be a Godsend.

Adding fiber to the diet remains by far the most recommended dietary treatment in clinical practice.
A massive patient survey showed that up to 76% of all IBS patients are given this suggestion by their doctors, yet just 5-13% of patients report high satisfaction.
“today, gastroenterologists are more likely to see patients who have failed a trial of high-fiber diet than those who take insufficient fiber”



A massive patient survey showed that up to 76% of all IBS patients are given this suggestion by their doctors, yet just 5-13% of patients report high satisfaction.
“today, gastroenterologists are more likely to see patients who have failed a trial of high-fiber diet than those who take insufficient fiber”




People have this idea that constipation is the absence of stool production, leading to the erroneous belief that more feces would ease defecation.
In reality, constipation involves difficulty in passing stool already present in the rectum, and increasing fiber intake, which enlarges fecal bulk, does not alleviate this issue.
It does the exact opposite, exacerbating the problem by increasing stool size and bulk.
In reality, constipation involves difficulty in passing stool already present in the rectum, and increasing fiber intake, which enlarges fecal bulk, does not alleviate this issue.
It does the exact opposite, exacerbating the problem by increasing stool size and bulk.

Researchers have ridiculed the idea of fiber curing constipation, saying
“The role of dietary fiber in constipation is analogous to cars in traffic congestion. The only way to alleviate slow traffic would be to decrease the number of cars and to evacuate the remaining cars quickly. Should we add more cars, the congestion would only be worsened. ”
“The role of dietary fiber in constipation is analogous to cars in traffic congestion. The only way to alleviate slow traffic would be to decrease the number of cars and to evacuate the remaining cars quickly. Should we add more cars, the congestion would only be worsened. ”

It’s even stated in textbooks that fiber can enhance peristalsis, the proper contractions of the upper GI tract, but there is no experimental evidence to support this.
Insoluble fiber is suspended in fluid for most of digestion, so it cannot initiate this process by bulking.
Insoluble fiber is suspended in fluid for most of digestion, so it cannot initiate this process by bulking.
In fact, fiber has been shown to IMPAIR proper motility by increasing gas retention, which leads to uncomfortable bloating, gut pain and distention.




Stool becomes solid only at the very end of the colon.
At this stage, particularly for individuals suffering from constipation, an increase in stool volume can exacerbate evacuation issues.
Therefore, it does not make sense to aim for larger and more voluminous stools in patients with idiopathic constipation or in anyone who experiences difficulty in stool passage.
At this stage, particularly for individuals suffering from constipation, an increase in stool volume can exacerbate evacuation issues.
Therefore, it does not make sense to aim for larger and more voluminous stools in patients with idiopathic constipation or in anyone who experiences difficulty in stool passage.

There’s also this idea that fiber makes stools less dry, yet evidence suggests that stool moisture remains constant regardless of fiber or water intake.
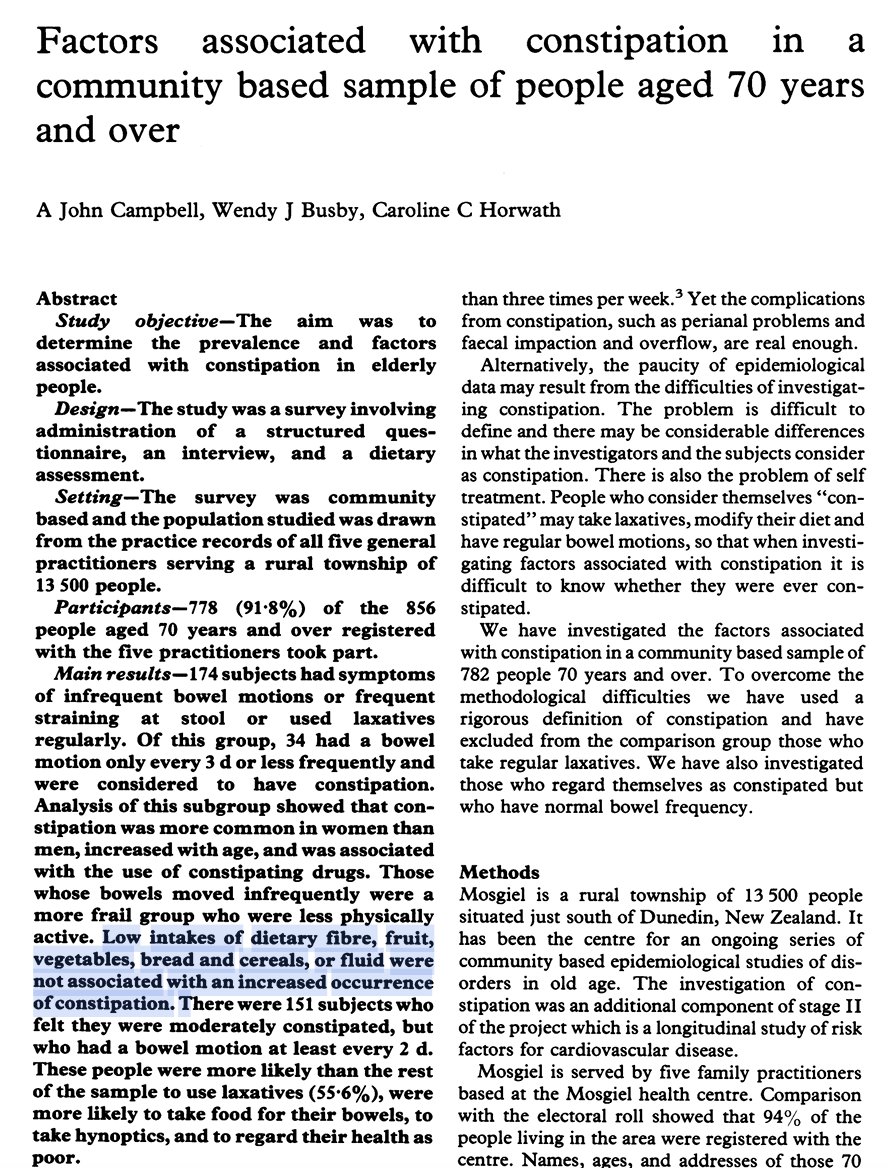
People with chronic constipation have, on average, the same dietary fiber intake as those without it.
It's myth after myth after myth.

People with chronic constipation have, on average, the same dietary fiber intake as those without it.
It's myth after myth after myth.

How could this all be though? All I hear is that fiber is good for the gut!
It is true that soluble fiber can be beneficial by serving as substrate for gut bacteria, which in turn feeds the metabolism of the colon and creates a more robust environment.
It’s also true that insoluble fiber can increase colonic motility and bowel movements / bulk.
HOWEVER…
It is true that soluble fiber can be beneficial by serving as substrate for gut bacteria, which in turn feeds the metabolism of the colon and creates a more robust environment.
It’s also true that insoluble fiber can increase colonic motility and bowel movements / bulk.
HOWEVER…

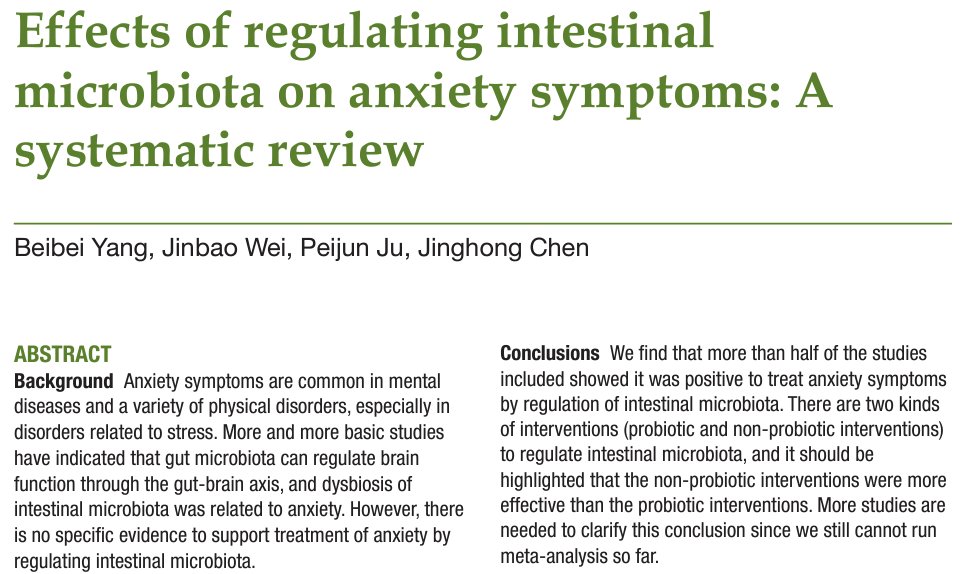
If you suffer from a chronic gut issue, you more than likely ALREADY have a bacterial overgrowth.
Bloating, pain and gas are caused by the buildup of excess stool and gasses produced by excess bacterial growth.
Diarrhea is a classic sign of bacterial overgrowth as well, while many bacterial metabolites can slow motility and lead to constipation.
You also ALREADY have excess fecal material and impaired motility.
In this scenario, eating highly fermentable foods, i.e soluble FIBER or resistant starch, is probably the WORST thing you can do.
The LAST thing you want to do is give more fuel to the bacterial fiber.
Bloating, pain and gas are caused by the buildup of excess stool and gasses produced by excess bacterial growth.
Diarrhea is a classic sign of bacterial overgrowth as well, while many bacterial metabolites can slow motility and lead to constipation.
You also ALREADY have excess fecal material and impaired motility.
In this scenario, eating highly fermentable foods, i.e soluble FIBER or resistant starch, is probably the WORST thing you can do.
The LAST thing you want to do is give more fuel to the bacterial fiber.

The increased sensitivity, bloating, discomfort and pain can all be driven directly by SEROTONIN, which is produced in response to excess bacterial growth:
https://x.com/Outdoctrination/status/1678072420190547968?s=20
Now, do I think this means that everyone should be on a zero fiber diet forever, or that all of these problems are due to fiber intake? No.
It simply means that if you struggle with these issues, then one of the lowest hanging fruits is to cut out highly fermentable (soluble fiber) and irritating (insoluble) fibers.
As you address the underlying problem (bacterial overgrowth and impaired motility / immunity), then continuing to add in these foods as tolerated is the optimal solution in the long run.
Once you can tolerate them, then I'd agree that adding in more fiber is likely beneficial for maintaining digestive function, but NOT for repairing a very broken gut.
You should be able to tolerate many, including fibrous, foods, but if your gut is compromised, then you’ll need to be careful about how you reintroduce these.
It simply means that if you struggle with these issues, then one of the lowest hanging fruits is to cut out highly fermentable (soluble fiber) and irritating (insoluble) fibers.
As you address the underlying problem (bacterial overgrowth and impaired motility / immunity), then continuing to add in these foods as tolerated is the optimal solution in the long run.
Once you can tolerate them, then I'd agree that adding in more fiber is likely beneficial for maintaining digestive function, but NOT for repairing a very broken gut.
You should be able to tolerate many, including fibrous, foods, but if your gut is compromised, then you’ll need to be careful about how you reintroduce these.
Gut issues can be quite difficult to figure out.
That’s why we started a premium consulting platform.
We have a team of practitioners collaborating to help folks looking to optimize their gut health.
Schedule a free consultation here to hear more! prism.miami
That’s why we started a premium consulting platform.
We have a team of practitioners collaborating to help folks looking to optimize their gut health.
Schedule a free consultation here to hear more! prism.miami
Thank you for reading along. Hopefully this was helpful and you can use this info to improve your health.
Toss us a RT if you’re so inclined, helps us a lot.
Be sure to check out all of our content and supplements, as well as ways to donate, over at lnk.bio/analyze.and.op…
Toss us a RT if you’re so inclined, helps us a lot.
Be sure to check out all of our content and supplements, as well as ways to donate, over at lnk.bio/analyze.and.op…
• • •
Missing some Tweet in this thread? You can try to
force a refresh