A new research finds a direct correlation between HDL Cholesterol (HDL-C) & ferritin levels and the severity of #LongCOVID. The decline in HDL-C levels & the rise in ferritin levels in patients could potentially play a role in persistence & progression of longCOVID symptoms 1/ 
The research findings suggest that HDL-C and ferritin levels could serve as crucial markers and therapeutic targets, opening new avenues for treatment strategies aimed at mitigating the long-term effects of the disease. 2/
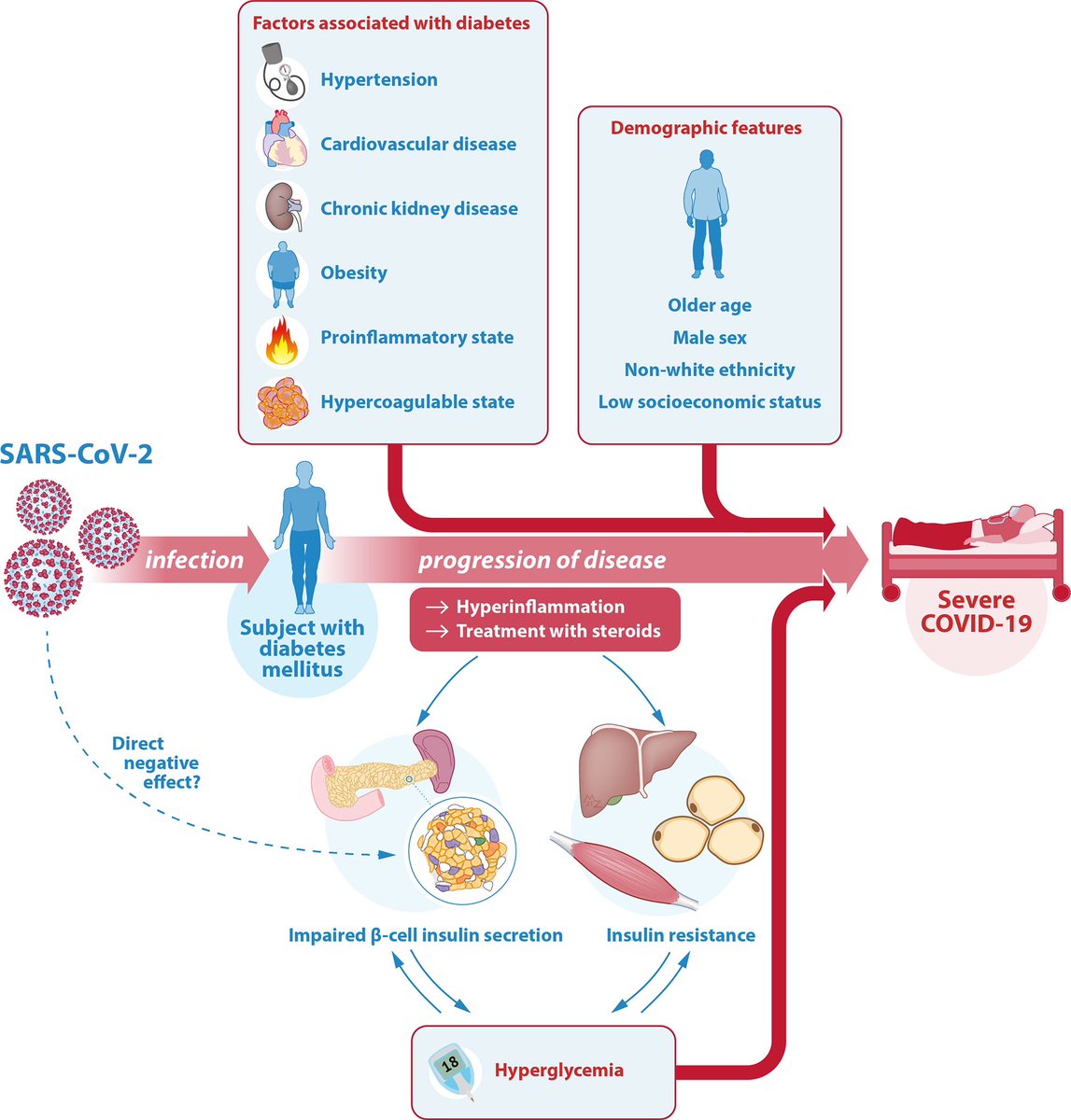
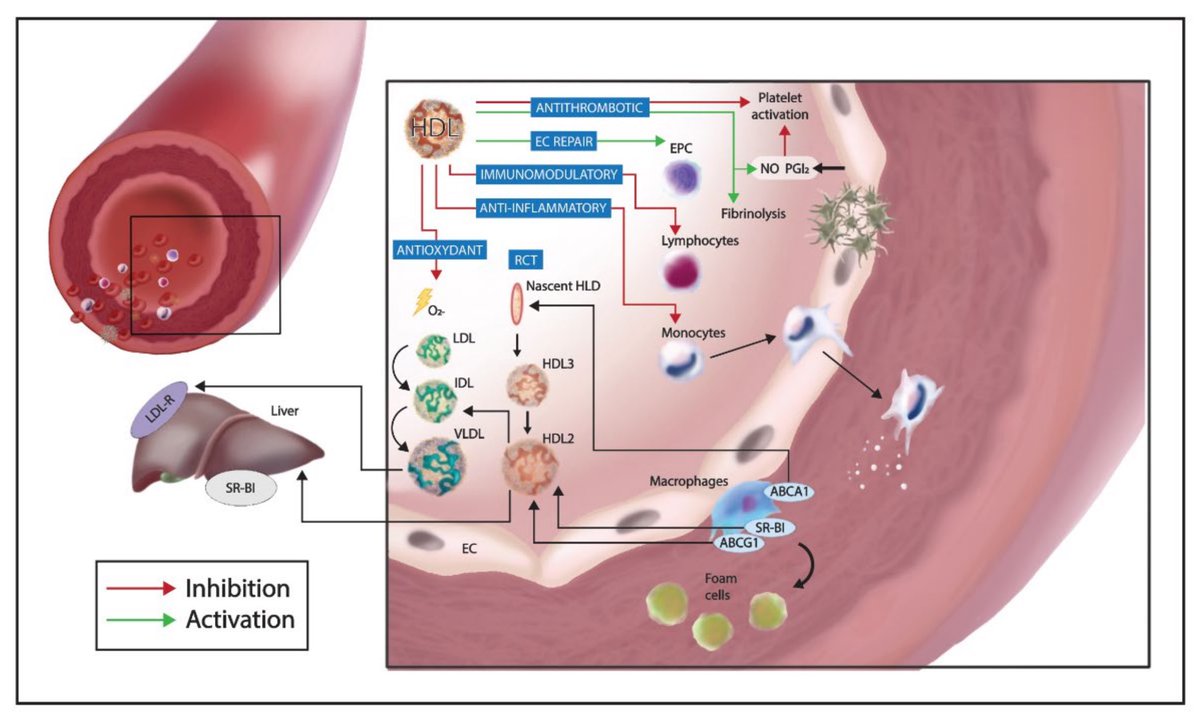
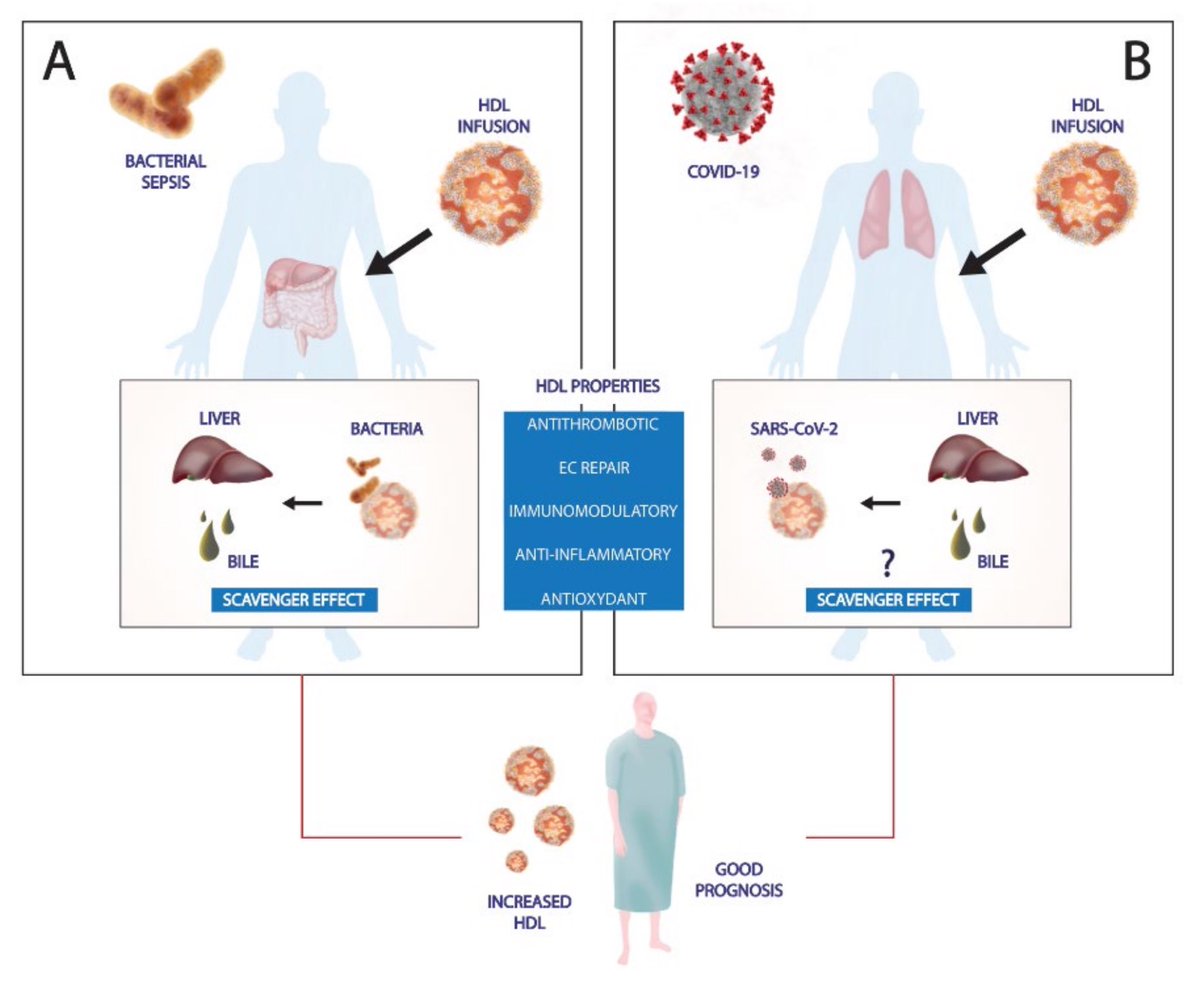
The observed correlation between diminished levels of HDL-C, the severity of COVID-19, and its prolonged course might be explained by HDL-C's function as a modulator of the immune response. 3/ 
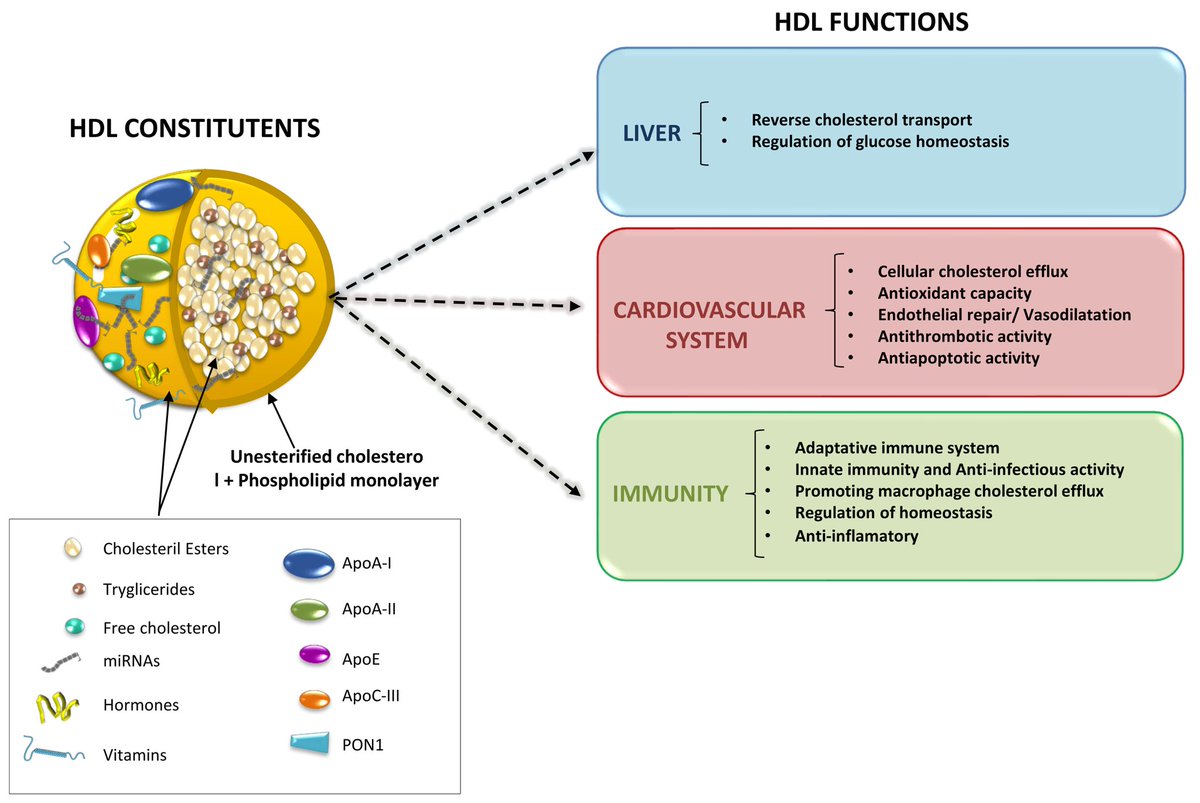
This includes its roles as an anti-inflammatory, antioxidant, and antiatherogenic agent, particularly vital during the heightened inflammatory response triggered by the virus. 4/ 
Investigating HDL-C's utility beyond its conventional role in cholesterol transport is crucial for a comprehensive understanding of COVID-19 and its secondary health effects, such as longCOVID. 5/
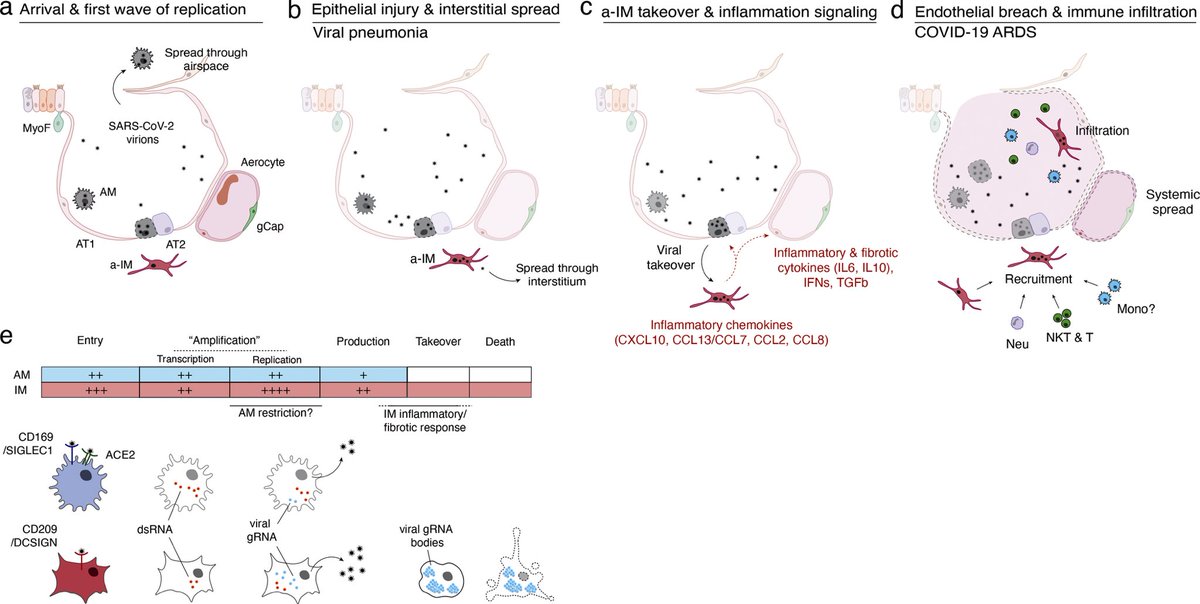
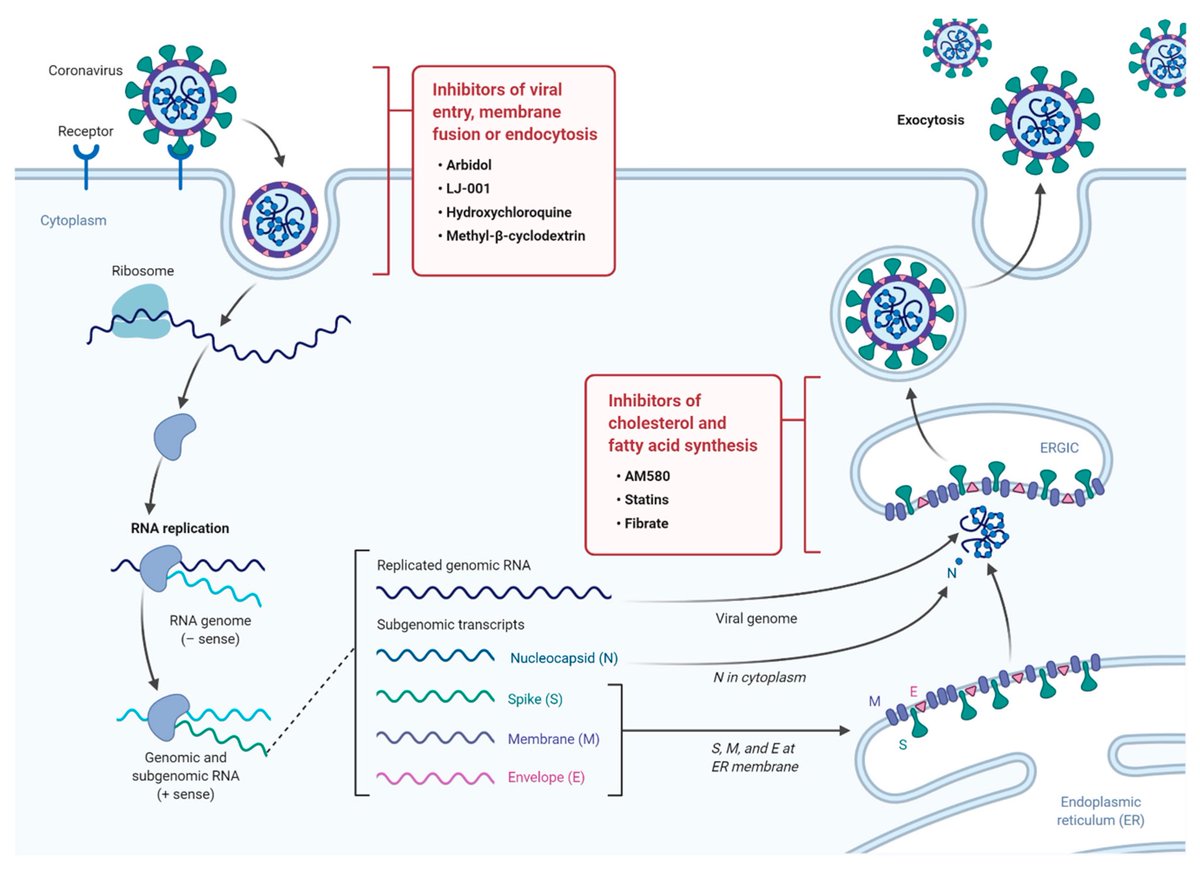
Research indicates that COVID-19 precipitates notable shifts in the host's lipid metabolism, leading to the accumulation of cellular lipid reserves. These alterations aid in the viral takeover of host cellular mechanisms, thus facilitating the progression of the infection. 6/ 
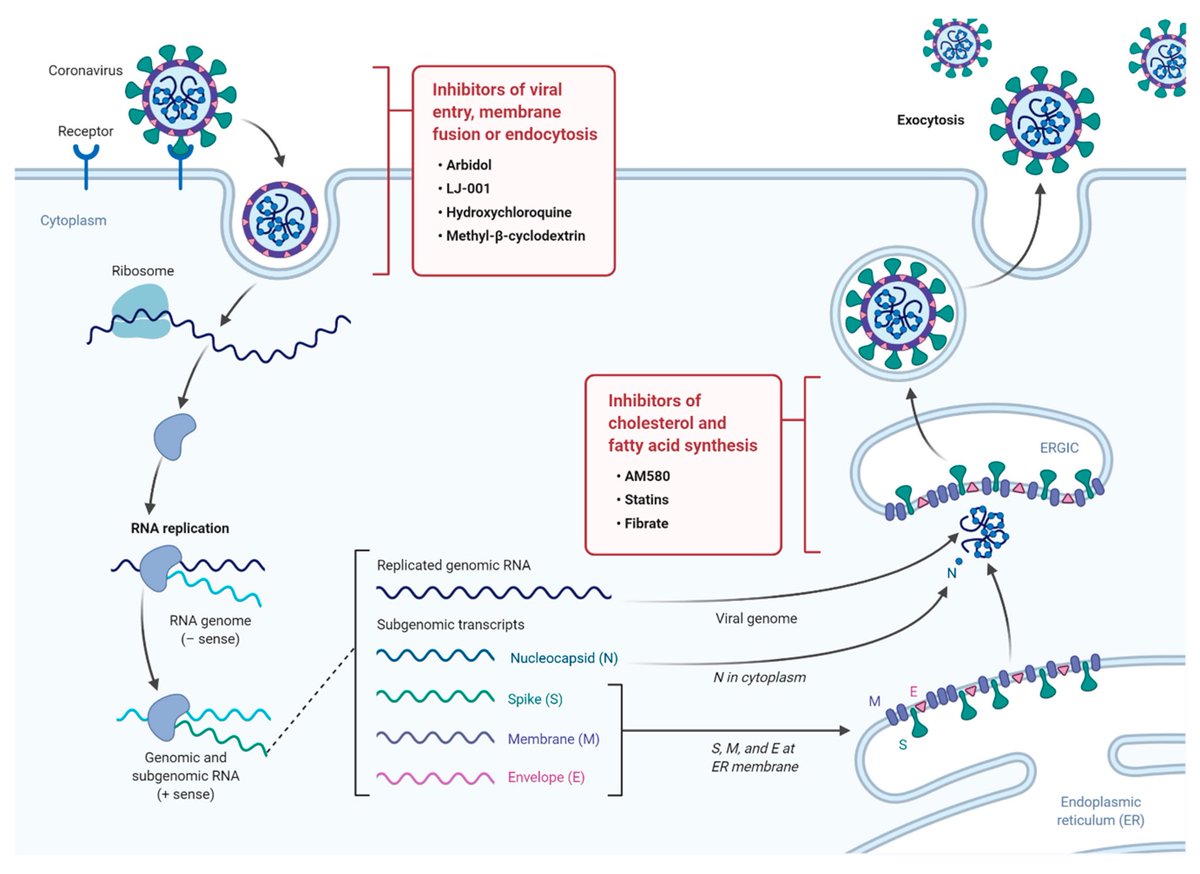
This theory gains support from laboratory evidence showing the cessation of viral replication upon the administration of small molecule lipid inhibitors, highlighting the critical dependence of the virus on host lipid resources for replication. 7/
A notable aspect of the interplay between HDL-C functionality and iron homeostasis is the process of ferroptosis, induced by lipid peroxidation and disturbed iron balance, characterized by the buildup of iron and products of lipid oxidation. 8/ 

This leads to diminished antioxidant defense capabilities. HDL-C is influential in mitigating the detrimental effects associated with ferroptosis, underscoring the significance of maintaining balanced iron levels in COVID-19 management. 9/
These findings highlight the exacerbating effect of impaired iron regulation on COVID-19 progression, further complicated by the disrupted protective functions of HDL-C. 10/
The outcome of the "war," between the host's metabolic defenses and viral invasion strategies, axes on the control over iron and lipid resources. The SARS-CoV-2 virus strategically targets these metabolic reserves to support its replication and spread. 11/
This battle underscores the complex interaction between host metabolic pathways and viral mechanisms, emphasizing the strategic importance of iron and lipid regulation in determining the course and outcome of COVID-19 infection. 12/ 
How does the strategic alteration of iron and HDL-C levels by a virus contribute to its underlying aim of targeting mitochondria to disrupt host defense mechanisms? 13/
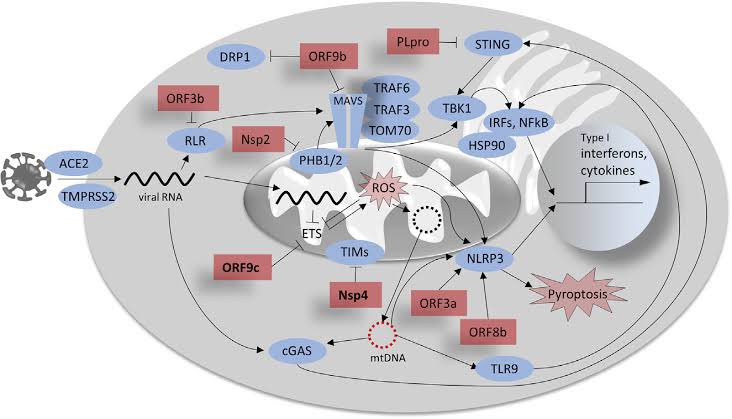
In the intricate dance of viral infection, the virus employs a calculated strategy aimed directly at the heart of the host's cellular energy and defense systems—the mitochondria. 14/ 
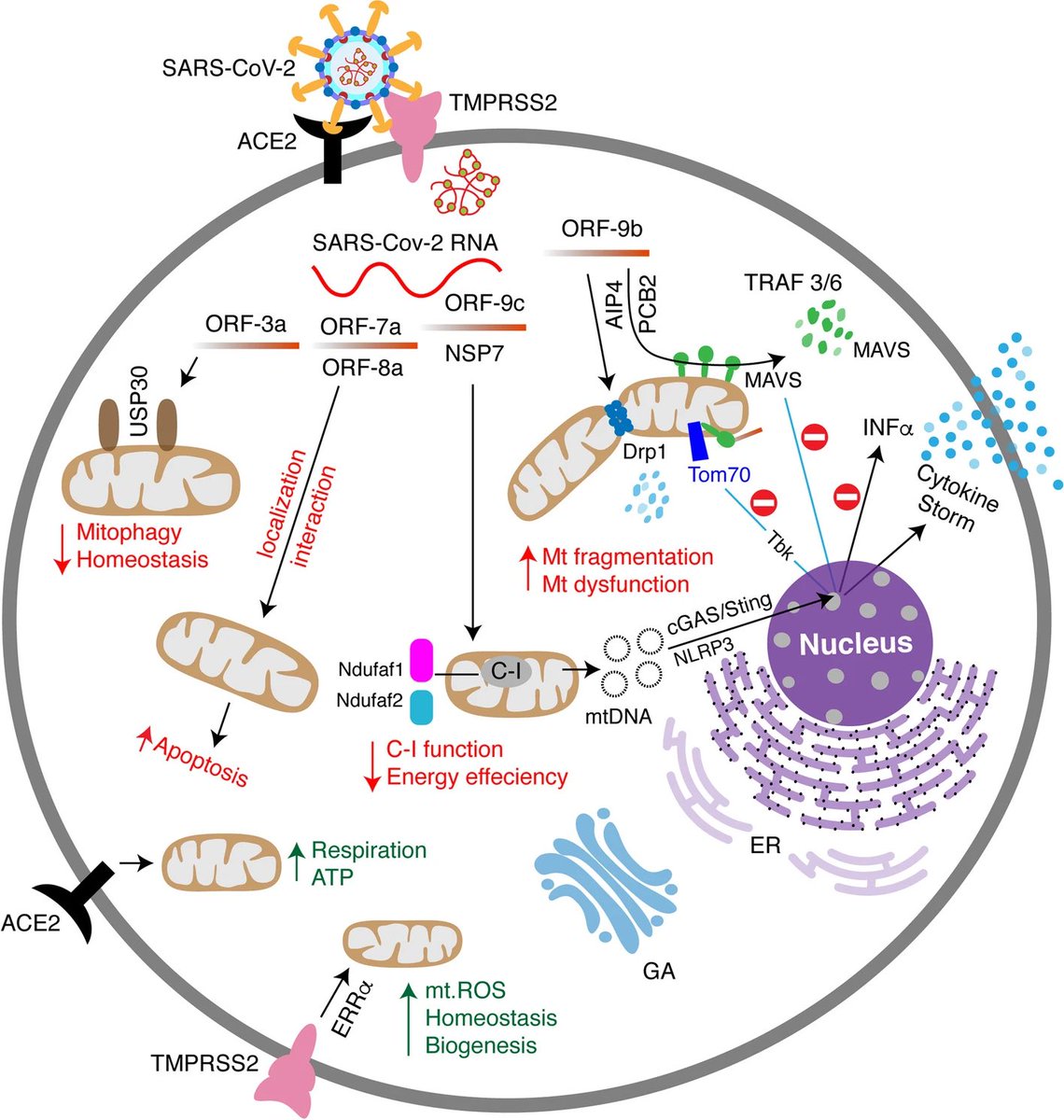
By subtly manipulating and altering the host's iron metabolism and HDL-C levels, the virus orchestrates a multifaceted attack designed to undermine mitochondrial integrity and function. 15/
This strategic disruption serves to weaken the mitochondria, a crucial step in the virus's broader aim to compromise the host's ability to mount an effective defense. Through this sophisticated mechanism of action, SARS2 ensures its survival & proliferation within the host 16/ 
The implications of this study are broad, providing a new understanding of long COVID-19's impact on metabolic health and laying the foundation for future research and therapeutic interventions aimed at improving patient outcomes. 17/
By considering these metabolic markers, we can shape preventive strategies and significantly mitigate the long-term impacts of COVID-19 on patients' health. 18/18
sciencedirect.com/science/articl…
sciencedirect.com/science/articl…
• • •
Missing some Tweet in this thread? You can try to
force a refresh