𝗙𝗿𝗼𝗺 𝗯𝗶𝗿𝗱𝘀 𝘁𝗼 𝗺𝗮𝗺𝗺𝗮𝗹𝘀: 𝘀𝗽𝗶𝗹𝗹𝗼𝘃𝗲𝗿 𝗼𝗳 𝗵𝗶𝗴𝗵𝗹𝘆 𝗽𝗮𝘁𝗵𝗼𝗴𝗲𝗻𝗶𝗰 𝗮𝘃𝗶𝗮𝗻 𝗶𝗻𝗳𝗹𝘂𝗲𝗻𝘇𝗮 𝗛5𝗡1,
led to efficient intra- and interspecies transmission
H/t @DuckSwabber
biorxiv.org/content/10.110…

led to efficient intra- and interspecies transmission
H/t @DuckSwabber
biorxiv.org/content/10.110…

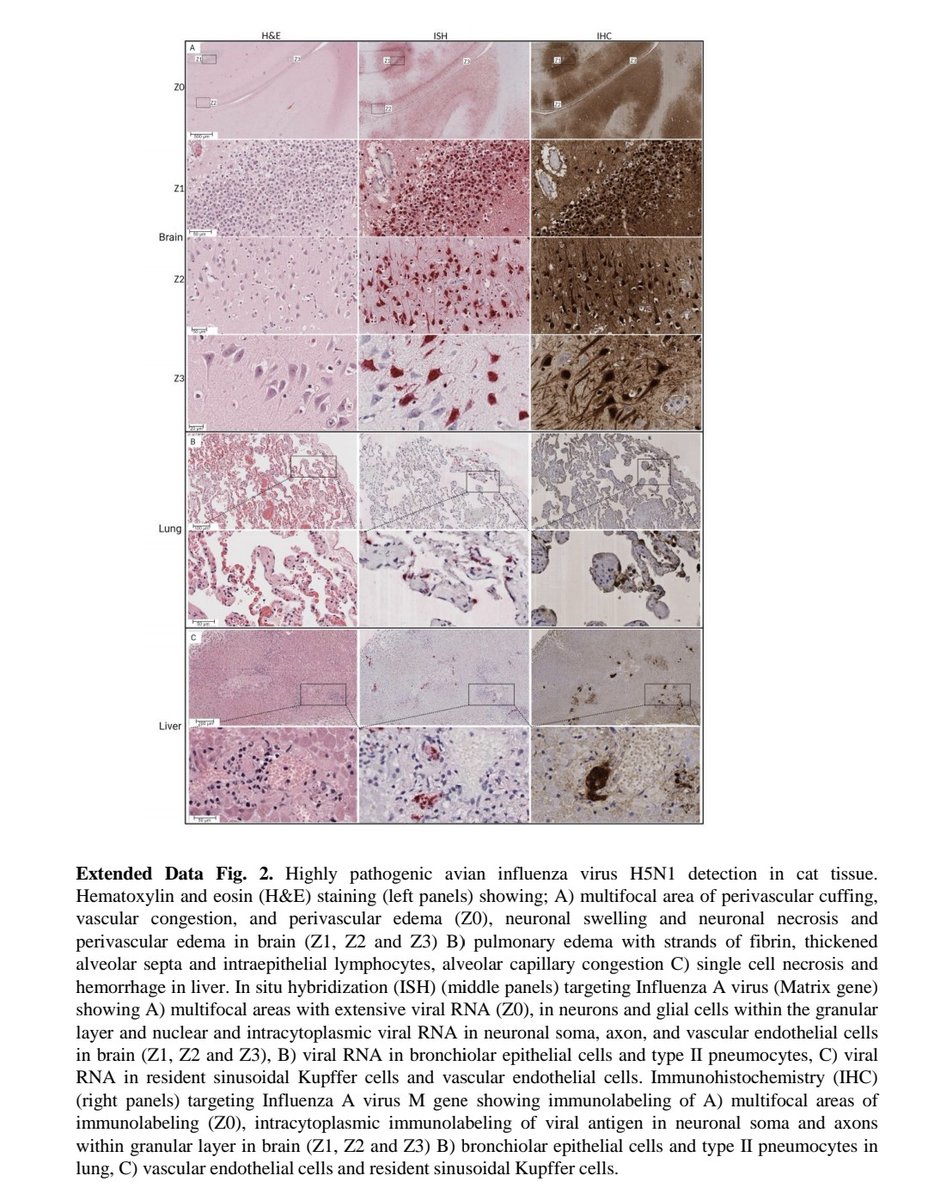
2) Highly pathogenic avian influenza H5N1 virus was detected infecting dairy cattle herds in several states in the U.S. in early 2024, representing the first report of H5N1 in a livestock species. 

3) Affected cattle displayed clinical signs like decreased appetite, respiratory distress, diarrhea, decreased milk production, and abnormal milk. Virus was detected in milk, nasal swabs, blood, and tissues of infected cows. 

4) Extensive virus replication was observed in the mammary glands of infected cows, resulting in high viral loads and shedding in milk. Histological analysis and virus staining showed tropism for milk-secreting epithelial cells. 

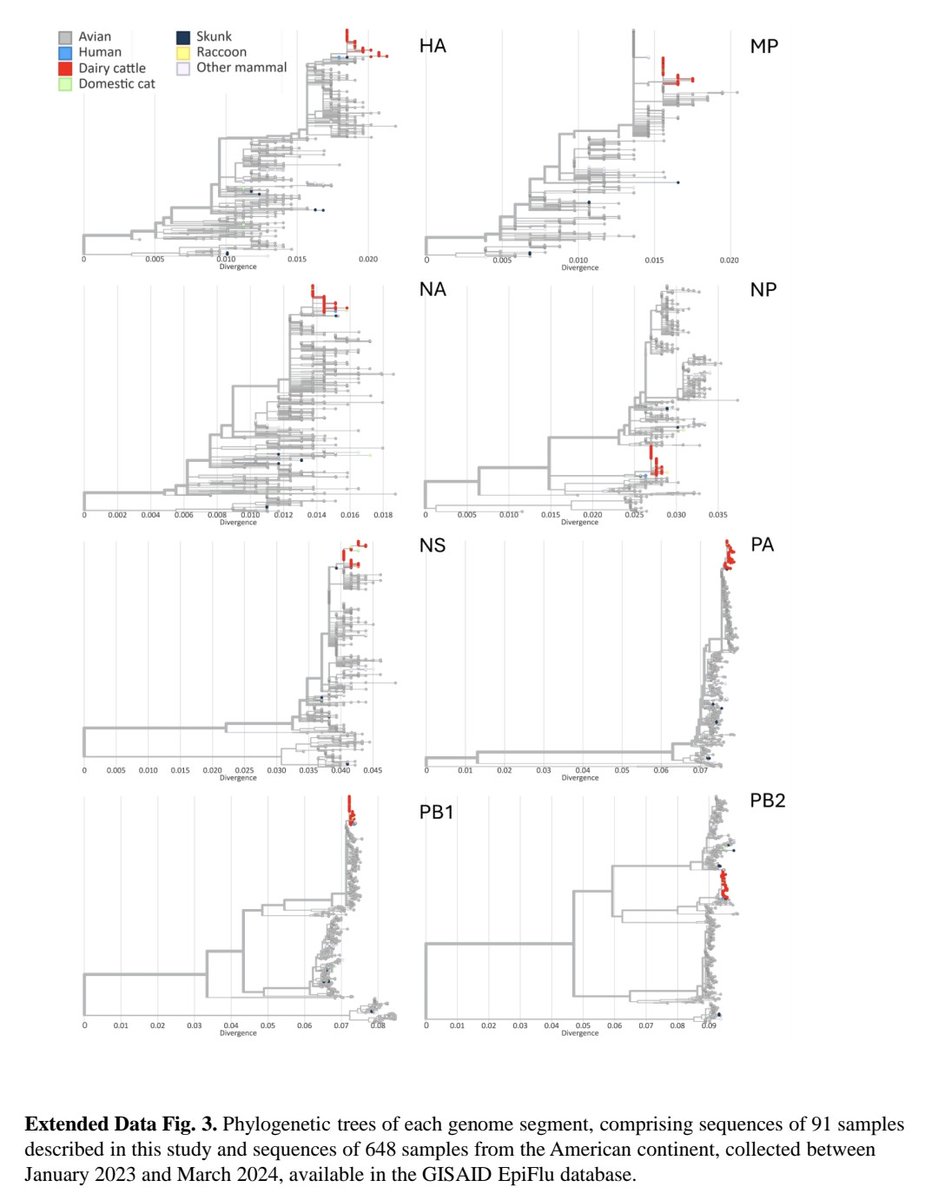
5) Virus transmission between cows was determined to be efficient based on epidemiological and genomic analysis. Virus was also transmitted to wild birds, domestic cats, and a raccoon on infected farms. 

6) Genomic analysis identified a reassortment event that produced a new genotype (B3.13) with enhanced ability to infect cows. Mutations accumulated after transmission to cows. 

7) Between-farm transmission occurred through livestock movement, contact with infected wild birds, and fomites/personnel movement between locations. 

8) This represents the first sustained transmission of H5N1 in a livestock species. Efficient shedding and transmission in cows is a concern that could allow the virus to further adapt to mammals. 
9) So in summary, this paper describes the spillover and transmission of H5N1 virus in dairy cattle herds in multiple U.S. states, highlighting its ability to cross species barriers into a new host.
Thanks for reading 🙏
Thanks for reading 🙏
• • •
Missing some Tweet in this thread? You can try to
force a refresh