What determines whether someone gets infected or not after exposure to SARS-CoV-2? A new study by Lindeboom et al examined this question with COVID-19 human challenge study. @BenIsraelow and I summarize their key findings in this News & Views 🧵 (1/)
nature.com/articles/d4158…
nature.com/articles/d4158…
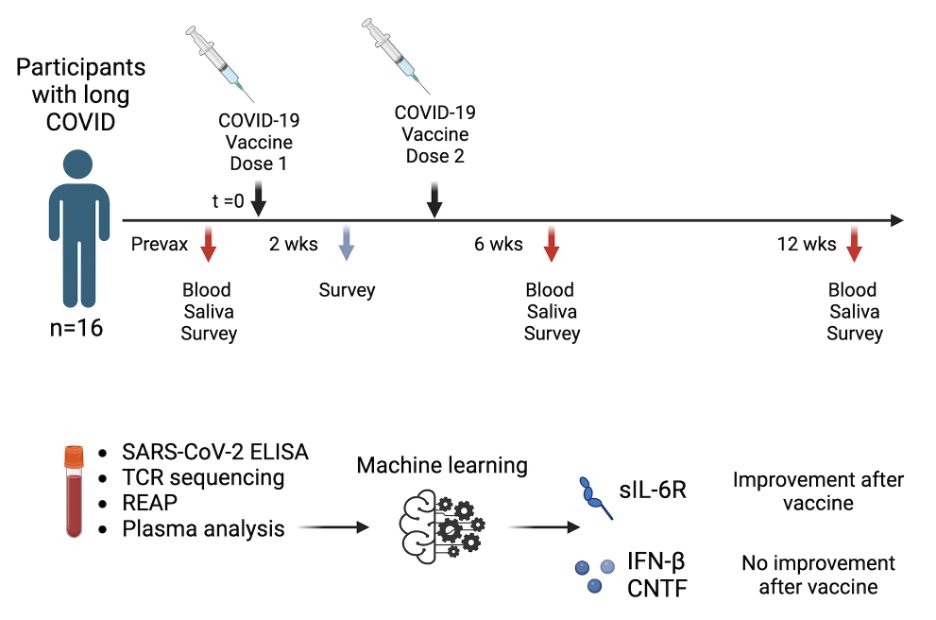
The study: 16 healthy young volunteers with no prior infection or vaccination were inoculated nasally with a low dose of pre-Alpha SARS-CoV-2 strain. Interestingly, only 6 had sustained infection, 3 had transient, and 7 had abortive infection at this dose. (2/) nature.com/articles/s4158…

The three infection outcomes allowed investigation of key features associated with susceptibility vs. resistance. Higher baseline expression of HLA-QA2 mRNA was associated with COVID resistance. Early nasal interferon I response was seen in those with transient infection. (3/) 

In people who had sustained infection, local IFN I responses and cellular infiltrations were delayed (>5 days). Transiently infected people had rapid IFN-I and cellular recruitment into the nasopharynx (1 day). Adaptive immunity was induced only after sustained infection. (4/) 

Curiously, in all exposed individuals regardless of infection outcomes, blood levels of activated monocytes declined while activated mucosal-associated invariant T (MAIT) cells were elevated ~3-10 days post-exposure. This feature may be useful as an early biomarker of viral exposure. (5/)

Of note, the HLA-DQA2 molecule may not operate conventionally as other MHC class II molecules. HLA-DQA2 is poorly polymorphic and highly conserved. It can pair with HLA-DQB2 to be expressed on Langerhans cells (antigen-presenting cells in the skin). (6/) doi.org/10.4049/jimmun…
Does HLA-DQA2 protein stimulate (unconventional?) T cells to provide COVID resistance? HLA-DQA2 mRNA might correlate with some other process that confers resistance. HLA-DQA2 alleles have been associated with diseases such as type 1 diabetes, rheumatoid arthritis, and Parkinson’s disease. (7/)
Fortunately, none of the challenged volunteers developed long COVID. This study provides key new insights into the immune signatures associated with sustained, transient, and abortive infection in human mucosa and blood. Congratulations to all the authors of this paper 👇🏼 (end) 

I will post the article on SharedIt so you can read our News and Views, as soon as I receive the link from Nature.
• • •
Missing some Tweet in this thread? You can try to
force a refresh