GUESS WHAT?! A new study has shown SARS-CoV-2 infection is DISTINCT from common respiratory viruses!
Unequivocally, COVID is NOT "just a cold."
These findings are HUGELY significant, for multiple reasons! Here's a breakdown of the study (written for a general audience)...
1/16
Unequivocally, COVID is NOT "just a cold."
These findings are HUGELY significant, for multiple reasons! Here's a breakdown of the study (written for a general audience)...
1/16
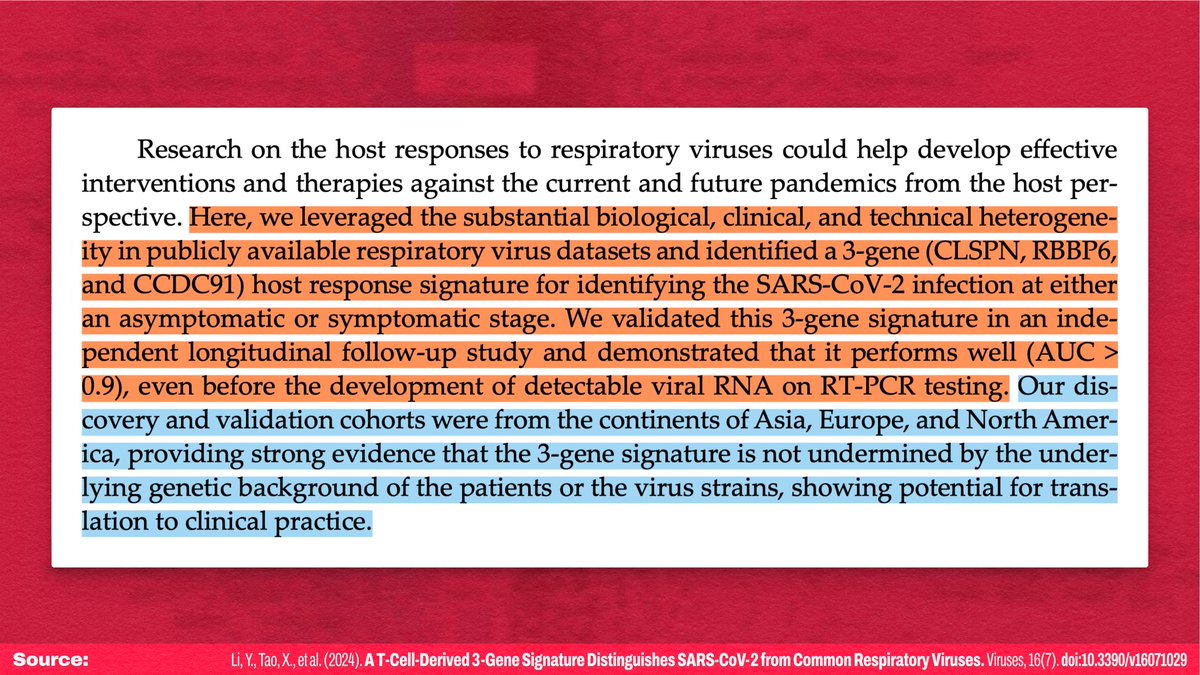
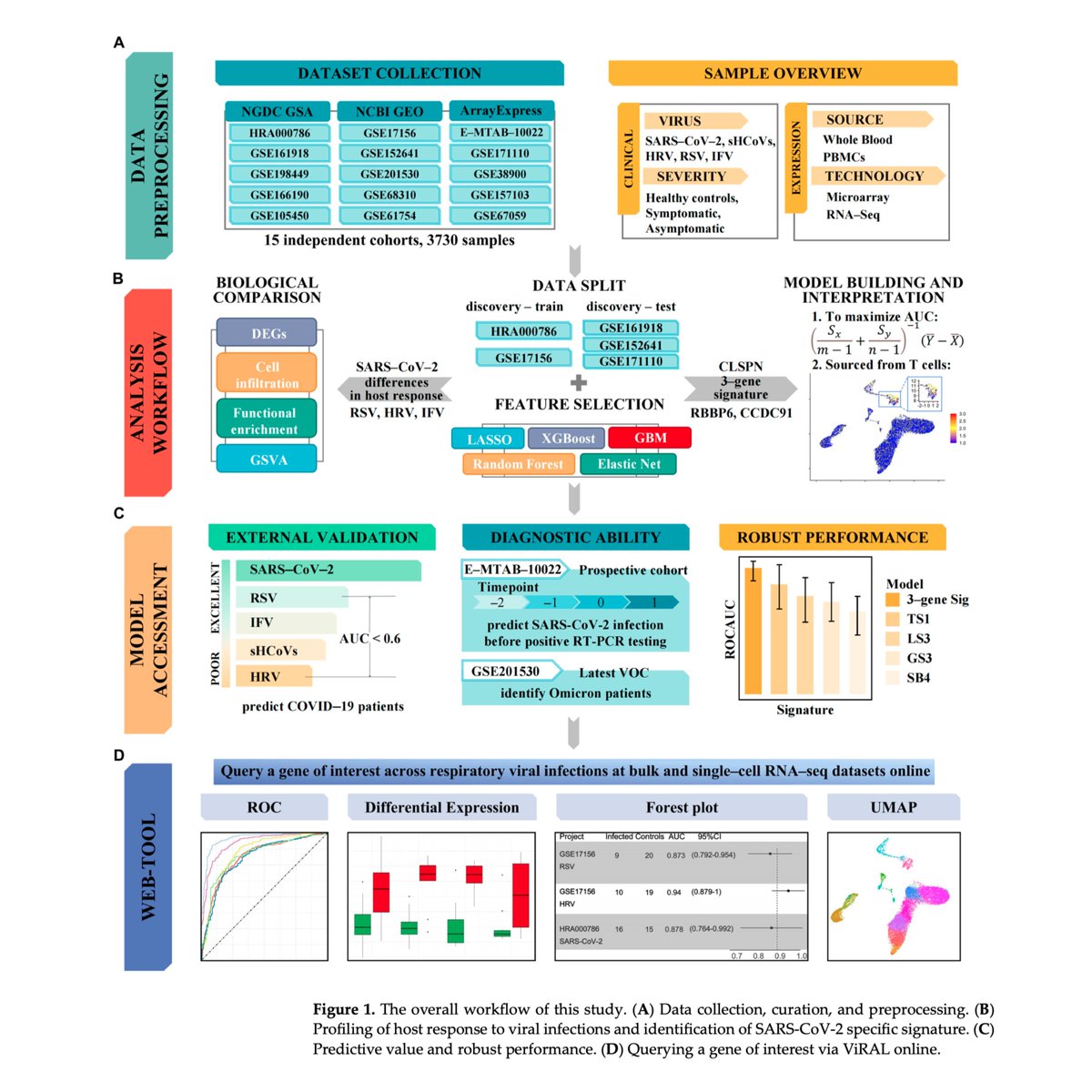
The paper is fairly complicated, so I'm going to start with the high-level takeaways before explaining everything in more detail.
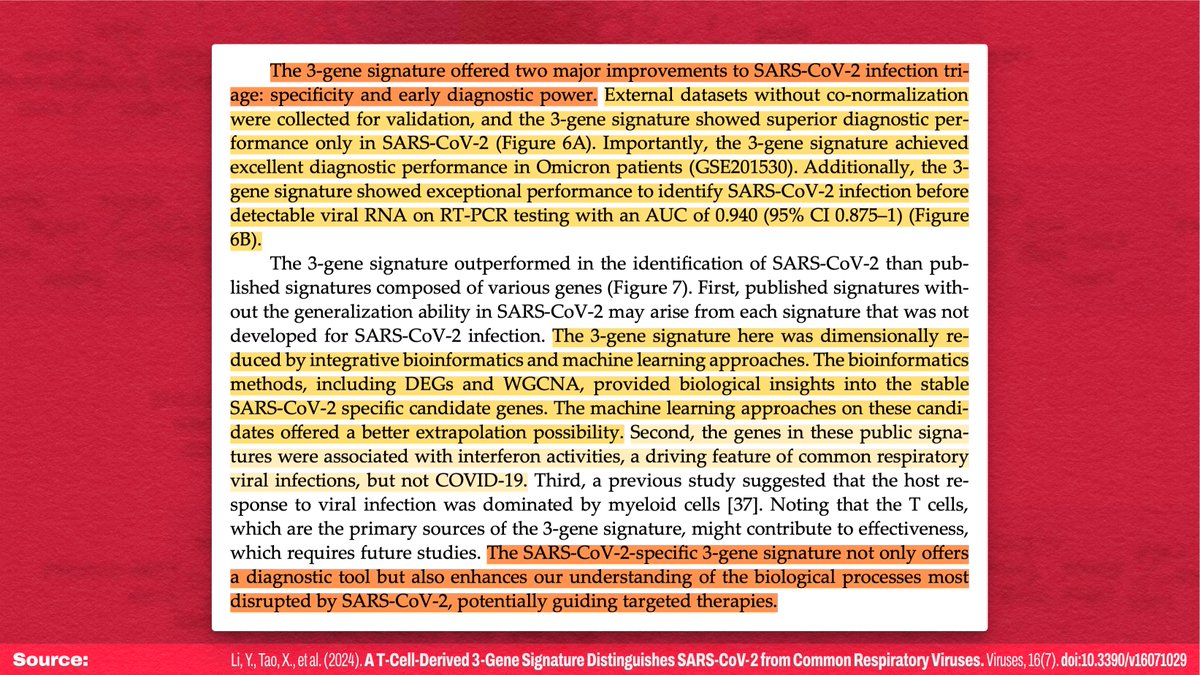
Overall, they found a 3-gene signature that distinguishes SARS-CoV-2 infections from common viral infections—long before PCR test positivity!
2/
Overall, they found a 3-gene signature that distinguishes SARS-CoV-2 infections from common viral infections—long before PCR test positivity!
2/
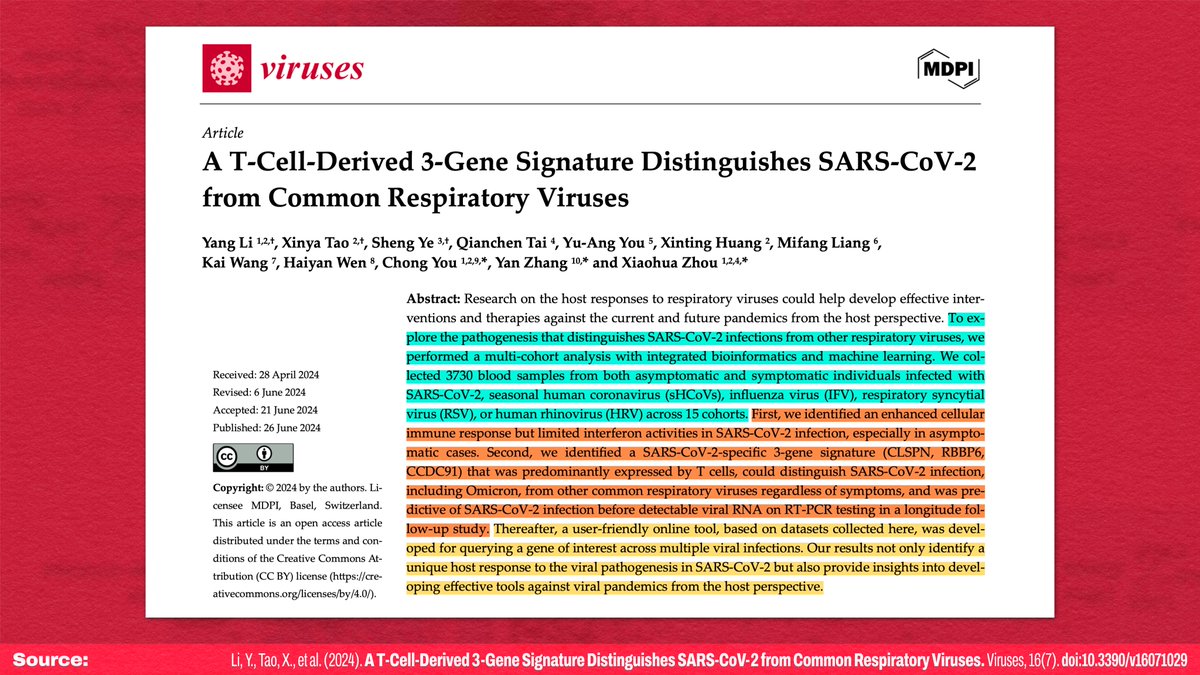
Because the signature:
1. is SPECIFIC to SARS-CoV-2,
2. is an EARLY indicator of infection,
3. is a DISTINCT pattern from other infections, and
4. even accurately identifies Omicron infections,
this discovery may be useful as a diagnostic tool AND a direction for treatment!
3/
1. is SPECIFIC to SARS-CoV-2,
2. is an EARLY indicator of infection,
3. is a DISTINCT pattern from other infections, and
4. even accurately identifies Omicron infections,
this discovery may be useful as a diagnostic tool AND a direction for treatment!
3/
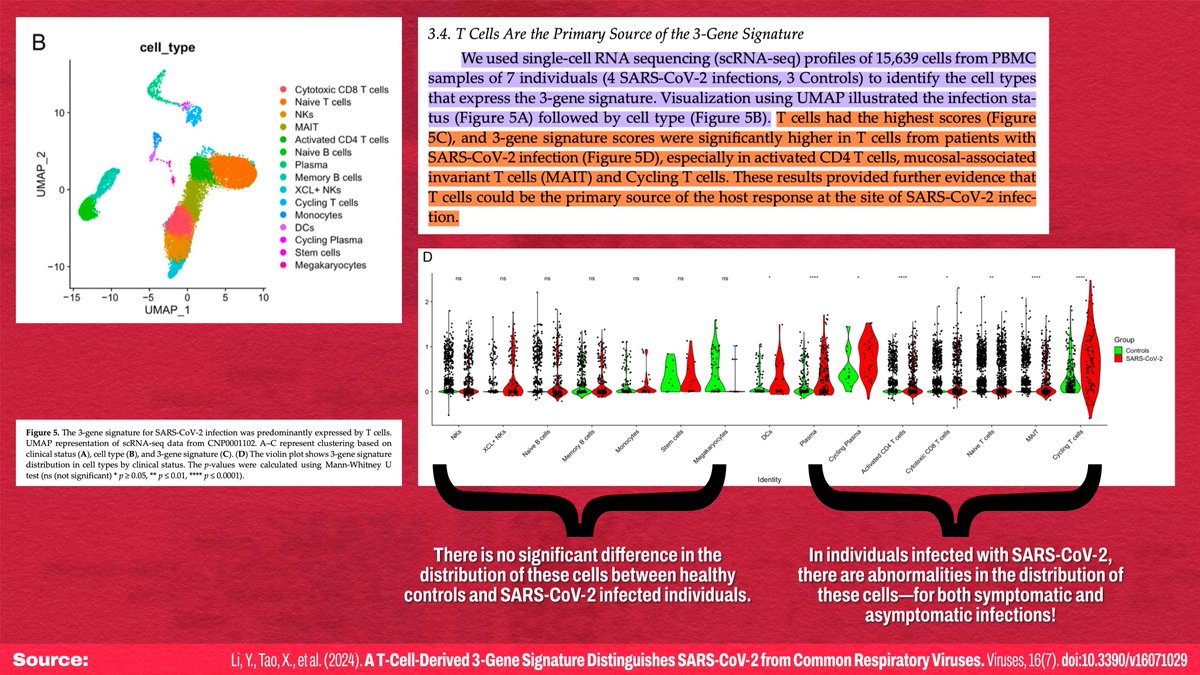
One of the major limitations of this study is that it's unknown how applicable this signature will be for immunocompromised individuals. Why?
Because T cells were the major source of this 3-gene signature being expressed! This is important, because...
4/
Because T cells were the major source of this 3-gene signature being expressed! This is important, because...
4/
This is YET ANOTHER study showing SARS-CoV-2 adversely impacts the immune system.
Monocyte abnormalities (decreases) were found in BOTH symptomatic and asymptomatic SARS-CoV-2 infections! Because monocytes INCREASE in normal immune response, this suggests monocyte infection!
5/!["In addition, the results of CIBERSORTx revealed a reduced level of monocytes in SARS-CoV2 infection, while other viruses introduced an elevated level of monocytes, especially in the symptomatic group (Figure 3A). SARS-CoV-2-related monocytic abnormalities have been observed in both symptomatic [53] and asymptomatic cases [17]. The possible mechanism might be that the monocytes could be directly infected with SARS-CoV-2, leading to pyroptosis [54]. Moreover, attention should be paid to the boosted levels of IFNG and TNF in COVID-19 (Figure 3B), as synergism of TNF-α and IFNG triggers i...](/images/1px.png)
Monocyte abnormalities (decreases) were found in BOTH symptomatic and asymptomatic SARS-CoV-2 infections! Because monocytes INCREASE in normal immune response, this suggests monocyte infection!
5/
!["In addition, the results of CIBERSORTx revealed a reduced level of monocytes in SARS-CoV2 infection, while other viruses introduced an elevated level of monocytes, especially in the symptomatic group (Figure 3A). SARS-CoV-2-related monocytic abnormalities have been observed in both symptomatic [53] and asymptomatic cases [17]. The possible mechanism might be that the monocytes could be directly infected with SARS-CoV-2, leading to pyroptosis [54]. Moreover, attention should be paid to the boosted levels of IFNG and TNF in COVID-19 (Figure 3B), as synergism of TNF-α and IFNG triggers i...](https://pbs.twimg.com/media/GR2Q-rNWwAArG5p.jpg)
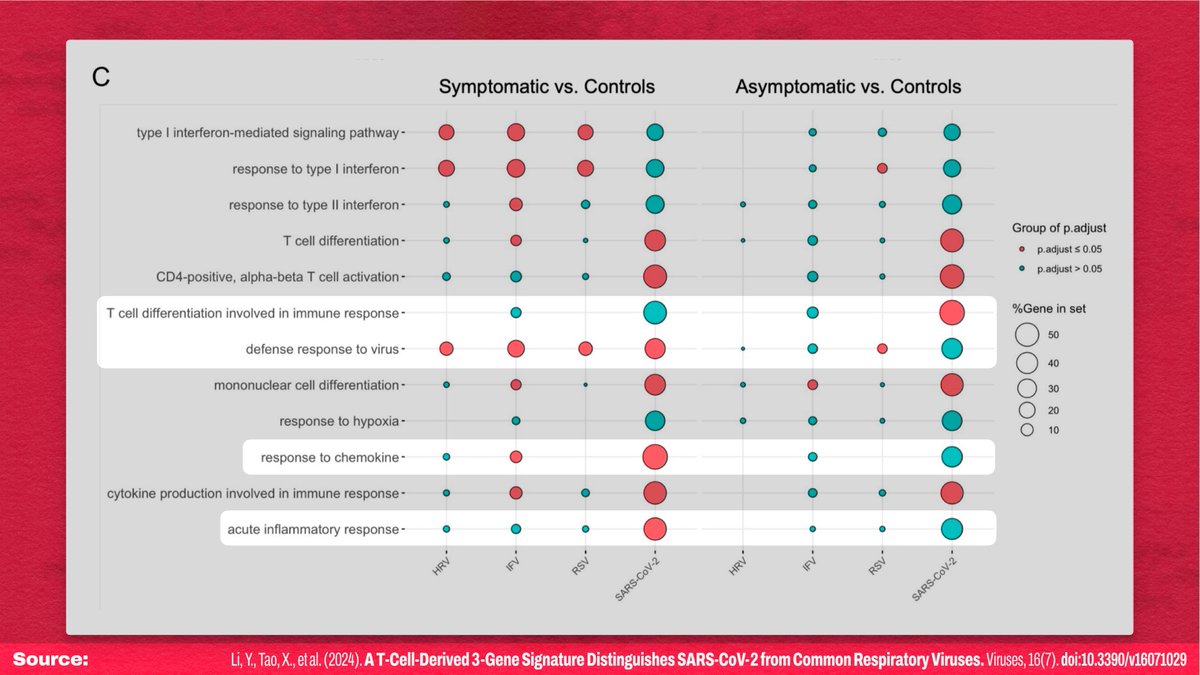
This study also found the same odd immune response patterns found by other studies: The immune system is STRONGLY activated (especially the inflammatory response), but the pathway responsible for signaling *targeted* attacks on infected cells is suppressed!
6/!["Host responses resulting in SARS-CoV-2 infection differed from several common respiratory viruses. These results were in line with previous in vitro studies [9] (Figure S5). Although part of ISGs (i.e., IFI27) were enhanced in SARS-CoV-2 infection (Figure 2A), moderate IFN responses have been a sign of COVID-19 (Figure 2C). The improved cellular immune response, such as strong T cell responses and high secretion of TNF, were observed, surprisingly in these asymptomatic subjects (Figures 2 and 3). It has been reported that asymptomatic SARS-CoV-2-infected individuals might develop an effi...](/images/1px.png)
6/
!["Host responses resulting in SARS-CoV-2 infection differed from several common respiratory viruses. These results were in line with previous in vitro studies [9] (Figure S5). Although part of ISGs (i.e., IFI27) were enhanced in SARS-CoV-2 infection (Figure 2A), moderate IFN responses have been a sign of COVID-19 (Figure 2C). The improved cellular immune response, such as strong T cell responses and high secretion of TNF, were observed, surprisingly in these asymptomatic subjects (Figures 2 and 3). It has been reported that asymptomatic SARS-CoV-2-infected individuals might develop an effi...](https://pbs.twimg.com/media/GR2RB6-acAIcs_W.jpg)
As shown in Figure 2C, BOTH symptomatic and asymptomatic SARS-CoV-2 activate identical cellular pathways, but with less inflammatory signaling for asymptomatic infections.
That is, even asymptomatic SARS-CoV-2 impacts processes usually unaffected by the other studied viruses!
7/
That is, even asymptomatic SARS-CoV-2 impacts processes usually unaffected by the other studied viruses!
7/
This study strongly suggests that there are "distinct molecular mechanisms" at play during SARS-CoV-2 infections, relative to other common respiratory viruses.
It *unambiguously* shows, however, that even asymptomatic SARS-CoV-2 infections are NOT "just a cold."
8/!["Discovery and validation of SARS-CoV-2-specific host response genes have been calling [26]. To address this issue, an ideal dataset for biomarker discovery should include not only SARS-CoV-2 infections but also other respiratory infections (Figure 4). Therefore, we co-normalized datasets HRA000786 and GSE17156, which included both asymptomatic and symptomatic cases. With integrative bioinformatics and machine learning approaches, we identified that the combination of CLSPN, RBBP6, and CCDC91 was robustly associated with SARS-CoV-2 infection in both discovery and validation datasets. Col...](/images/1px.png)
It *unambiguously* shows, however, that even asymptomatic SARS-CoV-2 infections are NOT "just a cold."
8/
!["Discovery and validation of SARS-CoV-2-specific host response genes have been calling [26]. To address this issue, an ideal dataset for biomarker discovery should include not only SARS-CoV-2 infections but also other respiratory infections (Figure 4). Therefore, we co-normalized datasets HRA000786 and GSE17156, which included both asymptomatic and symptomatic cases. With integrative bioinformatics and machine learning approaches, we identified that the combination of CLSPN, RBBP6, and CCDC91 was robustly associated with SARS-CoV-2 infection in both discovery and validation datasets. Col...](https://pbs.twimg.com/media/GR2RJ5uWAAAB6p_.jpg)
The authors validated their discovery with a longitudinal study that was able to detect even asymptomatic Omicron infections with high accuracy, long before a given patient is able to test positive with RT-PCR testing.
9/
9/
That's all the highlights! The study is Open Access and available at
The rest of this thread is going to be commentary/analysis of the details of the study...
10/16mdpi.com/1999-4915/16/7…
The rest of this thread is going to be commentary/analysis of the details of the study...
10/16mdpi.com/1999-4915/16/7…
So what role do these genes play?
It seems to be a cascade that highjacks the innate and adaptive immune responses in a way that's advantageous for the SARS-CoV-2 virus itself. That's not to say that the virus *directly* increases expression of these genes...
11/!["We proposed that the upregulation of CLSPN, RBBP6, and CCDC91 by SARS-CoV-2 in T cells might create a cascade of effects that alter both the innate and adaptive immune responses. First, CLSPN plays a significant role in genomic stability during DNA replication [56]. ... CLSPN might help T cells manage the stress and damage induced by viral replication. Second, ... RBBP6 is involved in cell cycle regulation, apoptosis, and ubiquitination processes [58]. RBBP6 has been reported as a negative regulator of Ebola virus replication by mimicking the viral protein [59]. ... RBBP6 might preven...](/images/1px.png)
It seems to be a cascade that highjacks the innate and adaptive immune responses in a way that's advantageous for the SARS-CoV-2 virus itself. That's not to say that the virus *directly* increases expression of these genes...
11/
!["We proposed that the upregulation of CLSPN, RBBP6, and CCDC91 by SARS-CoV-2 in T cells might create a cascade of effects that alter both the innate and adaptive immune responses. First, CLSPN plays a significant role in genomic stability during DNA replication [56]. ... CLSPN might help T cells manage the stress and damage induced by viral replication. Second, ... RBBP6 is involved in cell cycle regulation, apoptosis, and ubiquitination processes [58]. RBBP6 has been reported as a negative regulator of Ebola virus replication by mimicking the viral protein [59]. ... RBBP6 might preven...](https://pbs.twimg.com/media/GR2RRiZXQAATToF.jpg)
Rather, these are the common product of the cascade of dysfunctional processes triggered by SARS-CoV-2 infection. This study identified a unique signature of *differentially expressed genes*, but there's not a 1:1 cause and effect for differential expression of a given gene!
12/!["Although there is limited specific information on the expression changes of CCDC91 in response to viral infections, CCDC50, a related gene to CCDC91, negatively regulated the type I IFN signaling pathway initiated by RIG-I-like receptors (RLRs), the sensors for RNA viruses [60]. Together, these genes may in concert with T cells not only respond to viral infections effectively through cellular immunity but also regulate the immune response to avoid excessive inflammation or autoimmunity. Further experimental validation and research would be essential to elucidate these proposed mechanisms...](/images/1px.png)
12/
!["Although there is limited specific information on the expression changes of CCDC91 in response to viral infections, CCDC50, a related gene to CCDC91, negatively regulated the type I IFN signaling pathway initiated by RIG-I-like receptors (RLRs), the sensors for RNA viruses [60]. Together, these genes may in concert with T cells not only respond to viral infections effectively through cellular immunity but also regulate the immune response to avoid excessive inflammation or autoimmunity. Further experimental validation and research would be essential to elucidate these proposed mechanisms...](https://pbs.twimg.com/media/GR2RU8fWkAAHF34.jpg)
The methods were thorough, in that they cross-validated all of their findings multiple ways to ensure they weren't picking up on some spurious signal in the data. Even if the genes turn out not to be meaningful for *pathogenesis*, they're VERY meaningful for *diagnosis*!
13/
13/
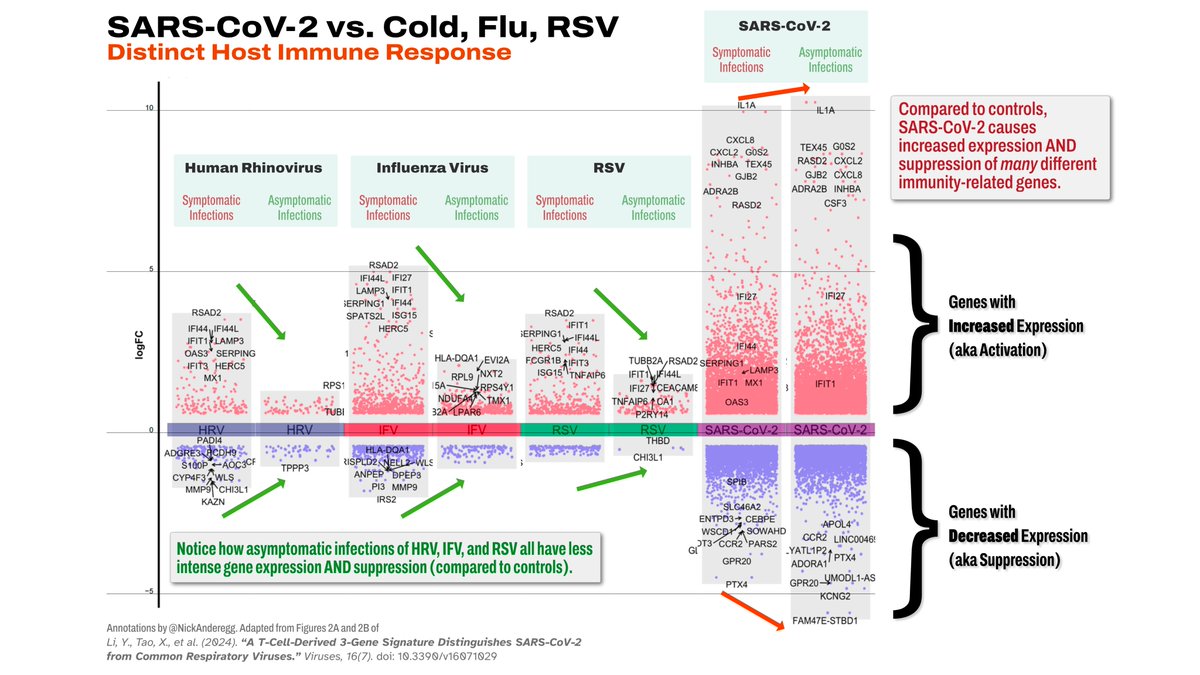
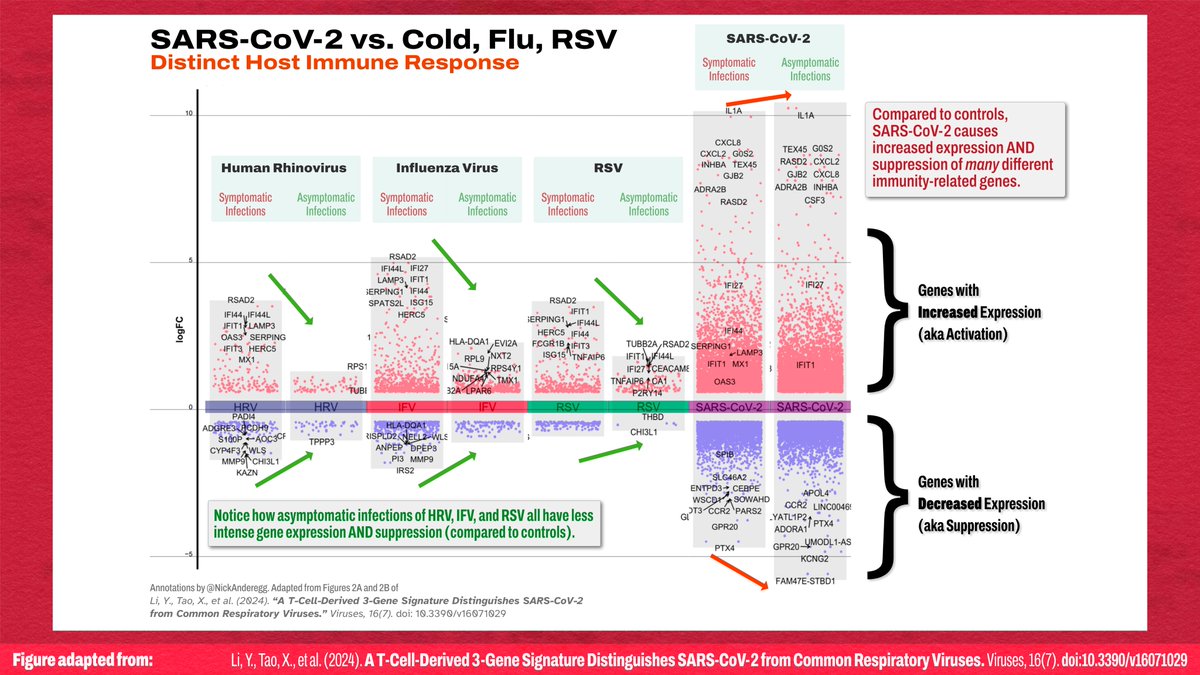
IMO, there's one big error. Figures 2A and 2B have slightly different Y-axes, likely because the graphs were generated separately, but it actually has the effect of shrinking a range that is *unexpectedly* larger.
I aligned the scales on Figures 2A and 2B here
14/
I aligned the scales on Figures 2A and 2B here
14/
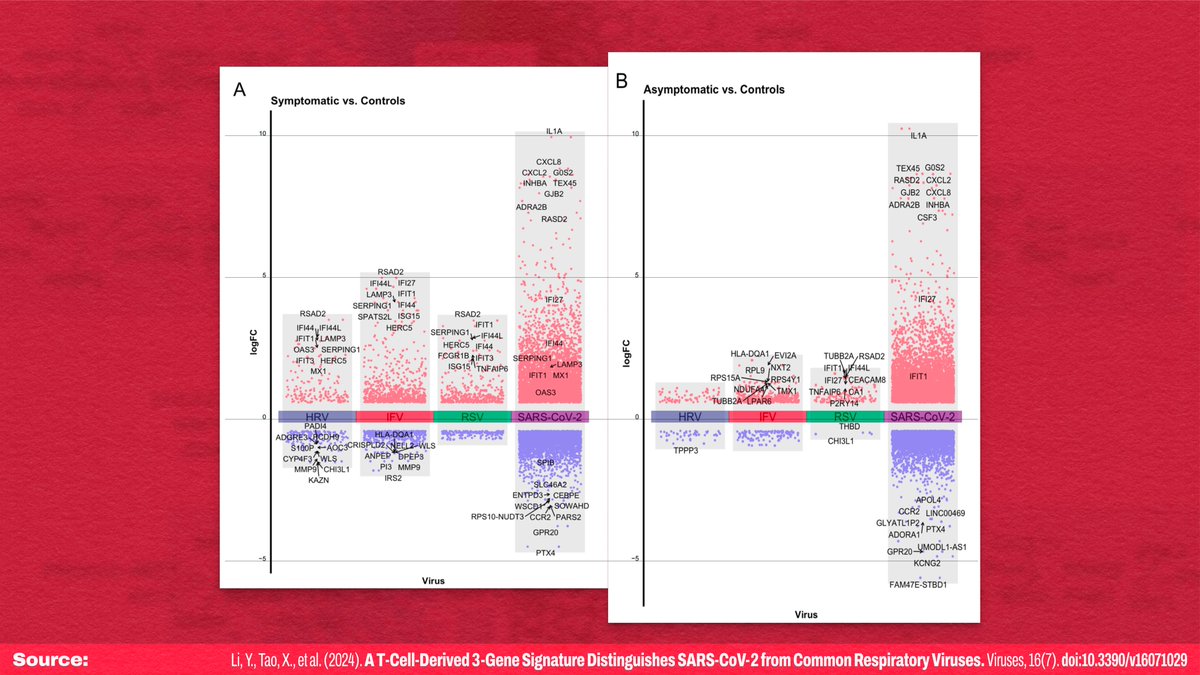
When symptomatic and asymptomatic gene expression for each virus are put side by side, it's clear that SARS-CoV-2 has a wildly different pattern compared to the other viruses, and a vastly larger magnitude of effect.
Differential expression INCREASES in asymptomatic covid?!
15/
Differential expression INCREASES in asymptomatic covid?!
15/
Most notably, T cells are the PRIMARY type of cell where the 3-gene signature is most differentially expressed... and it's specifically a pattern that will lead to T cell exhaustion through overactivation.
Say it with me: "COVID is airborne and exhausts T cells!"
16/end
Say it with me: "COVID is airborne and exhausts T cells!"
16/end
Afterthought: The bit about “discovery should include not only SARS-CoV-2 infections but also other respiratory infections” is an echo of another paper about HCoV-OC43… from 1980! There, the author also complained about lack of dataset diversity
17/16
![Discovery and validation of SARS-Co V-2-specific host response genes have been calling 26]. To address this issue, an ideal dataset for biomarker discovery should include not only SARS-CoV-2 infections but also other respiratory infections (Figure 4). Therefore, we co-normalized datasets HRA000786 and GSE17156, which included both asymptomatic and symptomatic cases. With integrative bioinformatics and machine learning approaches, we identified that the combination of CLSPN, RBBP6, and CCDC91 was robustly associated with SARS-CoV-2 infection in both discovery and validation datasets. Collect...](/images/1px.png)
17/16
https://x.com/nickanderegg/status/1768298525345960333
![Discovery and validation of SARS-Co V-2-specific host response genes have been calling 26]. To address this issue, an ideal dataset for biomarker discovery should include not only SARS-CoV-2 infections but also other respiratory infections (Figure 4). Therefore, we co-normalized datasets HRA000786 and GSE17156, which included both asymptomatic and symptomatic cases. With integrative bioinformatics and machine learning approaches, we identified that the combination of CLSPN, RBBP6, and CCDC91 was robustly associated with SARS-CoV-2 infection in both discovery and validation datasets. Collect...](https://pbs.twimg.com/media/GR3DX4FboAACeWT.jpg)
I’m not sure if it would, because at least one of the genes is involved in one type of cell entry, and there’s evidence that persistent infections may use *different* methods to move between cells that possibly wouldn’t engage that gene!
18/16
18/16
https://twitter.com/denysbennett/status/1809872943234605533
2. Lots of things can cause lymphopenia! () It's just usually *temporary* with most non-HIV causes.
1. Like the HIV patients on death's door in the 90s, who are alive today thanks to HAART, recovery may be possible
19/16
en.wikipedia.org/wiki/Lymphocyt…
![The most common cause of temporary lymphocytopenia is a recent infection, such as the common cold.[citation needed] Lymphocytopenia, but not idiopathic CD4+ lymphocytopenia, is associated with corticosteroid use, infections with HIV and other viral, bacterial, and fungal agents, malnutrition, systemic lupus erythematosus,[3] severe stress,[4] intense or prolonged physical exercise (due to cortisol release),[5] rheumatoid arthritis, sarcoidosis,[6] multiple sclerosis,[7] and iatrogenic (caused by other medical treatments) conditions. Lymphocytopenia is a frequent, temporary result from man...](/images/1px.png)
1. Like the HIV patients on death's door in the 90s, who are alive today thanks to HAART, recovery may be possible
19/16
en.wikipedia.org/wiki/Lymphocyt…
https://x.com/DoctorVive/status/1809962555953103125
![The most common cause of temporary lymphocytopenia is a recent infection, such as the common cold.[citation needed] Lymphocytopenia, but not idiopathic CD4+ lymphocytopenia, is associated with corticosteroid use, infections with HIV and other viral, bacterial, and fungal agents, malnutrition, systemic lupus erythematosus,[3] severe stress,[4] intense or prolonged physical exercise (due to cortisol release),[5] rheumatoid arthritis, sarcoidosis,[6] multiple sclerosis,[7] and iatrogenic (caused by other medical treatments) conditions. Lymphocytopenia is a frequent, temporary result from man...](https://pbs.twimg.com/media/GR5RzAuXMAAH7Kx.jpg)
Simply put, if the cause of dysregulation is removed, the immune system can *likely* recover.
Time is the enemy, in this case! Cancer is a huge concern here, because without immune cells, cells with defective DNA will be ignored and grow into tumors
20/16
Time is the enemy, in this case! Cancer is a huge concern here, because without immune cells, cells with defective DNA will be ignored and grow into tumors
20/16
https://x.com/nerfherding_sm/status/1809836851160641822
Opportunistic infections are the biggest concern with a compromised immune system (lack of defenses), but when an individual has effectively zero immune system, the body isn't able to perform basic janitorial tasks that clean up random defective processes!
21/16
21/16
Sure! Here's a meta-annotated version of the graph with simplified explanations of each element. The graph itself is fairly noisy, but the takeaways are simple!
tl;dr: larger graph = more intense response
[Quoted tweet was referring to the graph]
22/16

tl;dr: larger graph = more intense response
[Quoted tweet was referring to the graph]
22/16
https://x.com/HenryWilliams74/status/1809936864469762218
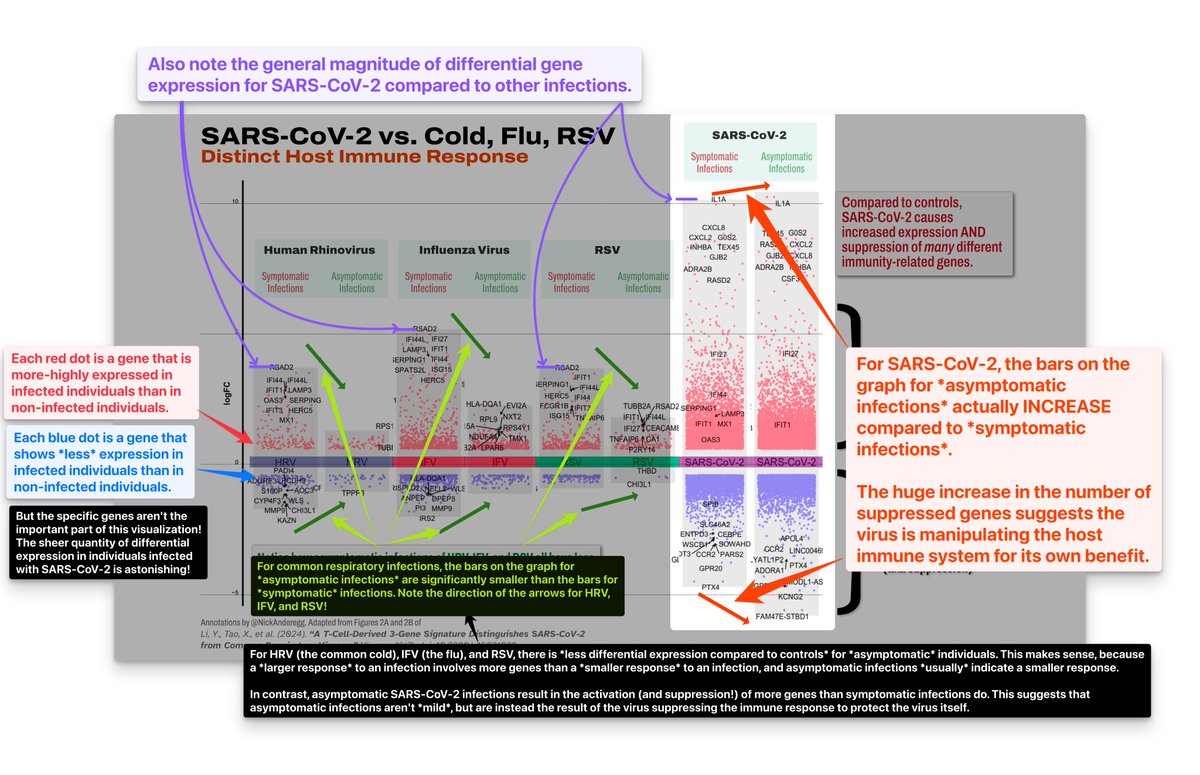
Lack of symptoms may not even be because of immune system *destruction*! Symptoms of cold and flu are driven by interferon signaling, which SARS-CoV-2 suppresses.
But the end result is the same: lack of effective immune response!
23/16
But the end result is the same: lack of effective immune response!
23/16
https://x.com/heretolearnyyc/status/1809986755757777341
The immune system has a vast range of functions spread across different systemic and cellular mechanisms.
It's likely that there are many people walking around with a compromised innate immune system, who don't realize it as leftover adaptive defenses fight infections
24/16
It's likely that there are many people walking around with a compromised innate immune system, who don't realize it as leftover adaptive defenses fight infections
24/16
This discovery seems to have a clear path to commercialization, because this discovery is purely a new method of *analyzing* the results of existing types of Nucleic Acid Amplification Tests (NAAT), including RT-PCR and LAMP testing. It's software!
25/16
25/16
https://x.com/VanyaWright/status/1809911385872064817
The advantage here is that, rather than requiring detection of a specific viral protein (which may be present in the body but not the swab location), it requires detection of elevated levels of HOST PROTEINS that indicate active viral infection!
26/16
26/16
Here's the entire thread about the article "A T-Cell-Derived 3-Gene Signature Distinguishes SARS-CoV-2 from Common Respiratory Viruses," on a single page for easier sharing:
readwise.io/reader/shared/…
readwise.io/reader/shared/…
[Caveat: This doesn’t apply to people trying supplements as *treatment*]
Supplements will have no effect. The deficiencies associated with severe covid/LC are likely a product of the infection itself, because the virus is dysregulating the production processes
27/16
Supplements will have no effect. The deficiencies associated with severe covid/LC are likely a product of the infection itself, because the virus is dysregulating the production processes
27/16
https://twitter.com/ayarayarohi/status/1810071935067488515
• • •
Missing some Tweet in this thread? You can try to
force a refresh


![“8. Performance of Nuclear Power Plants Affected by the Blackout On August 14, 2003, nine U.S. nuclear power plants experienced rapid shutdowns (reactor trips) as a consequence of the power outage. Seven nuclear power plants in Canada operating at high power levels at the time of the event also experienced rapid shutdowns. […]. Many non-nuclear generating plants in both countries also tripped during the event. Numerous other nuclear plants observed disturbances on the electrical grid but continued to generate electrical power without interruption. […] - The severity of the grid transient...](https://pbs.twimg.com/media/G0Q9wDEXkAAknYM.jpg)








