NEW PREPRINT! This one seems potentially very, VERY SIGNIFICANT!
This study found "significant reductions in measures of mitochondrial content and impaired muscle energetics" in LC fatigue—AND a corresponding biomarker!
Summary thread (for a general audience!)...
1/many
This study found "significant reductions in measures of mitochondrial content and impaired muscle energetics" in LC fatigue—AND a corresponding biomarker!
Summary thread (for a general audience!)...
1/many

So as you probably know (or at least, should know), prolonged fatigue is one of the most common and significant long-term consequences of COVID, even after mild cases.
Studies have pointed to the T cell response having an impact on mitochondrial function.
2/
Studies have pointed to the T cell response having an impact on mitochondrial function.
2/

They sought to examine if there are specific factors that stand out in relation to mitochondria. They found two major things:
- Mitochondrial function is impaired.
- The "T cell-derived soluble IL-2 receptor alpha subunit" (sIL2R) may play a role in this impairment.
3/
- Mitochondrial function is impaired.
- The "T cell-derived soluble IL-2 receptor alpha subunit" (sIL2R) may play a role in this impairment.
3/

So, what did they find specifically?
This study looked at those with "mild to moderate" COVID, meaning they had at least one symptom but didn't require oxygen or hospitalization. For some of the experiments, they also included pre-pandemic biopsies as controls!
4/
This study looked at those with "mild to moderate" COVID, meaning they had at least one symptom but didn't require oxygen or hospitalization. For some of the experiments, they also included pre-pandemic biopsies as controls!
4/

As is commonly found in these types of studies, many of the participants in the Long COVID group actually had fairly high levels of physical activity before they developed Long COVID.
For the majority of the people in that group, COVID forced them to reduce their activity.
5/
For the majority of the people in that group, COVID forced them to reduce their activity.
5/

They also conducted some basic physical and mental exertion tasks, and they found no major difference between the LC group and the healthy controls. That is, "there was no significant difference in the muscle's ability to produce force."
However, endurance took a hit.
6/


However, endurance took a hit.
6/


Likewise, they found no significant differences in the thickness of the muscles, and no significant differences in muscle fiber size between the Long COVID group and the healthy controls. There was also no difference in fiber type composition.
So what's going on?
7/
So what's going on?
7/

The muscle fibers seem to be morphologically healthy, so why aren't they working as intended?
The examination of the muscle fibers suggest that there might be some difference in mitochondrial activity within the cells. Mitochondria are the powerhouse of the cell!
8/
The examination of the muscle fibers suggest that there might be some difference in mitochondrial activity within the cells. Mitochondria are the powerhouse of the cell!
8/
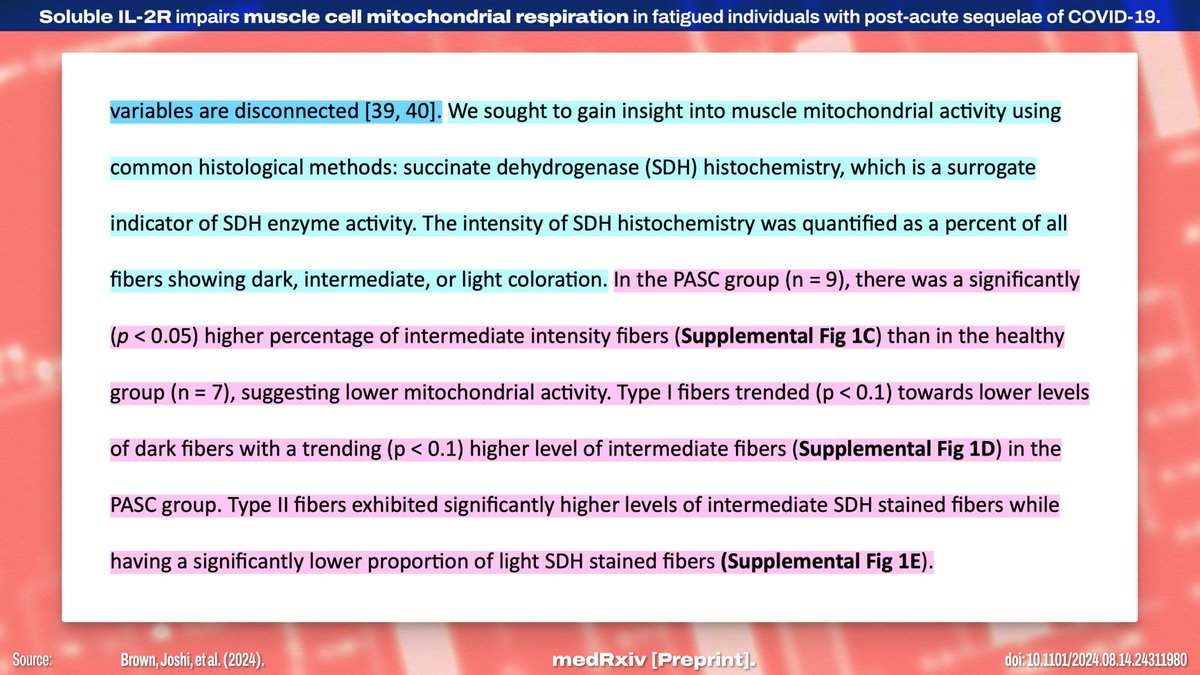
When they compared mitochondrial respiration between healthy controls and the LC group, they found a lower *quantity* of active mitochondria in the LC group, but the energy capacity of the present mitochondria seemed mostly unchanged.
9/
!["PASC participants have compromised skeletal muscle mitochondrial function. Several recent studies have linked PASC fatigue to reduced mitochondrial respiratory capacity in skeletal muscle [12, 41]. The observation that SDH activity differed in type II fibers prompted us to explore potential differences in mitochondrial respiration between healthy individuals and those with PASC. To investigate this, we used high resolution respirometry (HRR) to measure mitochondrial oxygen flux (JO2). State 3 respiration for complex I and combined complex I+II were significantly (p < 0.05) lower in PASC m...](/images/1px.png)



9/
!["PASC participants have compromised skeletal muscle mitochondrial function. Several recent studies have linked PASC fatigue to reduced mitochondrial respiratory capacity in skeletal muscle [12, 41]. The observation that SDH activity differed in type II fibers prompted us to explore potential differences in mitochondrial respiration between healthy individuals and those with PASC. To investigate this, we used high resolution respirometry (HRR) to measure mitochondrial oxygen flux (JO2). State 3 respiration for complex I and combined complex I+II were significantly (p < 0.05) lower in PASC m...](https://pbs.twimg.com/media/GVdzb3tWsAEOx5L.jpg)



On further examination, they found a similar pattern to the previous one.
These findings suggest "mainly mitochondrial content and not activity was lower in [LC] compared to healthy muscle." Electron microscopy also suggests the mitochondria are defective in some way.
10/


These findings suggest "mainly mitochondrial content and not activity was lower in [LC] compared to healthy muscle." Electron microscopy also suggests the mitochondria are defective in some way.
10/


They then asked if the reduced mitochondrial content is a result of deficient production of new mitochondria. The results indicate "that mitochondrial biogenesis was not impaired."
So like... what the fuck is happening here? To figure out the mechanism...
11/
So like... what the fuck is happening here? To figure out the mechanism...
11/

They examined the potential factors circulating in the blood. They identified sIL2R as "the most highly abundant circulating inflammatory marker, with the largest fold difference between healthy" and LC groups.
sIL2R is a receptor that comes from T cells!
12/
sIL2R is a receptor that comes from T cells!
12/

They treated some muscle cell tissue cultures with either sIL2R or the regular IL-2 cytokine.
They found the *baseline* oxygen consumption rate was unchanged, but the *maximum* respiration rate was limited by sIL2R specifically! This suggests a previously unknown pathway!
13/


They found the *baseline* oxygen consumption rate was unchanged, but the *maximum* respiration rate was limited by sIL2R specifically! This suggests a previously unknown pathway!
13/


What does this all mean? Despite no apparent differences in their muscles, those with LC fatigue "exhibited significant impairment of mitochondrial respiration across multiple components of the respiratory chain." sIL2R "emerged as the most significantly elevated factor."
14/
14/

Critically, elevated sIL2R levels are already:
1. Associated with muscle wasting.
2. A known biomarker that is "predictive of respiratory failure and ICU outcomes" in COVID!
Thus, the authors "posit that PASC fatigue is partially attributable to elevated systemic sIL2R."
15/
1. Associated with muscle wasting.
2. A known biomarker that is "predictive of respiratory failure and ICU outcomes" in COVID!
Thus, the authors "posit that PASC fatigue is partially attributable to elevated systemic sIL2R."
15/

The specifics of the effect sIL2R has are still unclear—although the authors have some hypotheses—but future research will need to explore this line of questioning further to pick apart the mechanism.
16/
16/

The study has a few limitations, but they're largely the type of limitations that would mean there's only a significant result if there's a large effect size to be measured! Of course, more research is needed to fully understand what's happening here.
17/
17/

Overall, these findings suggest "that mitochondria may function adequately under resting conditions but fail to meet increased energy demands during exertion," and that this "could explain post-exertional malaise" in LC despite otherwise normal muscle function.
18/
18/

This feels like a critical finding, and I agree with the authors' conclusion that their study "provides new insights into the physiological basis of" fatigue in Long COVID, opening "avenues for potential therapeutic interventions."
Source:
19/19 medrxiv.org/content/10.110…

Source:
19/19 medrxiv.org/content/10.110…

Huh. Latent herpesvirus reactivation leading to increased sIL2R… well that’s really the whole thing end-to-end isn’t it?
20/19
20/19
https://twitter.com/friesein/status/1826101973948481774
This quote is fascinating, because I’ve always thought the evidence lines up fairly well with post-infection chronic fatigue being the body’s rest-forcing illness response basically getting “stuck on.”
I wonder if sIL2R is a regulator for that process?
21/19
I wonder if sIL2R is a regulator for that process?
21/19
https://twitter.com/friesein/status/1826104385518059776
• • •
Missing some Tweet in this thread? You can try to
force a refresh





!["Data on BW consumption were obtained from the “Aspects of Daily Life” survey on households, conducted by the Italian National Institute of Statistics (ISTAT) [19]. ... The aim of the survey is to identify a variety of behavioral dimensions and aspects of daily life. ... We analyzed data from the 2021 edition of the survey, which included 45,597 individuals and 20,000 families, focusing on those who were 18 years or older at the time of the survey. ... a distinct stratum of municipalities with larger populations, labeled as self-representative (SR), and other municipalities, designated...](https://pbs.twimg.com/media/GVDBF48W4AAKDgi.jpg)









![Published August 5, 2024 in PLOS Pathogens: "SARS-CoV-2 spike-induced syncytia are senescent and contribute to exacerbated heart failure" "Author Summary In this paper, we directly linked SARS-2-S-triggered syncytium [fused cells] formation in the absence of infection with the ensuing induction of cellular senescence and its pathophysiological contribution to heart failure. We propose that both SARS-2-S expression and SARS-2-S protein internalization were sufficient to induce senescence in nonsenescent ACE2expressing cells. This is important because of the persistent existe...](https://pbs.twimg.com/media/GURP49TW0AAb71d.jpg)


!["Introduction ...Although symptoms resulting from infection typically resolve within weeks, some individuals experience persistent symptoms following the acute phase of COVID-19, the so-called post-acute sequelae of COVID-19 (PASC) or long COVID [2–4]. SARS-CoV-2 infection predominantly offends the respiratory system. Currently, evidence has suggested cardiac complications as one of the important pathogenic features of COVID-19 [5,6]. More importantly, compared with patients without heart failure, those with diagnosed heart failure experienced a longer length of hospital stay, increas...](https://pbs.twimg.com/media/GURP9_CWQAA3NX-.jpg)







