What is the DURATION of IMMUNITY? What is the IDEAL INTERVAL between TWO VACCINATIONS?
Immunity varying among individuals and vaccine effectiveness changing depending on variants, a vaccination strategy can only recommend a sufficiently wide interval.
journals.plos.org/plosone/articl…

Immunity varying among individuals and vaccine effectiveness changing depending on variants, a vaccination strategy can only recommend a sufficiently wide interval.
journals.plos.org/plosone/articl…

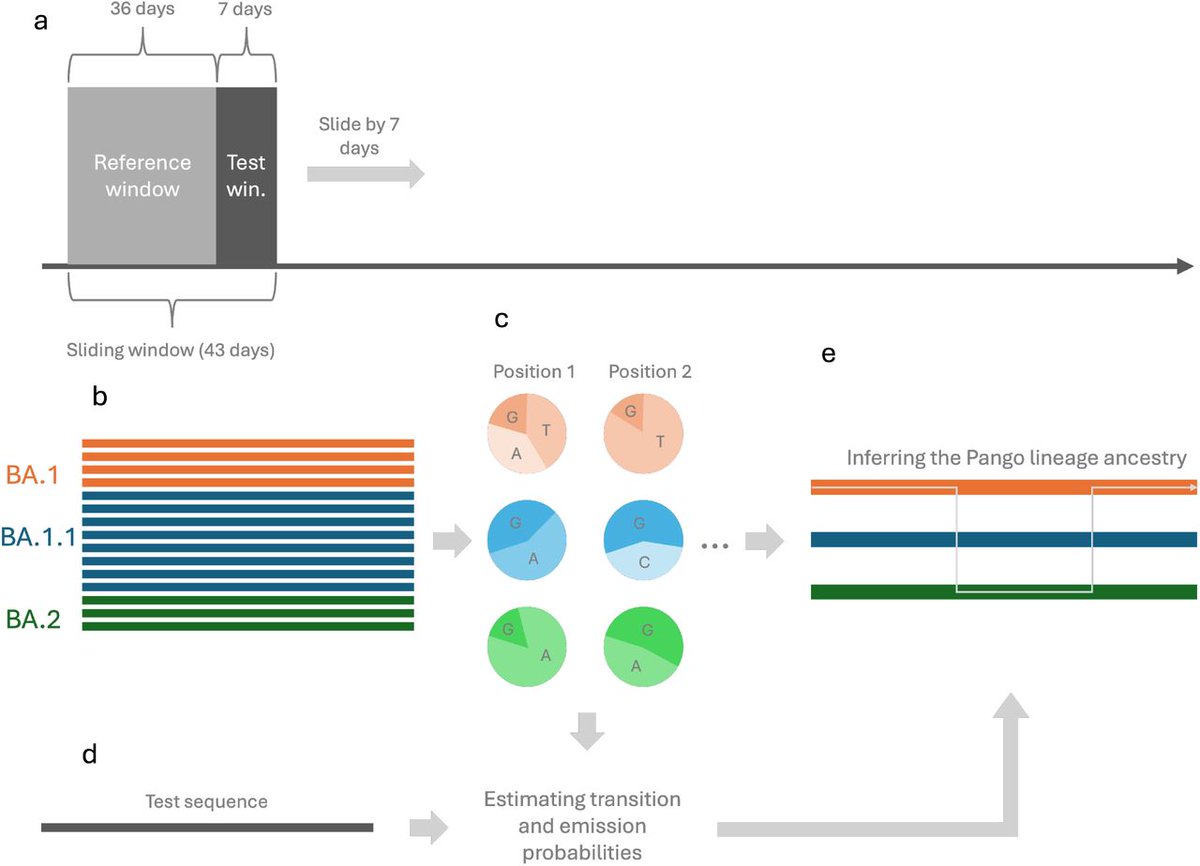
2) The study presents a comprehensive model to understand disease outbreaks and vaccination strategies. The model considers factors like comorbidity and multiple vaccine doses to analyze epidemic dynamics. 

3) The key findings:
- The gap between vaccine doses is crucial - it can significantly impact disease spread. Frequent vaccination may not always be necessary and can reduce immunity over time.
- The gap between vaccine doses is crucial - it can significantly impact disease spread. Frequent vaccination may not always be necessary and can reduce immunity over time.

4)- Determining the optimal dosing interval is critical. It should balance factors like immunity levels, vaccine efficacy, and emerging virus variants to effectively manage the disease. 

5) - The presence of multiple circulating strains can affect the frequency and severity of epidemic peaks. Optimizing the dose interval can build lasting immunity, reducing the need for frequent vaccination. 

6)- An optimal control strategy is proposed to minimize both infections and vaccination costs by finding the right gap between doses based on population immunity. 

7) The model provides a versatile framework that can be adapted for different diseases. It challenges the common assumption that frequent vaccination is always better, emphasizing the need for a more nuanced, cost-effective approach to disease control. 

8) The study acknowledges limitations like homogeneous population assumption, equal vaccine effectivness and lack of granular data.
In summary, the optimal time between two vaccine doses is not a one-size-fits-all solution, but rather ...
In summary, the optimal time between two vaccine doses is not a one-size-fits-all solution, but rather ...

9) ...should be determined by carefully analyzing the population immunity, vaccine efficacy, and cost-effectiveness factors. The study suggests a range of 3-8 months as a potentially optimal interval based on the modeling results.
Thanks for reading 🙏
Thanks for reading 🙏
• • •
Missing some Tweet in this thread? You can try to
force a refresh