1/ A 🧵 on the latest (preprint) paper by @CGATist et. al. The paper mentions that "Significant female and male traits were indicative of chronic inflammation, insulin resistance and liver disease" : Tagging @JennieJacques1 medrxiv.org/content/10.110…
2/ Differentially expressed proteins were used as inputs to the software framework I have been using in order to identify promising research targets. Note that "Liver disease" has been identified as early as 2017 as a potential target using certain analytical methods.




3/ Moreover, on a document I circulated among #MECFS researchers in 2017, issues with Glucose metabolism and Inflammatory processes have been also identified ("Liver disease" also mentioned) : 

4/ We begin with differentially expressed proteins appearing on Figure 5. A ranking is generated according to the relevance of each medical topic. Below are the results. Note the relevance of "protein stability" and transferases among others : 

5/ Next, the same ranking is generated for proteins appearing on figure 6c. Here are the rankings for males and females :


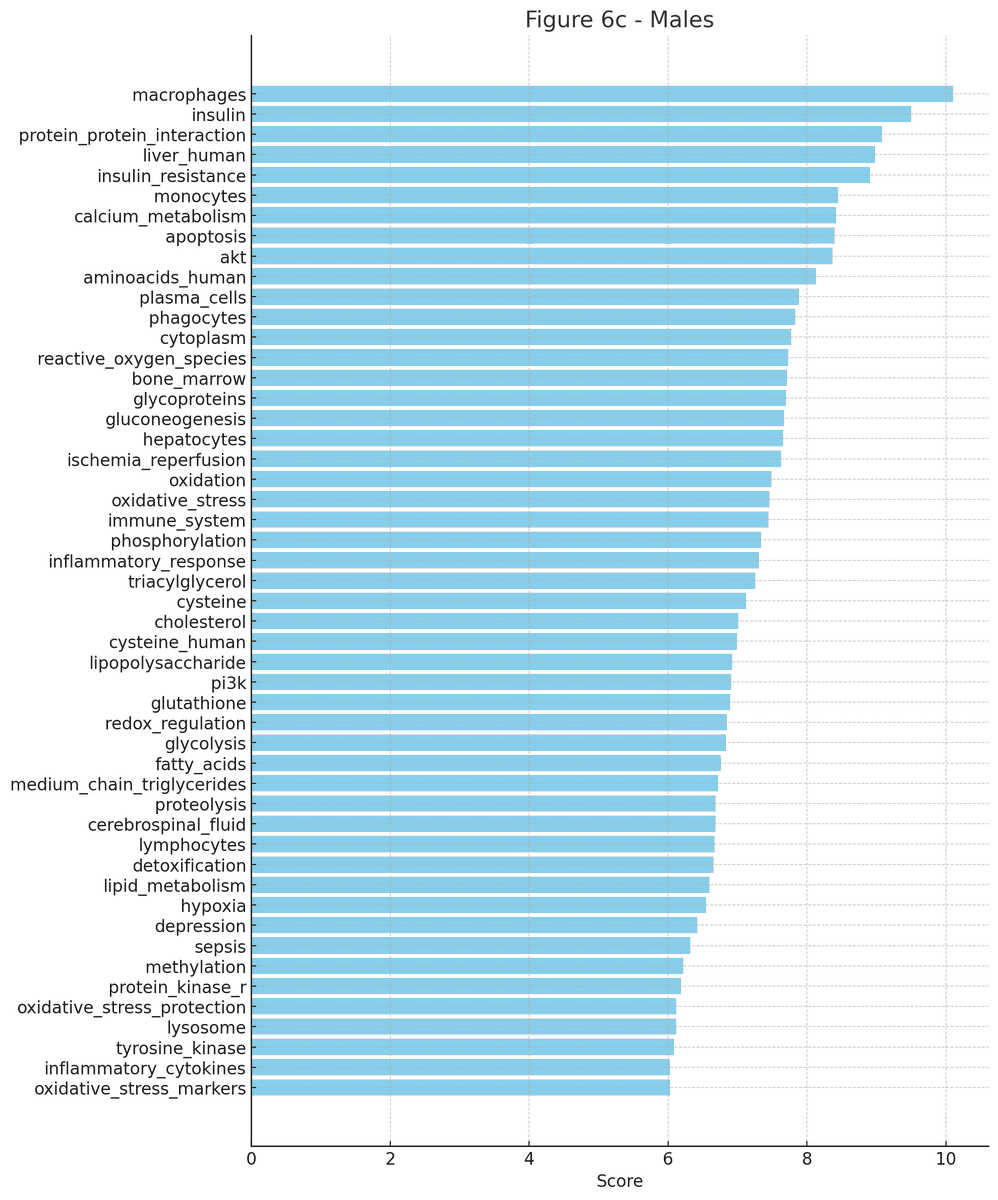

6/ ..and from the same figure (6c) below is the relevance ranking of proteins that were found to be differentially expressed in both males and females. Note the high ranking of the liver and transferases. 

7/ Transferases is one of the concepts that consistently received very high rankings. And there was evidence about this as early as 2017. From the same document mentioned in (3) : 

8/ According to #ChatGPT, the following are factors that affect transferases functioning. Tagging @scott_scientist for environmental toxins. Note the mention on "Protein folding" which is directly related to ER Stress (found in #MECFS patients by Hwang ) et.al



• • •
Missing some Tweet in this thread? You can try to
force a refresh




















