This time, we developed a nasal booster vaccine for influenza viruses. In this preprint, @MiyuMoriyama et al. show that nasal boosters with unadjuvanted hemagglutinin protein induce sterilizing immunity in mice against flu. (1/)
biorxiv.org/content/10.110…
biorxiv.org/content/10.110…
This work builds on the Prime and Spike vaccine strategy by @tianyangmao @BenIsraelow et al. against COVID where mRNA vaccine followed by nasal booster with recombinant spike protein established local immunity, ⬇️ infection & transmission in rodents. (2/)
science.org/doi/10.1126/sc…
science.org/doi/10.1126/sc…
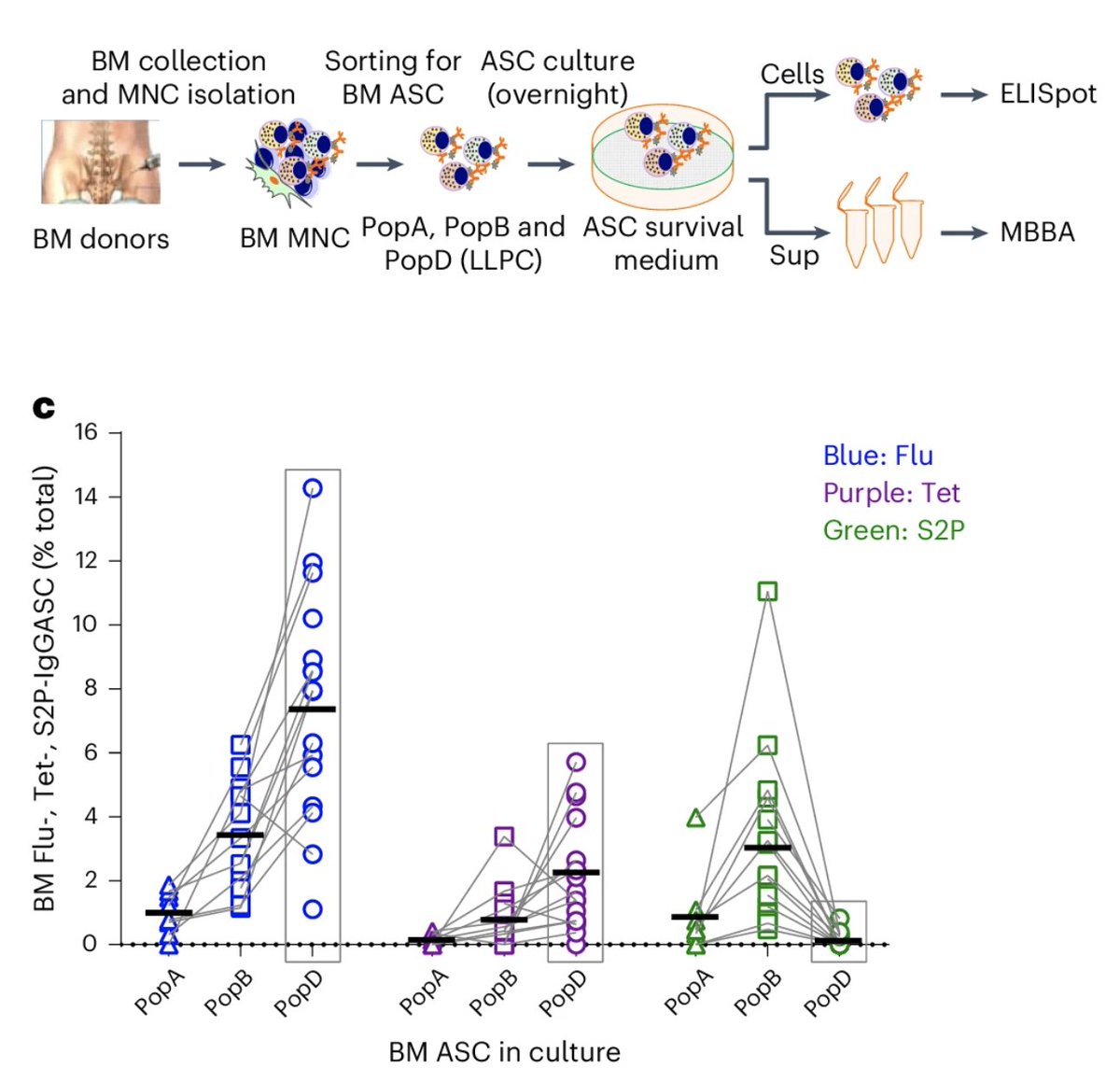
For Prime and HA against flu, @MiyuMoriyama tested several different mRNA IM prime and nasal HA booster doses, followed by a homologous influenza virus challenge. Like Prime and Spike, no adjuvant is needed for the nasal booster due to preexisting immunity from Prime. (3/) 

Intramuscular HA mRNA (2 doses) followed by a recombinant HA nasal booster induced sterilizing immunity against homologous viral challenge in the nose and lung leading to no weight loss or pathology from infection (4/) 
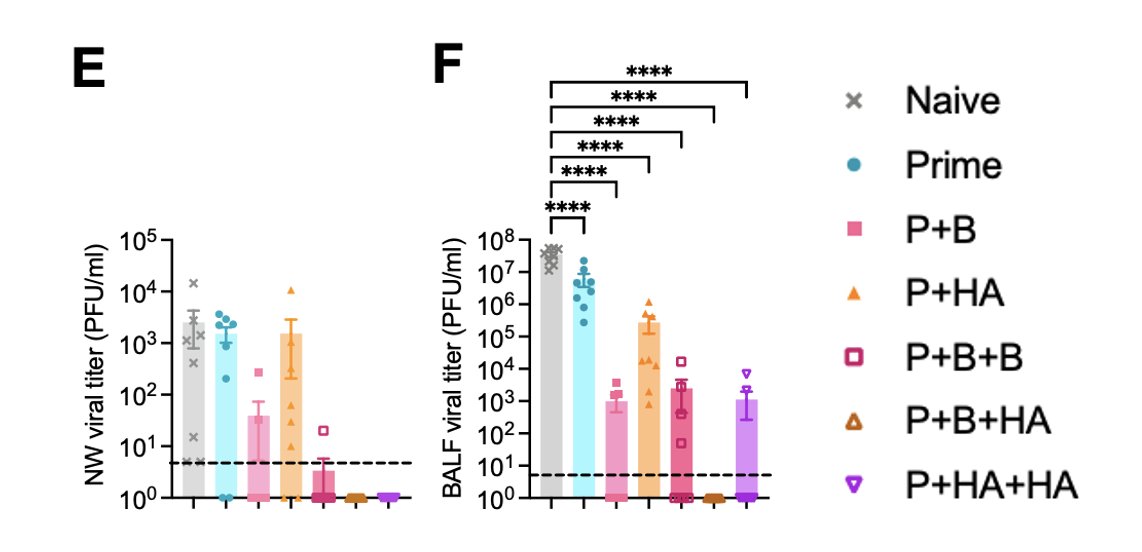
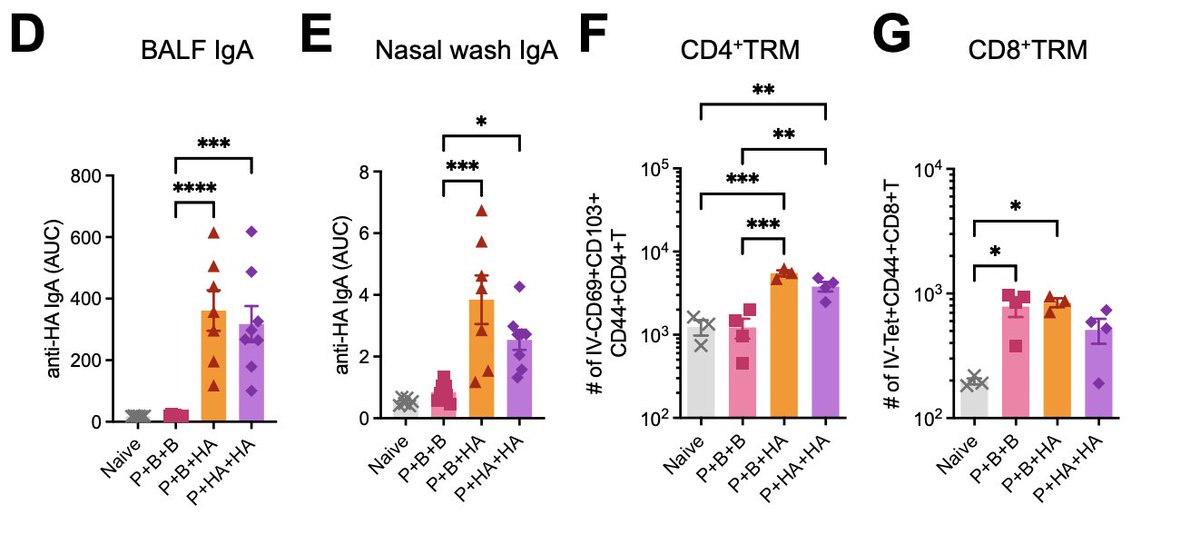
How does this happen? Prime and HA (P+B+HA or P+HA+HA), but not IM mRNA vaccines alone (P+B+B), induce robust nasal and lung IgA production, and tissue-resident memory CD4 T cells. (5/) 
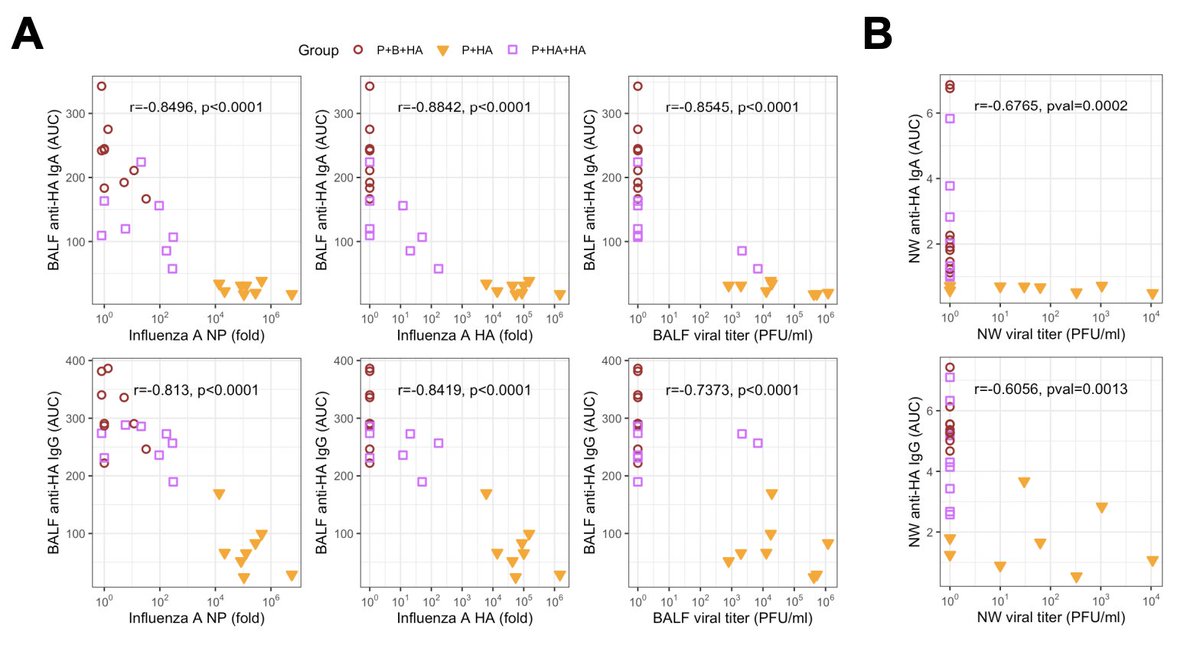
Mucosa IgA and IgG inversely correlated with viral burden in the respiratory tract. Note the interesting results for mucosal IgA and viral load. There appears to be a threshold of IgA above which virus replication is shut down 🤯 (6/) 
Older adults above age 65 years are at higher risk of developing severe and lethal influenza infections. @MiyuMoriyama next tested the Prime and HA vaccine approaches in older mice and showed that they can be protected from disease. (7/) 
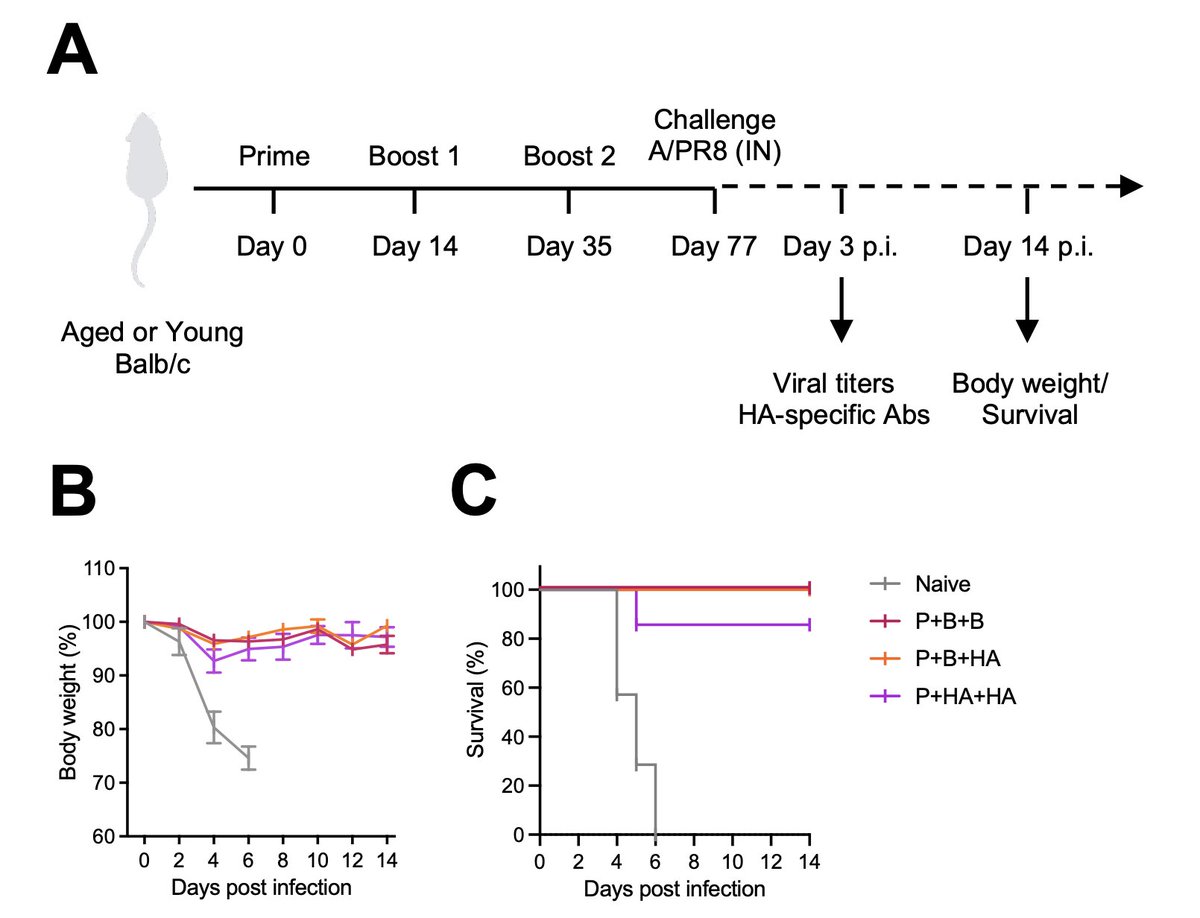
However, unlike younger mice, sterilizing immunity was not achieved in older mice in the lung (BALF) or nose (NW). Yet, 2 doses of HA mRNA vaccine followed by nasal HA booster (P+B+HA) did reduce viral load in the lung better than 3 doses of IM mRNA (P+B+B) in older mice. (8/) 

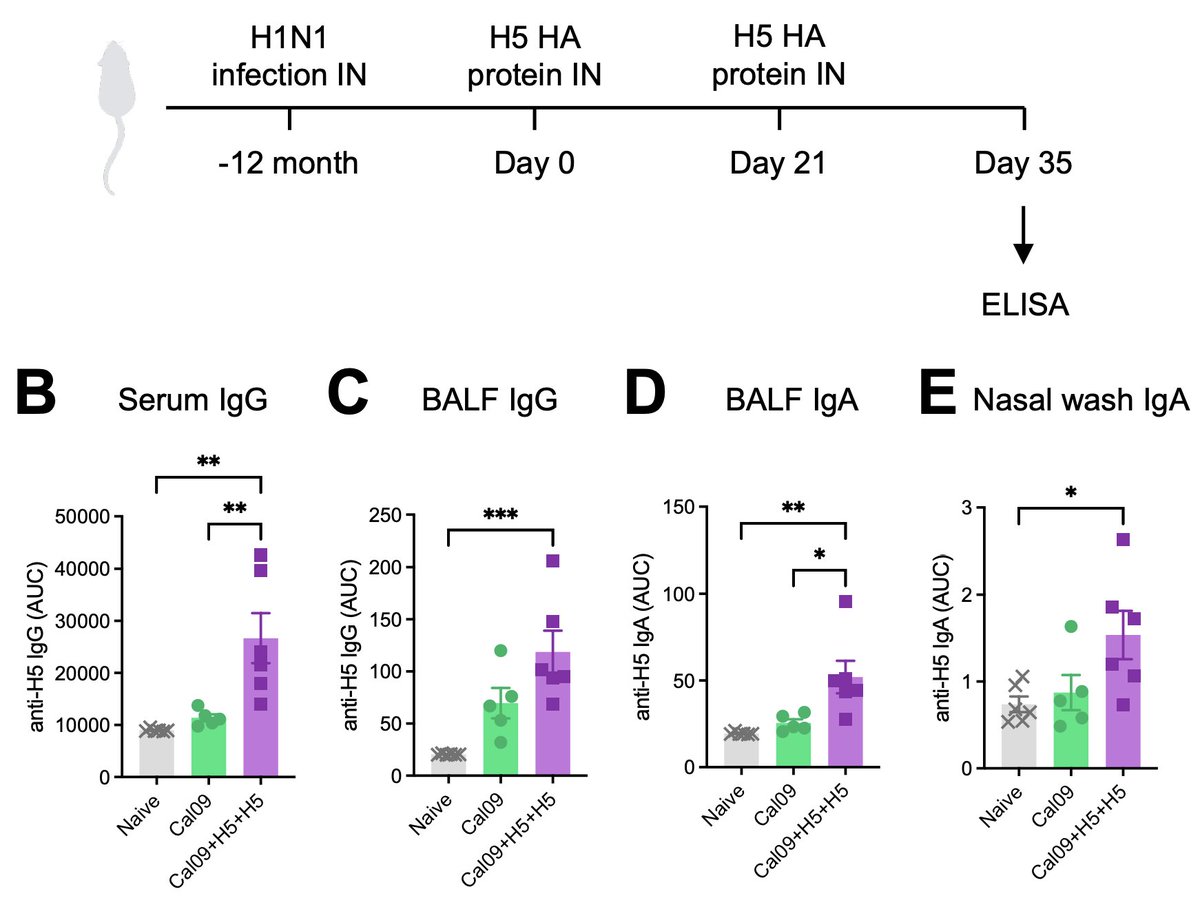
Can we adapt Prime and HA for avian flu? Yes! When two doses of nasal boosters of H5 HA protein were given to mice that recovered from an H1N1 infection a year ago (thus mimicking immunity in people), mice developed robust anti-H5 antibody responses. (9/) 
Finally, we show that nasal boosters with a mixture of HA from homologous (same HA as the Prime) and a heterologous influenza A virus (P+HAm+HAm) can confer sterilizing immunity against a heterologous viral challenge 💥 (10/) 

I wish to highlight the incredible work of the amazing team led by @MiyuMoriyama. We continue to strive to develop safe and effective vaccines against mucosal pathogens that can prevent infection and transmission. Grateful to @niaidcivics for the support 🙏 (end) 
• • •
Missing some Tweet in this thread? You can try to
force a refresh