Deep dive on #EARLYTAVR from ##TCT2024
Lots already said & discussed
It takes time to read the paper, read the supplementary appendix, analyse the results, think about them etc!
Some thoughts...🧵
Lots already said & discussed
It takes time to read the paper, read the supplementary appendix, analyse the results, think about them etc!
Some thoughts...🧵

On Sunday I wrote a thread about asymptomatic severe AS and what we knew already from RECOVERY & AVATAR RCTs and what the guidelines currently advocate
Here's the 🧵 in case you missed it
Here's the 🧵 in case you missed it
https://x.com/dr_benoy_n_shah/status/1850645694698135554?t=TAVDsW79WuDguZBGOutVBg&s=19
EARLY TAVR
Asymptomatic severe AS patients recruited between March '17 - Dec '21
75 sites across 🇺🇲 and 🇨🇦
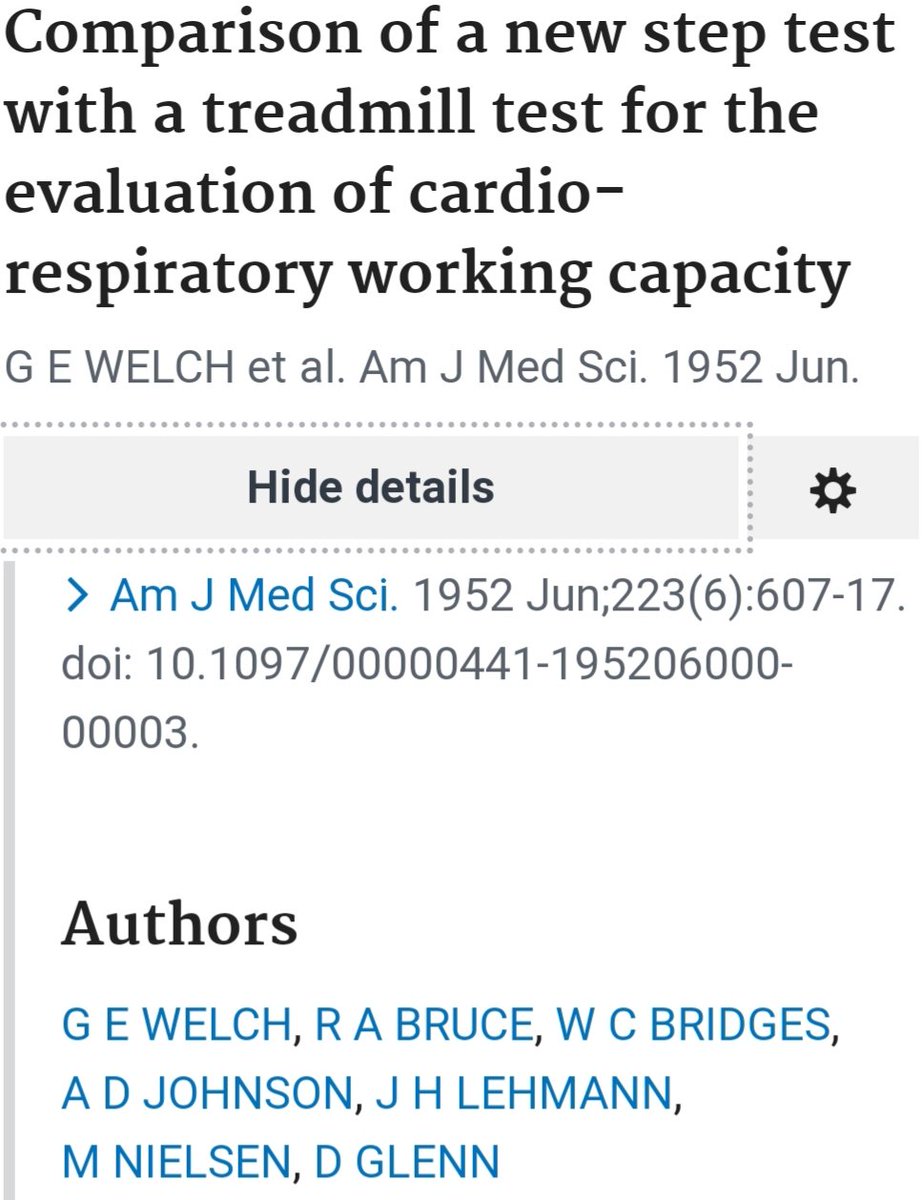
Asymptomatic status confirmed by negative treadmill test in 90.6%
(Remaining 9.4% unable to do test, relied on detailed physician history)
That's a good % that did ETT 👏
Asymptomatic severe AS patients recruited between March '17 - Dec '21
75 sites across 🇺🇲 and 🇨🇦
Asymptomatic status confirmed by negative treadmill test in 90.6%
(Remaining 9.4% unable to do test, relied on detailed physician history)
That's a good % that did ETT 👏
1578 patients screened, 901 randomized (57%)
Of the screen fails, 213/677 (31.5%) due to anatomical factors making TAVI either unsuitable or unattractive
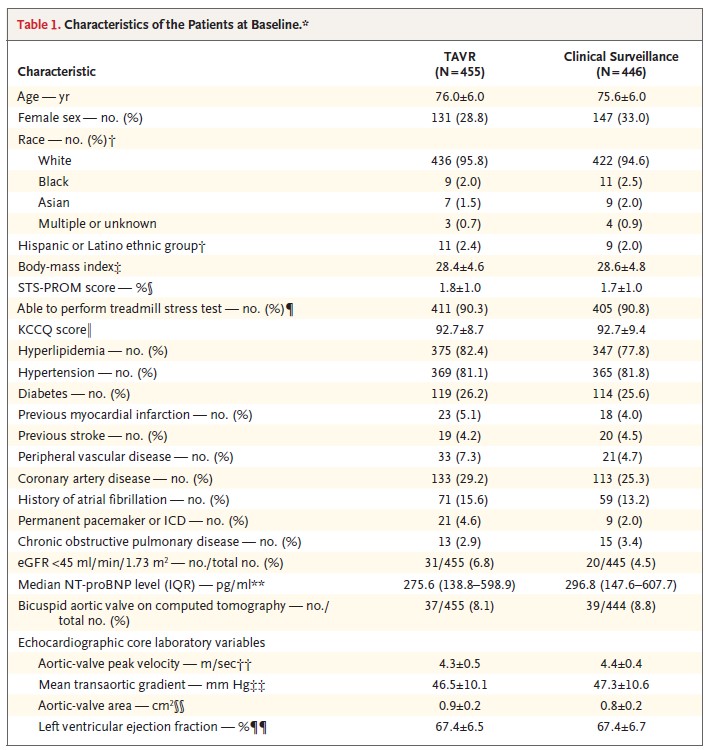
455 randomized to TAVI
446 randomized to 'clinical surveillance' [CS] (aka 'watchful waiting')
Of the screen fails, 213/677 (31.5%) due to anatomical factors making TAVI either unsuitable or unattractive
455 randomized to TAVI
446 randomized to 'clinical surveillance' [CS] (aka 'watchful waiting')

Key demographics:
Mean age 75.8yrs
31% women
95% Caucasian
Mean STS score 1.8%
>80% considered low risk locally
Mean AV Vmax 4.3m/s
Mean LV EF 67%
Bicuspid AV in 8.4%
If randomised to TAVI, mean time to TAVI was...14 days!
Mean age 75.8yrs
31% women
95% Caucasian
Mean STS score 1.8%
>80% considered low risk locally
Mean AV Vmax 4.3m/s
Mean LV EF 67%
Bicuspid AV in 8.4%
If randomised to TAVI, mean time to TAVI was...14 days!
TAVI procedure - nearly 20% under general anaesthesia!
Why? Is that still common in North America?
I think in most European countries, GA is used in <1% cases...
In total across both groups, valve sizes:
20mm - 17
23mm - 256
26mm - 387
29mm - 155
21-26% CEP devices used
Why? Is that still common in North America?
I think in most European countries, GA is used in <1% cases...
In total across both groups, valve sizes:
20mm - 17
23mm - 256
26mm - 387
29mm - 155
21-26% CEP devices used

CS group details
388/446 underwent TAVI
Median time from randomisation to TAVI = 11 months
Median time to intervention 32days
388/446 underwent TAVI
Median time from randomisation to TAVI = 11 months
Median time to intervention 32days
Median follow-up 3.8yrs
Composite primary EP (death, stroke, unplanned CV hospitalization) occurred in 122 (26.8%) in TAVI cohort vs 202 (45.3%) in CS cohort (95% CI 0.40-0.63, p<0.001)
11 deaths in CS group before crossing over to intervention, including 2 within 1st 6 months

Composite primary EP (death, stroke, unplanned CV hospitalization) occurred in 122 (26.8%) in TAVI cohort vs 202 (45.3%) in CS cohort (95% CI 0.40-0.63, p<0.001)
11 deaths in CS group before crossing over to intervention, including 2 within 1st 6 months


Trial conclusion
Early TAVI in asymptomatic severe AS patients reduced the composite EP of all-cause death, stroke & unplanned hospitalization for CV causes
Early TAVI in asymptomatic severe AS patients reduced the composite EP of all-cause death, stroke & unplanned hospitalization for CV causes
ANALYSIS
Quite a lot to consider here
Let's go in order, starting with the choice of primary EP and how 'unplanned hospitalization' was defined
They said that any TAVI in the surveillance group within 6/12 of randomisation would be an unplanned hospitalization...
Quite a lot to consider here
Let's go in order, starting with the choice of primary EP and how 'unplanned hospitalization' was defined
They said that any TAVI in the surveillance group within 6/12 of randomisation would be an unplanned hospitalization...

Now, in the Appendix is this extract within a table
You may be wondering what the column headings are...look at the second image
Yes, the *SPONSOR* chose this (by the look of this table)
I don't think TAVI within 6 months of randomisation is a failure of the strategy, imho

You may be wondering what the column headings are...look at the second image
Yes, the *SPONSOR* chose this (by the look of this table)
I don't think TAVI within 6 months of randomisation is a failure of the strategy, imho


Patients with asymptomatic severe AS that have a reassuring exercise test & are told 'see you in 6 months for review' are ALSO told to report new symptoms and NOT wait until that 6/12 appointment
So, if after 4 months they report new dyspnoea or chest pain, then you arrange Rx
So, if after 4 months they report new dyspnoea or chest pain, then you arrange Rx
They would then be scheduled to be admitted for a planned procedure. Sooner than initially anticipated, sure, but that's exactly how watchful waiting works...
I think it's reasonable to count it as an unplanned hospitalization IF they're admitted with decompensation
But...
I think it's reasonable to count it as an unplanned hospitalization IF they're admitted with decompensation
But...
If I have understood this table in the Suppl appendix correctly, then only 44 of the 377 (11.7%) patients with new symptoms were acutely hospitalised, the rest had new symptoms but didn't need hospital admission (I think?) 

Why is this relevant?
Because *105* patients initially allocated to CS crossed over to TAVI within 6 months of randomisation
So, 105 of the 202 events in the CS arm were unplanned hospitalization within 6m of randomisation, but I believe only 44 were acute hospitalizations
Because *105* patients initially allocated to CS crossed over to TAVI within 6 months of randomisation
So, 105 of the 202 events in the CS arm were unplanned hospitalization within 6m of randomisation, but I believe only 44 were acute hospitalizations
If you don't count those patients that had a scheduled TAVI (i.e. they came in from home for it electively, had it then went home again) then that primary EP difference almost certainly disappears
We should also talk about how many patients seemed to develop symptoms so soon...
We should also talk about how many patients seemed to develop symptoms so soon...
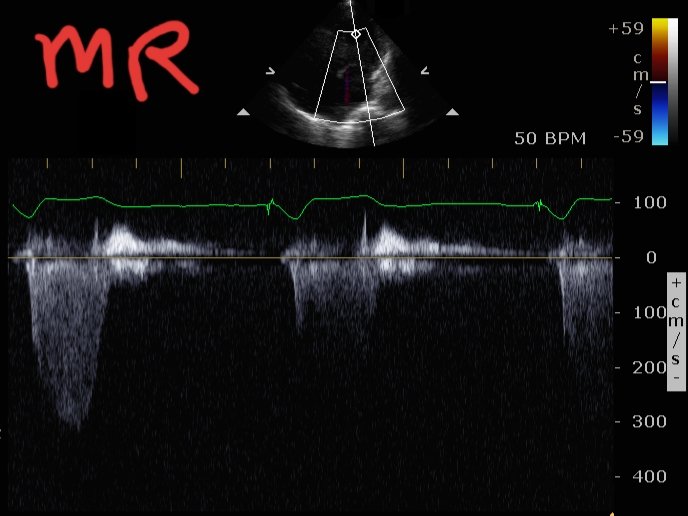
I must say I'm really surprised how many patients seemed to develop symptoms within 6 months
Why? Because they almost all had just had reassuring exercise tests!
I do treadmill tests routinely in asymptomatic severe AS patients, when they perform well it's rare they develop...

Why? Because they almost all had just had reassuring exercise tests!
I do treadmill tests routinely in asymptomatic severe AS patients, when they perform well it's rare they develop...


symptoms before their 6m visit
I find it hard to understand how so many patients, having just proven asymptomatic status with normal haemodynamic response to exercise, seemed to deteriorate so quickly
I don't see that in my routine practice
I find it hard to understand how so many patients, having just proven asymptomatic status with normal haemodynamic response to exercise, seemed to deteriorate so quickly
I don't see that in my routine practice
The reason this point is crucial is look at this KM curve...such a steep slope immediately after randomisation and then from 6months on the curves are parallel, literally superimposable without that early spike of unplanned hospitalizations! 🧐
@drjohnm
@drjohnm

So, do I think the trial design, and in particular selection of the composite EP (and definition of unplanned hospitalization) reveals bias in the trial?
Of course! But...
What did you expect?! Has there been an Industry-sponsored TAVI trial yet that didn't meet its primary EP?
Of course! But...
What did you expect?! Has there been an Industry-sponsored TAVI trial yet that didn't meet its primary EP?
I've said it before & will say it again. We should not criticise Industry or the docs doing these trials. They're not breaking any rules or laws
It's the regulator that allows the company that makes the device to run the crucial phase 3 trials that determine subsequent $$$
It's the regulator that allows the company that makes the device to run the crucial phase 3 trials that determine subsequent $$$
It's a crazy set-up
If you're Edwards & your stock price will improve if you deliver a new market (asymptomatic severe AS) and the regulator allows you to design, conduct & run the key trial that will determine if your stock price goes ⬆️ or ⬇️, *obviously* you'd game it!
If you're Edwards & your stock price will improve if you deliver a new market (asymptomatic severe AS) and the regulator allows you to design, conduct & run the key trial that will determine if your stock price goes ⬆️ or ⬇️, *obviously* you'd game it!
That's not illegal, I would do exactly the same if I were in their shoes!
It's the FDA / EMEA / MHRA etc that need much higher standards, but I fear that ship has sailed
Industry should, ideally, provide the devices for the trial but have NO involvement in the trial itself
It's the FDA / EMEA / MHRA etc that need much higher standards, but I fear that ship has sailed
Industry should, ideally, provide the devices for the trial but have NO involvement in the trial itself
Anyway, back to EARLY TAVR
Final point - it's important to remember that with severe AS, it's not really a question of IF you need treatment, but rather WHEN
These patients don't have a medical therapy option, it's valve intervention or conservative (i.e. palliative) care
Final point - it's important to remember that with severe AS, it's not really a question of IF you need treatment, but rather WHEN
These patients don't have a medical therapy option, it's valve intervention or conservative (i.e. palliative) care
So, although we can argue about trial semantics, important to remember that in reality, the most you can realistically delay treatment by is maybe 18-24 months? I know there are data showing you can monitor for 3-4 yrs but I feel that is v risky
We have to accept that there IS a small but real risk of sudden death with watchful waiting and there is of course the risk of adverse cardiac remodelling
⬆️ LVH
⬇️ LV EF (even if still >50%)
Diastolic dysfunction
LA enlargement --> ⬆️ risk AF
⬆️ LVH
⬇️ LV EF (even if still >50%)
Diastolic dysfunction
LA enlargement --> ⬆️ risk AF

So, in the end, I think you have to explain PROs and CONs of early intervention vs watchful waiting / surveillance to patients and they will often have an opinion based on inherent personality & personal preference/ approach to risk
RECOVERY trial --> benefit for earlier intervention
AVATAR trial --> benefit to earlier intervention
EARLY TAVR trial --> benefit to earlier intervention (albeit with above caveats re primary EP definition)
So is there still a role for clinical surveillance?
Yes, in some...
AVATAR trial --> benefit to earlier intervention
EARLY TAVR trial --> benefit to earlier intervention (albeit with above caveats re primary EP definition)
So is there still a role for clinical surveillance?
Yes, in some...
For clinical surveillance, I think follow-up has to be vigilant, patients need to know to contact you as soon as there's a change AND you must have a healthcare system that can deliver TAVI / SAVR *promptly* once symptoms arise
If you don't have those, go for intervention
End/
If you don't have those, go for intervention
End/
• • •
Missing some Tweet in this thread? You can try to
force a refresh