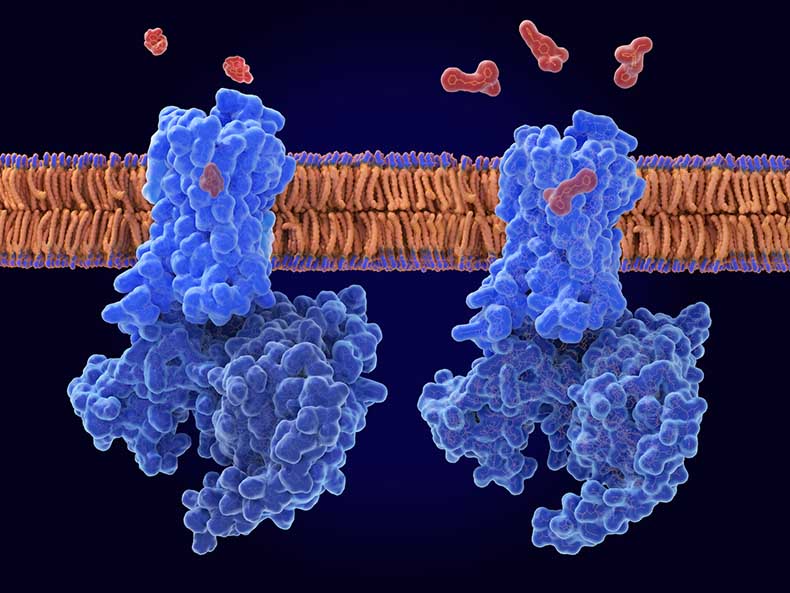
🧵 1/ This is the mu-opioid receptor 🧵
It plays a crucial role in attachment, reward, social bonding and pain.
🚀Understanding Borderline Personality Disorder (BPD) as an Interpersonal Pain Syndrome 👇
It plays a crucial role in attachment, reward, social bonding and pain.
🚀Understanding Borderline Personality Disorder (BPD) as an Interpersonal Pain Syndrome 👇
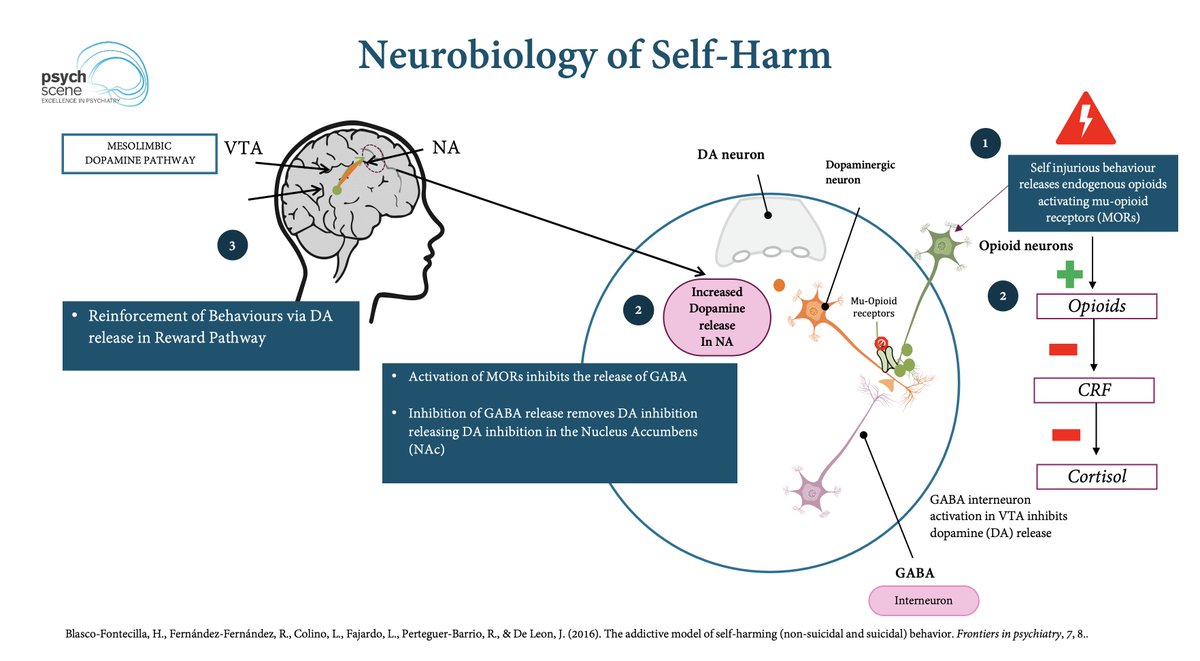
1/ BPD and Pain Sensitivity: Evidence shows that individuals with BPD often present atypical pain responses, with up to 80% displaying reduced pain perception during non-suicidal self-injury (NSSI) episodes.
This phenomenon may stem from opioidergic system dysregulation, where neurobiological shifts alter pain processing in the brain.
This phenomenon may stem from opioidergic system dysregulation, where neurobiological shifts alter pain processing in the brain.
2/Chronic Pain and BPD: Studies reveal that up to 65% of BPD patients experience chronic pain, which not only exacerbates emotional dysregulation but also predicts lower likelihood of remission.
3/ EOS and Emotional Dysregulation: The Endogenous Opioid System (EOS)- a neuromodulatory network crucial for mood, reward, and social bonding- plays a key role in BPD.
Components like mu-opioid receptors (MOR) and kappa-opioid receptors (KOR) modulate pleasure, pain, and the stress response, forming the foundation of pain abnormalities in BPD.
Components like mu-opioid receptors (MOR) and kappa-opioid receptors (KOR) modulate pleasure, pain, and the stress response, forming the foundation of pain abnormalities in BPD.
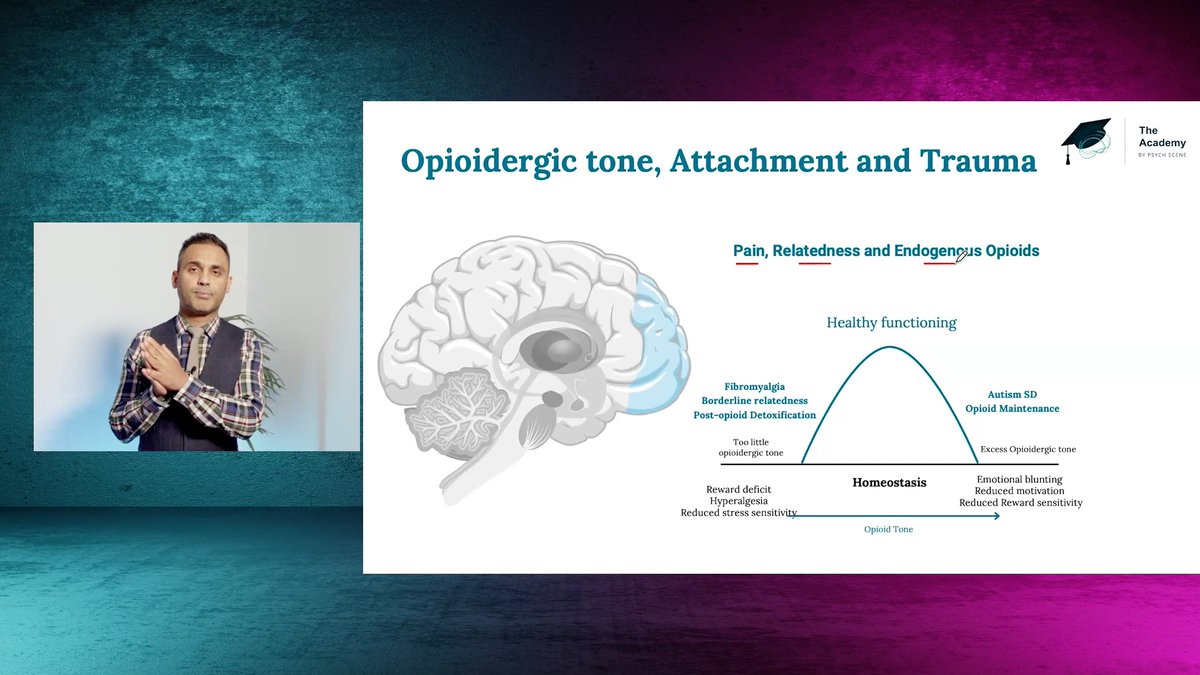
4/ In typical pain processing, MORs provide analgesia and reward signals, while KORs contribute to stress-induced dysphoria.
Childhood trauma and chronic stress disrupt this balance, often leading to hypomethylation of the OPRK1 gene, which boosts KOR expression and contributes to the emotional numbness and dysphoria characteristic of BPD.
Childhood trauma and chronic stress disrupt this balance, often leading to hypomethylation of the OPRK1 gene, which boosts KOR expression and contributes to the emotional numbness and dysphoria characteristic of BPD.

5/ Reduced MOR Activity: Neglect or social isolation can lead to under-stimulated MORs, impairing emotional bonding and reward processing.
To compensate, individuals with BPD might turn to behaviours like substance use or self-injury as attempts to restore EOS activity and alleviate emotional pain.
Clinical implications: Clinical trials involving opioid antagonists, such as naltrexone and buprenorphine (KOR antagonist), have shown promising results in reducing self-harming behaviours by blunting the rewarding effects typically associated with these actions.
To compensate, individuals with BPD might turn to behaviours like substance use or self-injury as attempts to restore EOS activity and alleviate emotional pain.
Clinical implications: Clinical trials involving opioid antagonists, such as naltrexone and buprenorphine (KOR antagonist), have shown promising results in reducing self-harming behaviours by blunting the rewarding effects typically associated with these actions.
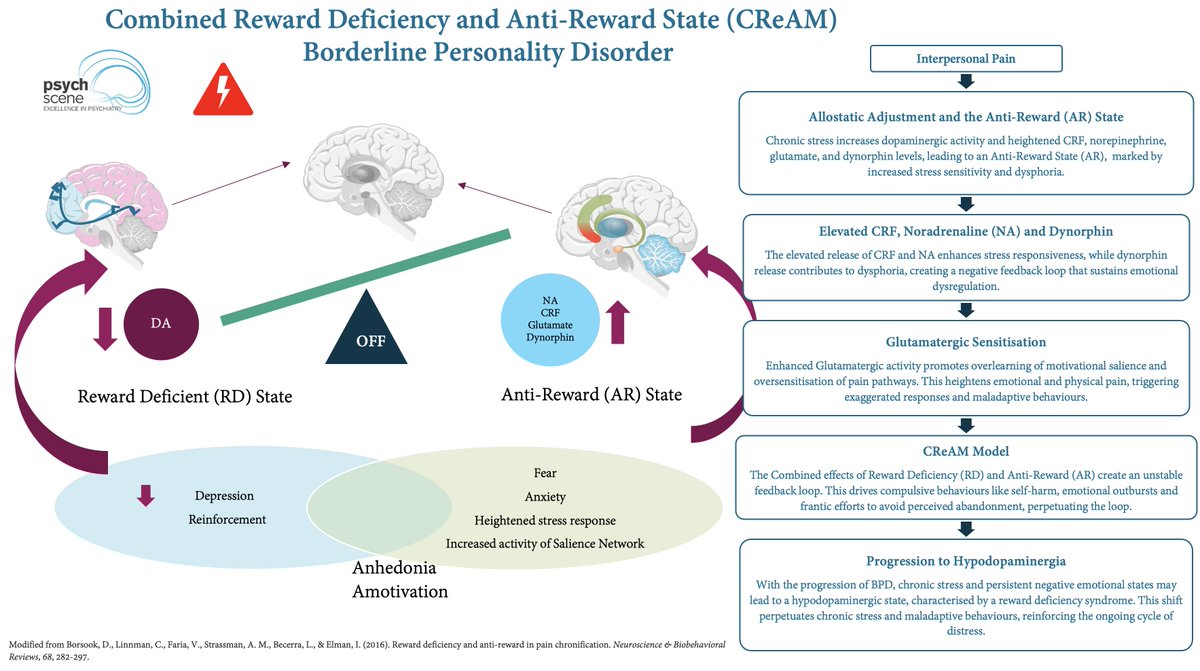
7/ Interpersonal Pain and Neuroadaptation in BPD: The Allostatic and CReAM Models
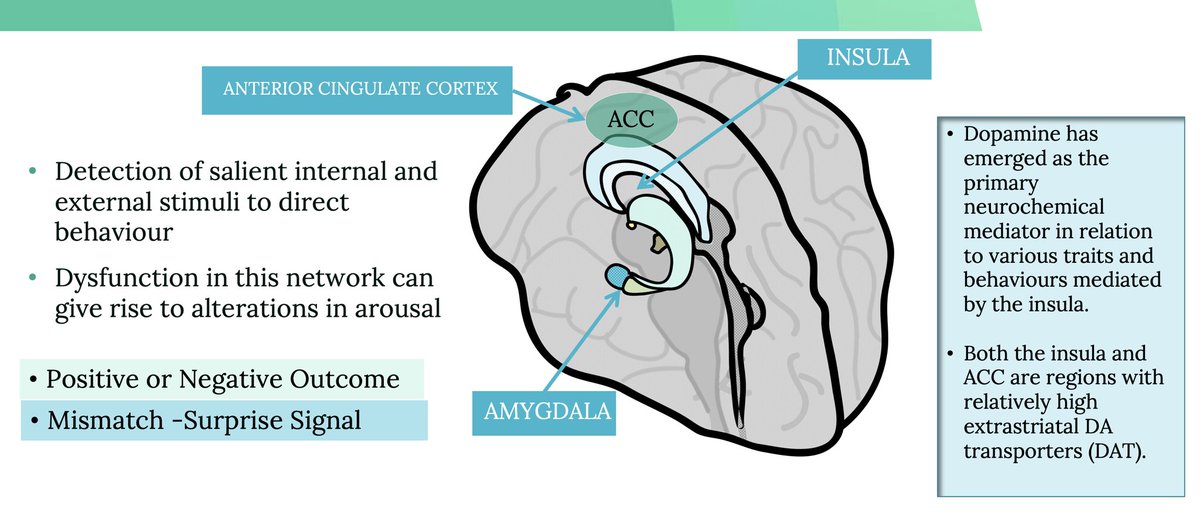
Initially, relational stress potentiates dopaminergic trafficking, but over time, prolonged stress shifts patients into a Reward Deficiency (RD) state marked by anhedonia and low motivation.
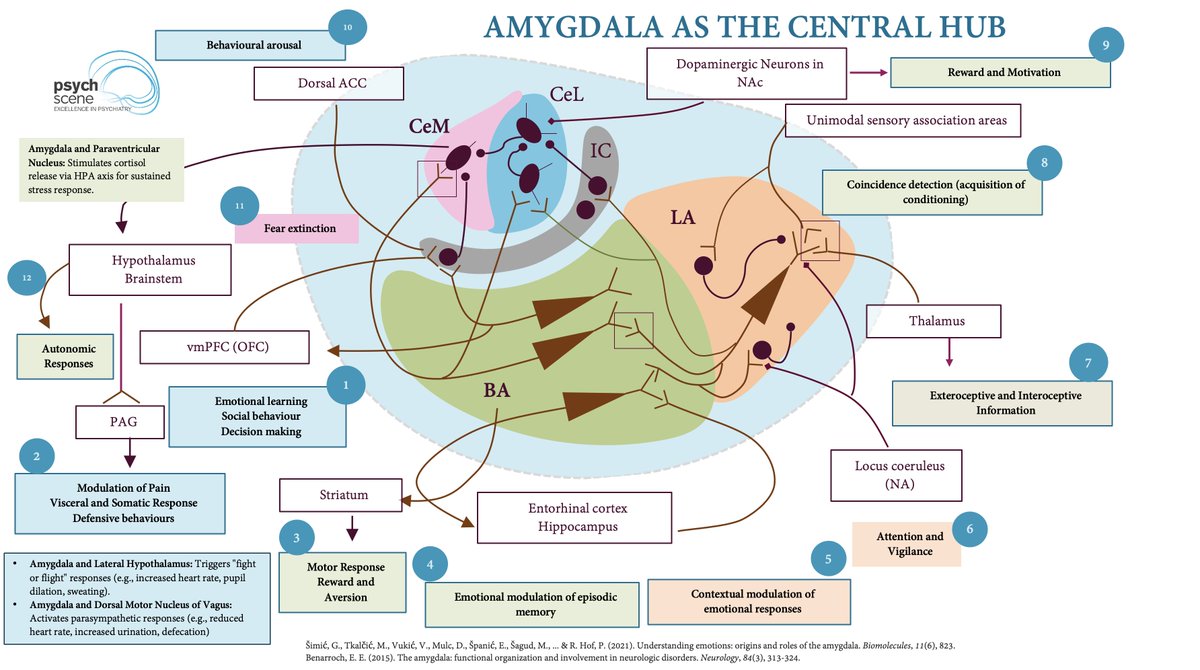
Neuroadaptations involving the amygdala and brainstem elevate CRF, norepinephrine, and dynorphin, reinforcing an Anti-Reward (AR) State and compounding chronic psychological pain.
Initially, relational stress potentiates dopaminergic trafficking, but over time, prolonged stress shifts patients into a Reward Deficiency (RD) state marked by anhedonia and low motivation.
Neuroadaptations involving the amygdala and brainstem elevate CRF, norepinephrine, and dynorphin, reinforcing an Anti-Reward (AR) State and compounding chronic psychological pain.
8/ Engel’s Lens on Pain: Developmental Roots of Relational Instability in BPD:
"We discover that in the course of the child’s development, pain and relief of pain enter into the formation of interpersonal (object) relations and into the concepts of good and bad, reward and punishment, success and failure. Pain becomes par excellence a means of assuaging guilt and thereby influences object relationships". [Engel, 1959]
In Borderline Personality Disorder (BPD), this link is important as early disruptions in processing pain and comfort within relationships can lead to heightened sensitivity to rejection and a cycle of relational instability.
"We discover that in the course of the child’s development, pain and relief of pain enter into the formation of interpersonal (object) relations and into the concepts of good and bad, reward and punishment, success and failure. Pain becomes par excellence a means of assuaging guilt and thereby influences object relationships". [Engel, 1959]
In Borderline Personality Disorder (BPD), this link is important as early disruptions in processing pain and comfort within relationships can lead to heightened sensitivity to rejection and a cycle of relational instability.
9/Zanarini’s Perspective: The “Pain of Being Borderline” :
Zanarini et al. highlighted that individuals with Borderline Personality Disorder (BPD) experience 25 distinct forms of distress that are far more prevalent in BPD than in other conditions.
This interpersonal pain may reinforce a “medical victim” identity, where relational distress becomes central to how individuals with BPD experience and seek relief from pain. [Sansone and Sansone, 2007]
Zanarini et al. highlighted that individuals with Borderline Personality Disorder (BPD) experience 25 distinct forms of distress that are far more prevalent in BPD than in other conditions.
This interpersonal pain may reinforce a “medical victim” identity, where relational distress becomes central to how individuals with BPD experience and seek relief from pain. [Sansone and Sansone, 2007]
This is a little glimpse from the comprehensive review of the Neurobiology and Psychodynamics of BPD.
Full article 👉psychscenehub.com/psychinsights/…
For clinicians, consider the courses (including the psychodynamic psychotherapy courses on the Academy ) 👉academy.psychscene.com
Full article 👉psychscenehub.com/psychinsights/…
For clinicians, consider the courses (including the psychodynamic psychotherapy courses on the Academy ) 👉academy.psychscene.com
• • •
Missing some Tweet in this thread? You can try to
force a refresh