
Psychiatrist blending neuroscience with real-world practice. Insights beyond the textbooks, made actionable. Follow for clear, practical takes.
7 subscribers
How to get URL link on X (Twitter) App


 1/ In cannabinoid hyperemesis syndrome (CHS), patients often report compulsive hot showers or baths that temporarily relieve severe nausea and vomiting.
1/ In cannabinoid hyperemesis syndrome (CHS), patients often report compulsive hot showers or baths that temporarily relieve severe nausea and vomiting.
 1/ Lessons from angina -
1/ Lessons from angina - 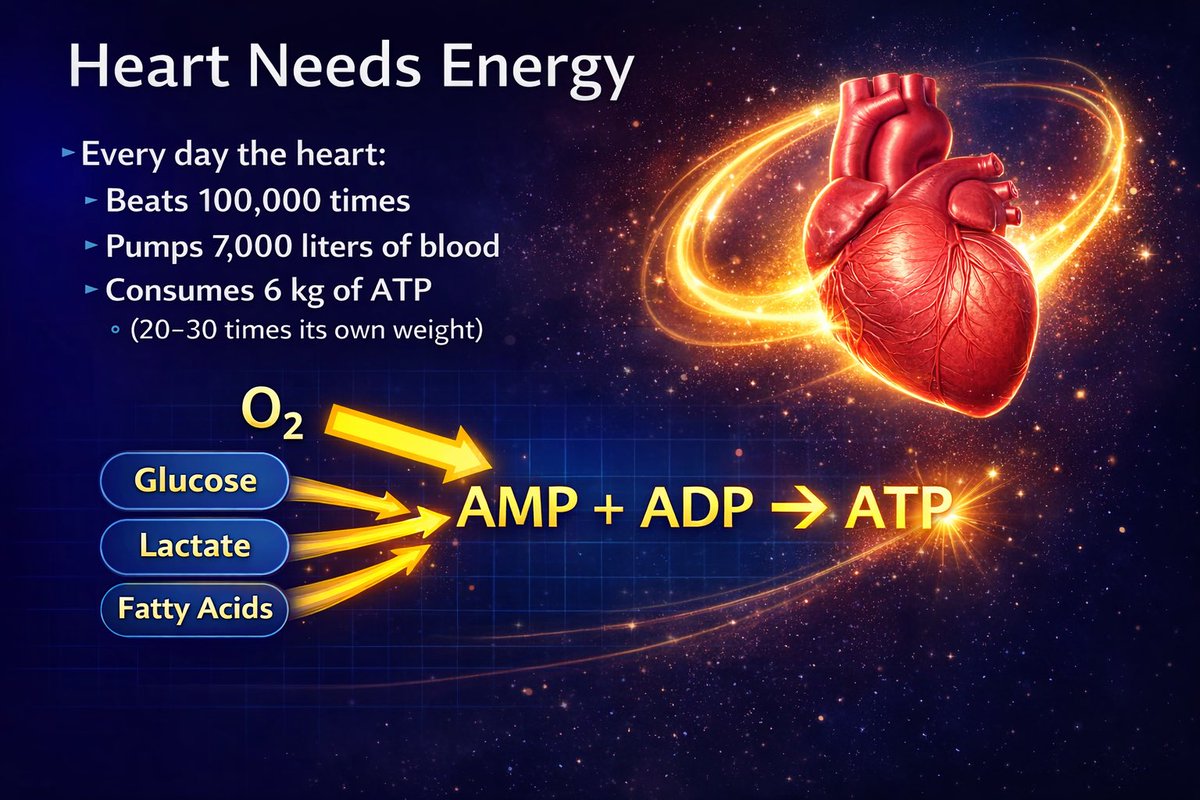
 1/ Receptor selectivity
1/ Receptor selectivity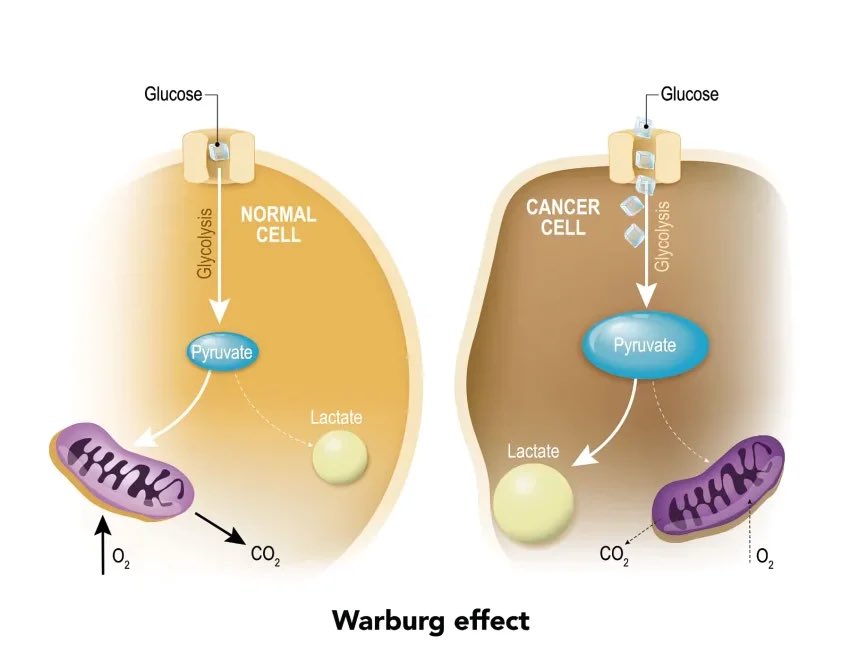
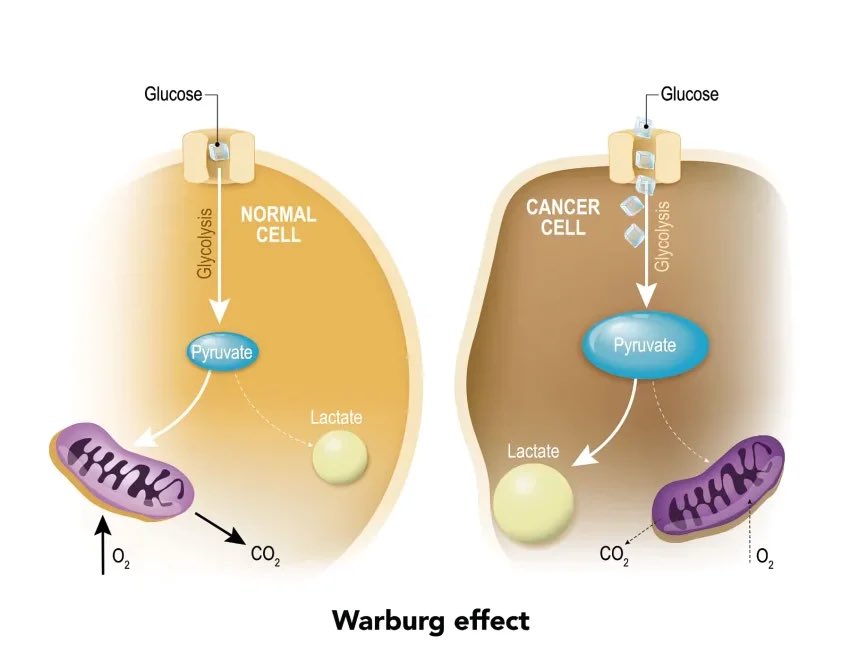 1/ In cancer, one of the earliest changes isn’t a mass or a tumour.
1/ In cancer, one of the earliest changes isn’t a mass or a tumour.
 1/ Prof Michael Berk has just published an important editorial in the British Journal of Psychiatry that articulates something many clinicians feel but rarely name.
1/ Prof Michael Berk has just published an important editorial in the British Journal of Psychiatry that articulates something many clinicians feel but rarely name.

https://twitter.com/stimimi/status/20102470511337597081/ These medications are multifaceted in their mechanisms of action that allow the pharmacologist to target specific domains.

 1/ Sleep problems in ADHD are heterogeneous.
1/ Sleep problems in ADHD are heterogeneous.
https://twitter.com/awaisaftab/status/1991656715901964436
 1️⃣ Treat diagnosis as a process, not an endpoint
1️⃣ Treat diagnosis as a process, not an endpoint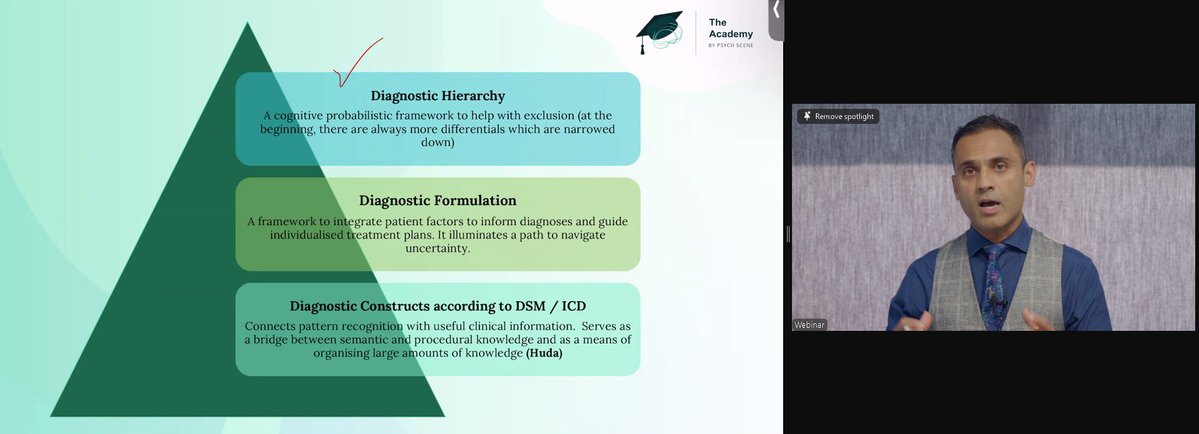

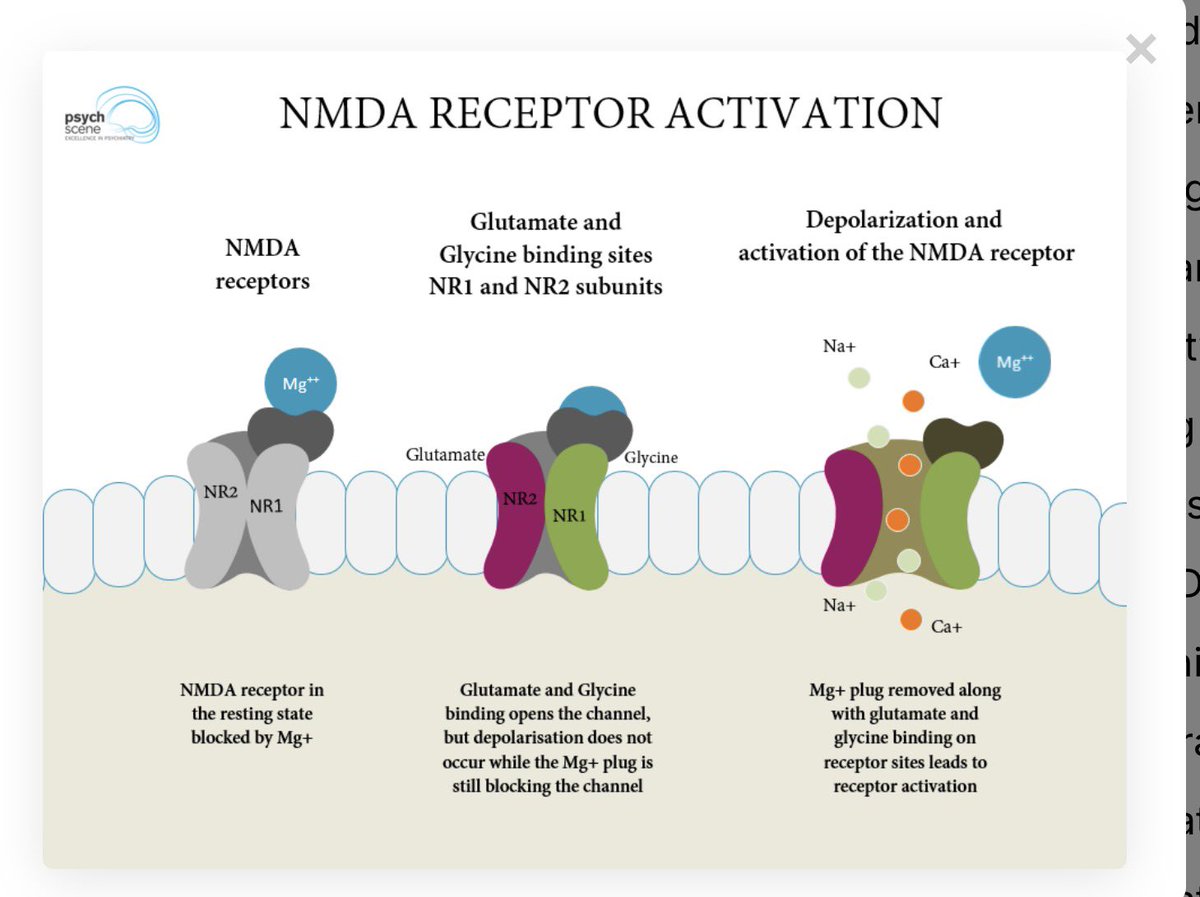
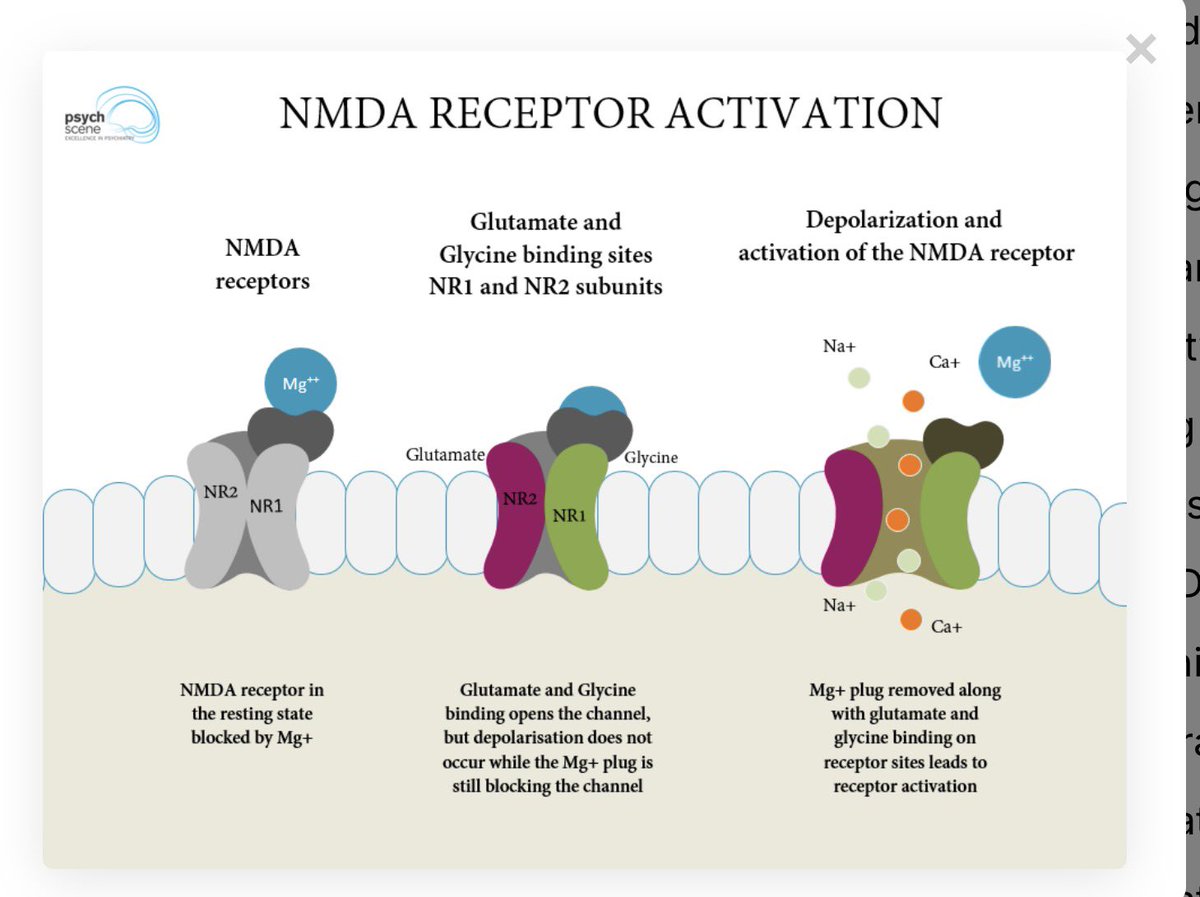
 1/ Psychosis isn’t just about voices or dopamine.
1/ Psychosis isn’t just about voices or dopamine.
 1/At #WCP25 Attended a talk by Prof Tomas Paus and this one theme stood out - the retina.
1/At #WCP25 Attended a talk by Prof Tomas Paus and this one theme stood out - the retina.

 1/ What we often call “ADHD” is a cluster of domains -
1/ What we often call “ADHD” is a cluster of domains - 



 1/ As a psychiatrist who work in addiction psychiatry - Understanding neuroscience is crucial because the brain doesn’t label behaviours as gambling or porn.
1/ As a psychiatrist who work in addiction psychiatry - Understanding neuroscience is crucial because the brain doesn’t label behaviours as gambling or porn.

 1/ Role of D3 receptors #WCP25 #WCP2025
1/ Role of D3 receptors #WCP25 #WCP2025 

 1/ Maxim 1: Define the depression
1/ Maxim 1: Define the depression

 2/ That factor is Depression and exhaustion (DEEX)
2/ That factor is Depression and exhaustion (DEEX) 
 1/ STAR*D is often described as a pragmatic trial.
1/ STAR*D is often described as a pragmatic trial.

 1/ Psychotherapy is essential in BPD.
1/ Psychotherapy is essential in BPD. 
 1/ Depression is frequently reduced to sadness or low mood.
1/ Depression is frequently reduced to sadness or low mood.

 1/ Clonidine is an alpha 2 agonist.
1/ Clonidine is an alpha 2 agonist. 
 1/ Metformin’s relevance in psychiatry goes beyond glucose control.
1/ Metformin’s relevance in psychiatry goes beyond glucose control.
 1/ For over a decade, psychiatry has recognised the metabolic burden of antipsychotics.
1/ For over a decade, psychiatry has recognised the metabolic burden of antipsychotics.