Who will get a Covid booster in 2025? Far fewer than before...
The JCVI decision means that Clinically Vulnerable people u70 and who aren't immunosuppressed lose access.
“Cost-effectiveness” prioritised over protection.
NEW CONCERNING STUDY 👇
1/🧵
The JCVI decision means that Clinically Vulnerable people u70 and who aren't immunosuppressed lose access.
“Cost-effectiveness” prioritised over protection.
NEW CONCERNING STUDY 👇
1/🧵
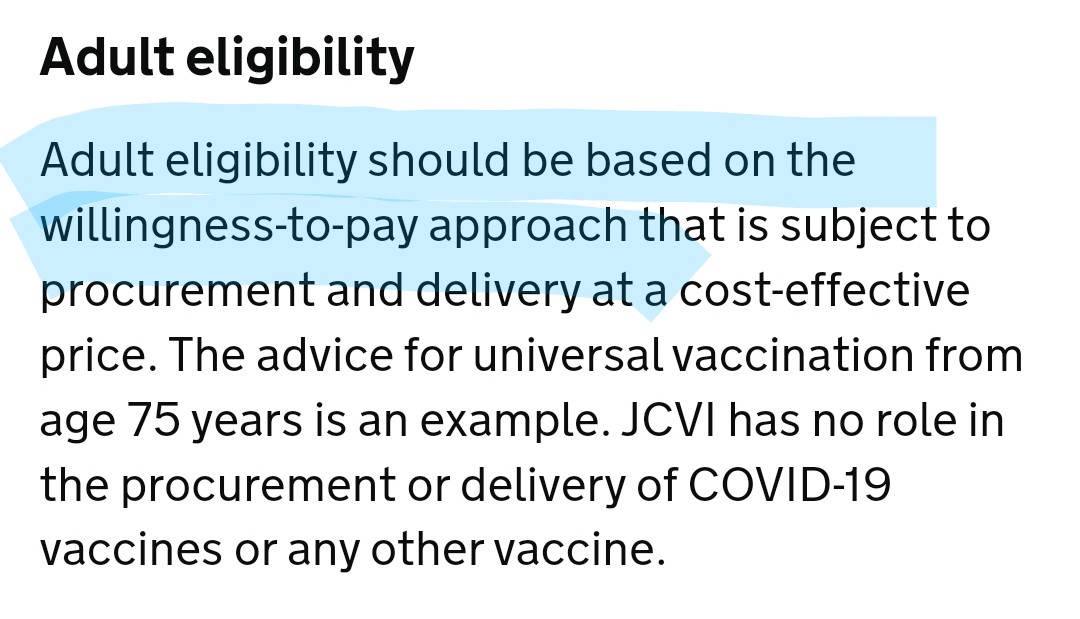
Until now, Covid vaccine policy prioritised protecting 'at risk' groups.
Their approach focuses on “cost-effectiveness,” raising age thresholds. Not providing vaccine protection to younger Clinically Vulnerable. It’s a deeply worrying change.
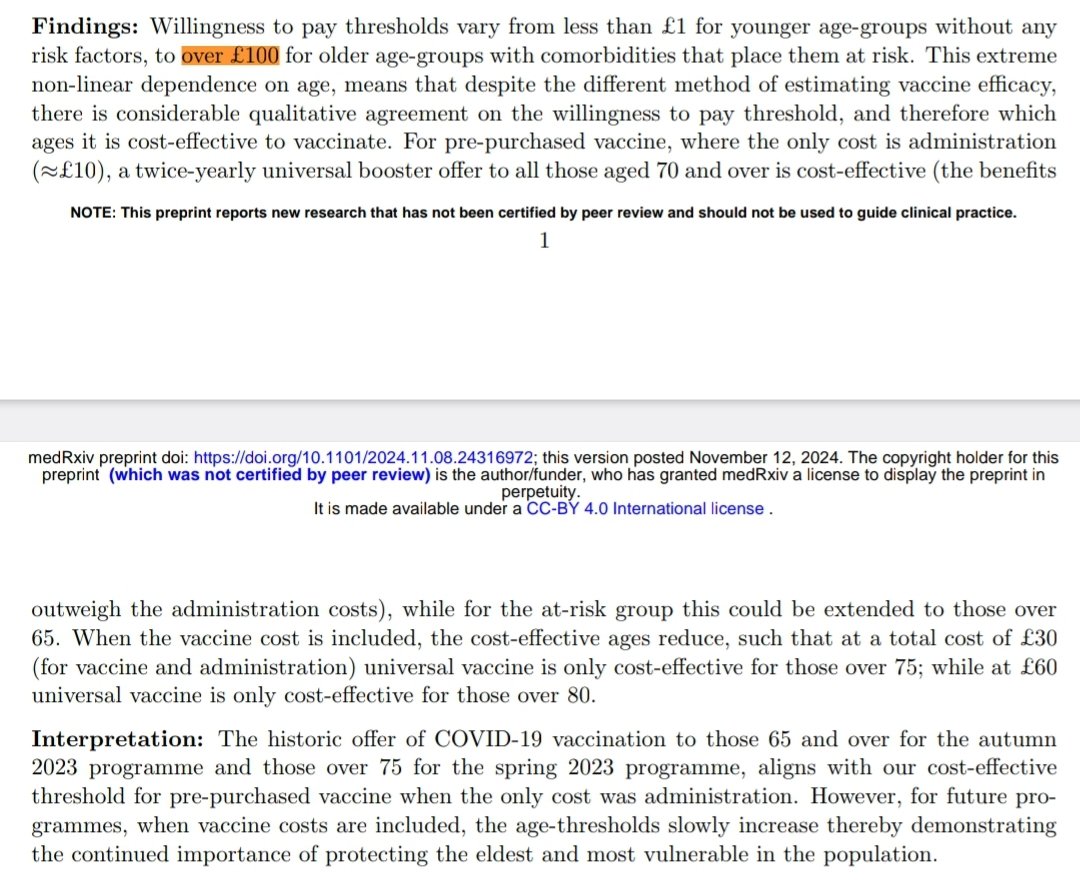
This data may have been used.
2/
Their approach focuses on “cost-effectiveness,” raising age thresholds. Not providing vaccine protection to younger Clinically Vulnerable. It’s a deeply worrying change.
This data may have been used.
2/

Younger Clinically Vulnerable people e.g. those with chronic heart failure, COPD, or diabetes could be excluded.
The study admits data for our group is limited, meaning the most at-risk could fall through the cracks.
*It is unclear if the study was used in decision-making.*
3/
The study admits data for our group is limited, meaning the most at-risk could fall through the cracks.
*It is unclear if the study was used in decision-making.*
3/

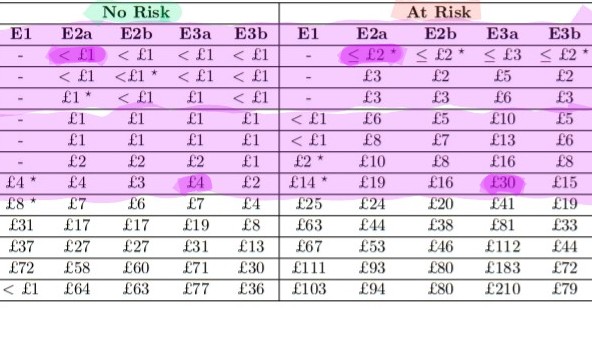
The disparity is clear:
The willingness to pay for Covid boosters varies from under £1-£4 for healthy people under 70, but between £2-£30 for vulnerable people in the same age group.
Worse, this approach ignores the economic disparities within the at-risk group itself.
4/
The willingness to pay for Covid boosters varies from under £1-£4 for healthy people under 70, but between £2-£30 for vulnerable people in the same age group.
Worse, this approach ignores the economic disparities within the at-risk group itself.
4/
Shifting vaccine decisions to economic models, which consider the ability and willingness to pay, rather than public health goals will deepen existing health inequalities for Clinically Vulnerable groups.
5/
5/
Vaccines reduce transmission, protect the NHS, protect health and save lives.
Narrow economic criteria ignoring these benefits, risk putting everyone at greater risk.
6/
Narrow economic criteria ignoring these benefits, risk putting everyone at greater risk.
6/
The focus on age-based thresholds ignores the reality for younger vulnerable groups.
So 30-year-old in heart failure could face far higher risks than a healthy 70-year-old, yet this new policy would exclude them from protection.
7/


So 30-year-old in heart failure could face far higher risks than a healthy 70-year-old, yet this new policy would exclude them from protection.
7/
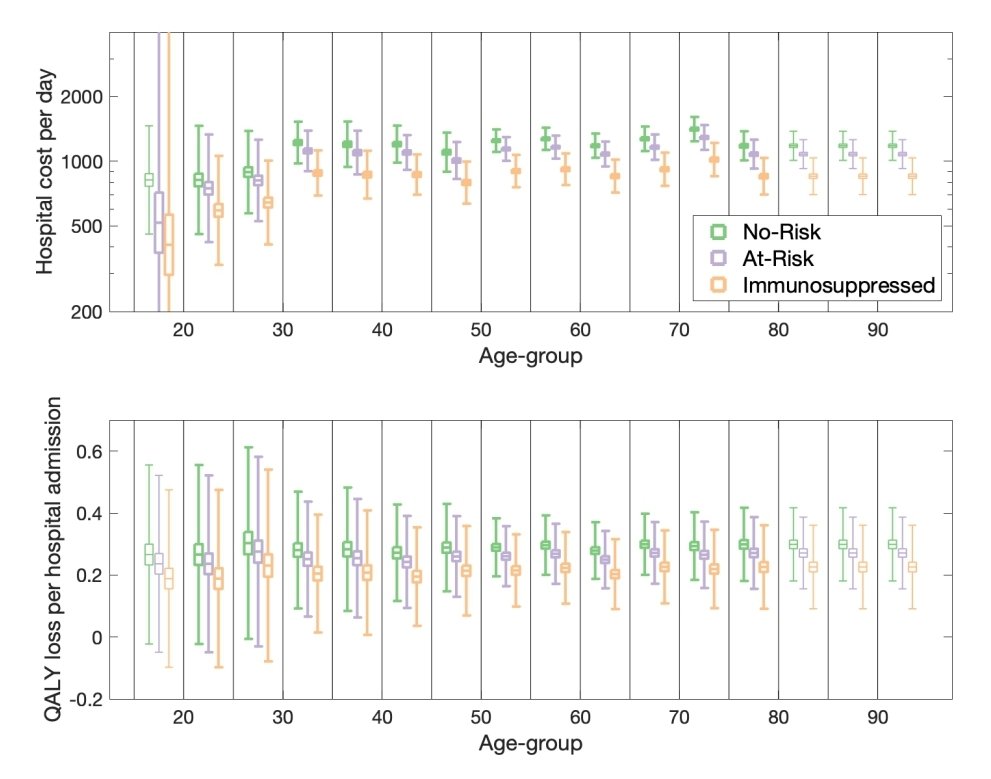
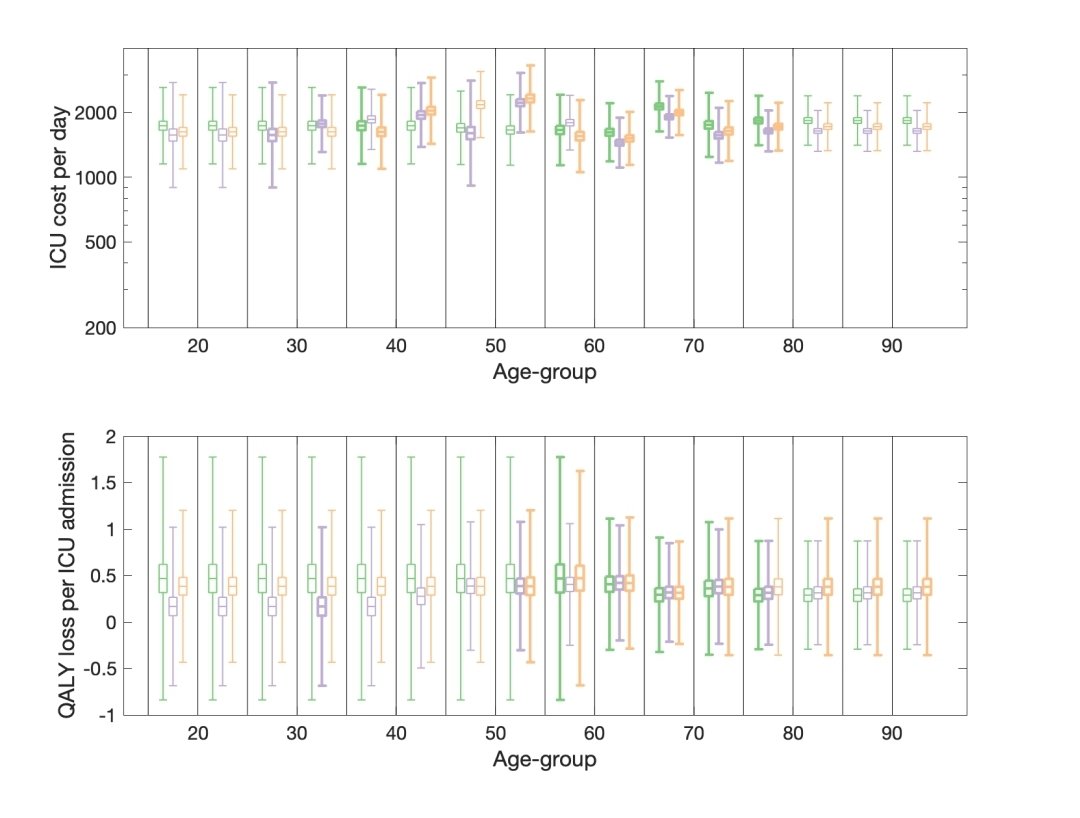
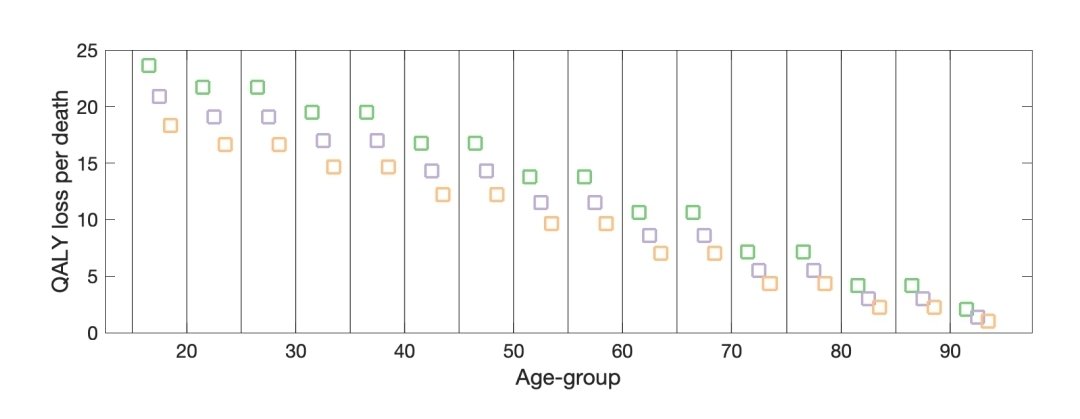
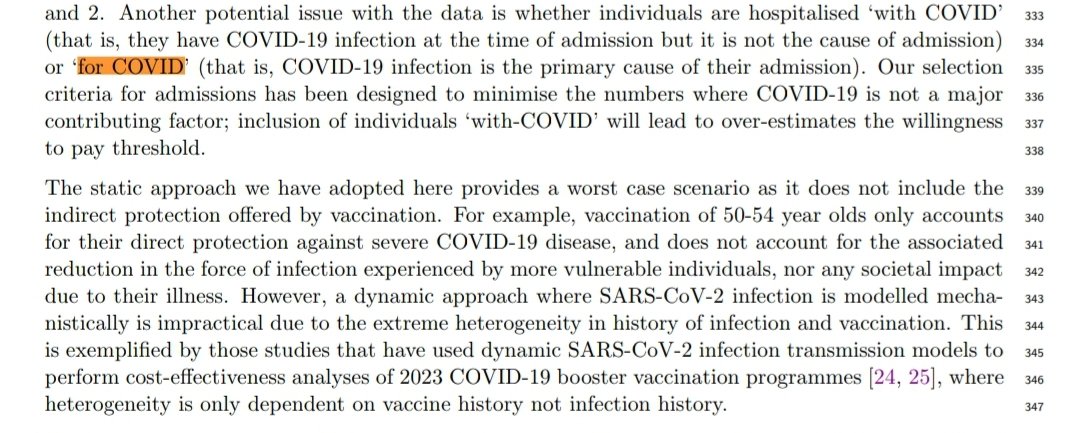
Data gaps may also make this worse. The study struggles to distinguish between hospitalisations “for COVID” and “with COVID.”
It dilutes the data for Clinically Vulnerable people and leads to an over estimation of willingness, making it harder to justify protections we need.
8/
It dilutes the data for Clinically Vulnerable people and leads to an over estimation of willingness, making it harder to justify protections we need.
8/
New variants are unpredictable.
A variant with higher severity or greater immune escape would hit vulnerable groups like us hardest.
The policy assumes risks will stay static - but we know from experience how quickly things can change...
9/
A variant with higher severity or greater immune escape would hit vulnerable groups like us hardest.
The policy assumes risks will stay static - but we know from experience how quickly things can change...
9/
This shift also ignores public health equity. Prioritising “cost-effectiveness” over vulnerability sends a chilling message:
That our lives are less valuable because protecting us isn’t deemed “efficient.”
10/
That our lives are less valuable because protecting us isn’t deemed “efficient.”
10/
Public involvement is mentioned in the study - only *after* models were developed. Involving Clinically Vulnerable groups from the outset would create policies that reflect real needs and risks.
There is an urgent need for direct inclusion in "Equality Impact Assessments".
11/
There is an urgent need for direct inclusion in "Equality Impact Assessments".
11/
Policymakers must:
1. Reverse this dangerous shift towards economic thresholds.
2. Collect better data on Clinically Vulnerable groups.
3. Centre equity and vulnerability in vaccine decisions, not just cost.
12/
1. Reverse this dangerous shift towards economic thresholds.
2. Collect better data on Clinically Vulnerable groups.
3. Centre equity and vulnerability in vaccine decisions, not just cost.
12/
Denying vaccines to the Clinically Vulnerable, based on what may well be flawed data and economic models, is not just bad policy - it is morally wrong.
We need protection, inclusion, and fairness!
13/
We need protection, inclusion, and fairness!
13/
The full study is available here:
"Cost-effectiveness of routine COVID-19 adult vaccination programmes in England"
14/
medrxiv.org/content/10.110…
"Cost-effectiveness of routine COVID-19 adult vaccination programmes in England"
14/
medrxiv.org/content/10.110…
We are deeply concerned about the impact of these changes on Clinically Vulnerable people.
If you share our concerns, please contact your MP and ask them to ensure equitable access to Covid vaccines for all who need them. 🙏
16/
parliament.uk/get-involved/c…
If you share our concerns, please contact your MP and ask them to ensure equitable access to Covid vaccines for all who need them. 🙏
16/
parliament.uk/get-involved/c…
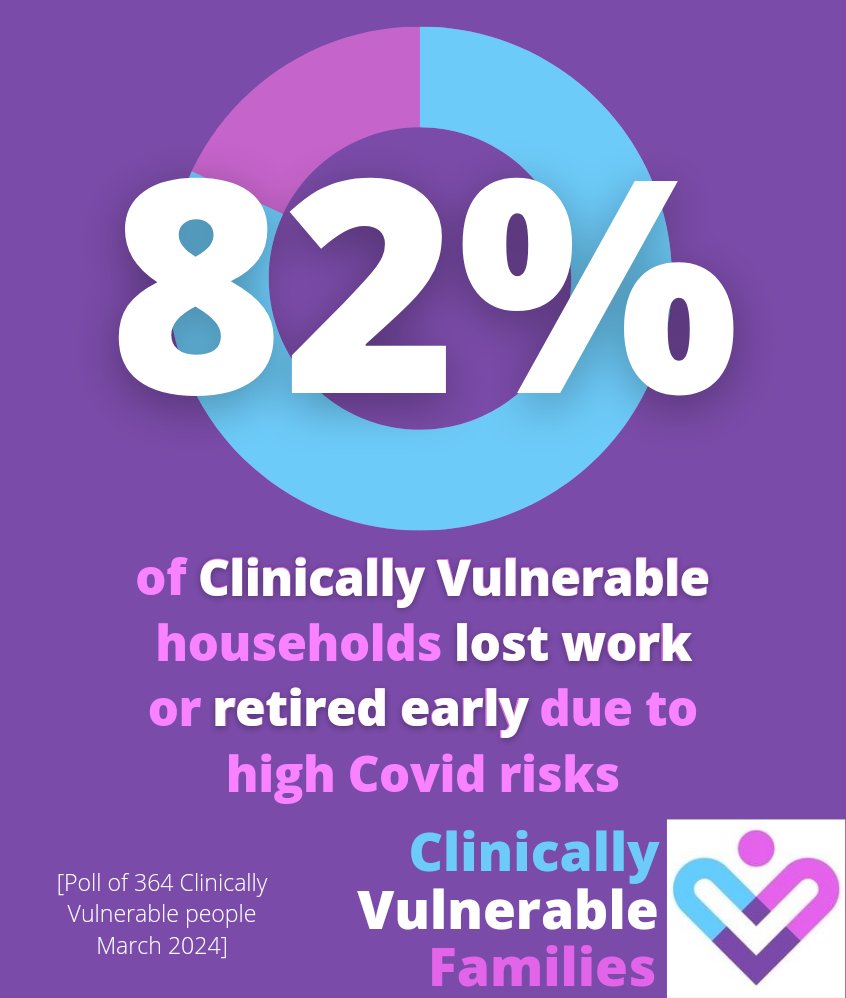
@_CatintheHat Huge proportions of Clinically Vulnerable households have lost work or retired early due to high Covid risks. 
• • •
Missing some Tweet in this thread? You can try to
force a refresh




![82% of Clinically Vulnerable households lost work or retired early due to high Covid risks [Poll of 364 Clinically Vulnerable people March 2024] Clinically Vulnerable Families](https://pbs.twimg.com/media/GbEcF7CbQAA08ir.jpg)



