Here's a reminder of my take on #COVID-19 (the disease not the pandemic).
It's not what you think it is ...
A thread 👇
1/23
It's not what you think it is ...
A thread 👇
1/23

The acute phase of #COVID was and is misunderstood by the majority of doctors.
The lung disease (the thing that many died of) was not a pneumonia.
Yes, it was a lung disease caused by a virus, but this is where the similarity with other viruses which cause pneumonias ends.
2/23
The lung disease (the thing that many died of) was not a pneumonia.
Yes, it was a lung disease caused by a virus, but this is where the similarity with other viruses which cause pneumonias ends.
2/23
Influenza causes inflammation in the lung airways. #COVID did not do this.
The lung disease we saw in the acute phase of COVID was a vascular disease. It caused inflammation, clotting, and congestion in the smallest blood vessels of the lungs.
3/23
The lung disease we saw in the acute phase of COVID was a vascular disease. It caused inflammation, clotting, and congestion in the smallest blood vessels of the lungs.
3/23
I'm talking about the lung disease in the past tense, because it is a thing of the past. We don't see it anymore.
This is not because of vaccinations, it is because the virus evolved. Delta and earlier variants caused the severe lung disease. Omicron variants do not.
4/23
This is not because of vaccinations, it is because the virus evolved. Delta and earlier variants caused the severe lung disease. Omicron variants do not.
4/23
The ACE2 receptor is found on the inner surface of our blood vessels. This is the protein receptor which the #SARS-CoV-2 virus binds to. This receptor is not found in the airways of the lungs.
The distribution of lung damage we saw is also important to understand.
5/23
The distribution of lung damage we saw is also important to understand.
5/23
It is a distinct pattern which damages the bottom, back and edges of the lungs, symmetrically.
These are the parts of the lungs which are most richly supplied with blood. They are also the parts of the lungs furthest away from the central airways.
6/23
These are the parts of the lungs which are most richly supplied with blood. They are also the parts of the lungs furthest away from the central airways.
6/23
This leads to the possibility that the #SARS virus can travel around the body in the blood, including to the lungs, from the upper respiratory tract - the nose & mouth.
This helps explain why those with gum disease are at massively increased risk of death (x14).
#LeakyGums
7/23
This helps explain why those with gum disease are at massively increased risk of death (x14).
#LeakyGums
7/23
It also explains why people with high levels of the #SARS2 virus in saliva are the most likely to die.
And it explains why introducing simple oral hygiene measures stopped people going into intensive care and dying at the height of the pandemic.
8/23
And it explains why introducing simple oral hygiene measures stopped people going into intensive care and dying at the height of the pandemic.
8/23
Understanding the acute phase of the disease is also crucial for understanding the later phase of #COVID, referred to as post-acute or #longCOVID. Sometimes these terms are used interchangeably, which is not necessarily correct.
9/23
9/23
Those who survived the severe acute disease may have a long period of recovery. Others get symptoms following infection which persist and are not dependent on the severity of the initial acute phase infection.
10/23
10/23
To understand these long-lasting phenomena we need to first understand that acute #COVID was never a pneumonia. Not only is COVID-19 not JUST a pneumonia, it was never a pneumonia at all.
11/23
11/23
Medical images show us that the severe lung disease of #COVID-19 is the opposite of influenza - it occupies a different anatomical compartment in the lungs.
All of this means there is no reason to expect that the later phases of COVID-19 should be anything like influenza.
12/23
All of this means there is no reason to expect that the later phases of COVID-19 should be anything like influenza.
12/23
It is also important to understand that all #SARS2 variants can cause #longCOVID, regardless of whether people had the lung disease.
What we need to understand is that the acute lung disease provides a big clue about long COVID.
13/23
What we need to understand is that the acute lung disease provides a big clue about long COVID.
13/23
It tells us that all phases of #COVID are related to damage to the endothelium (the cells which line the inner surface of blood vessels) not just in the lungs but all over the body.
Similar damage is seen in acute #COVID and #longCOVID.
14/23
Similar damage is seen in acute #COVID and #longCOVID.
14/23
Identical medical scan appearances are found in the lungs of >85% of people who have breathing problems months after hospital admission as those seen in the acute phase. The same lung disease of clotting and congestion of lung blood vessels persists in these patients.
15/23
15/23
We know #SARS2 spreads via the blood because it is found in many body organs months after infection.
Blood tests also show persistent microscopic clots in the blood of people with #longCOVID. These clots are different from normal blood clots because they don't break down.
16/23
Blood tests also show persistent microscopic clots in the blood of people with #longCOVID. These clots are different from normal blood clots because they don't break down.
16/23
Understanding the anatomical pathway the #SARS2 virus takes through the body is crucial, both in the acute phase and later phases of #COVID.
Which brings us back to the mouth.
17/23
Which brings us back to the mouth.
17/23
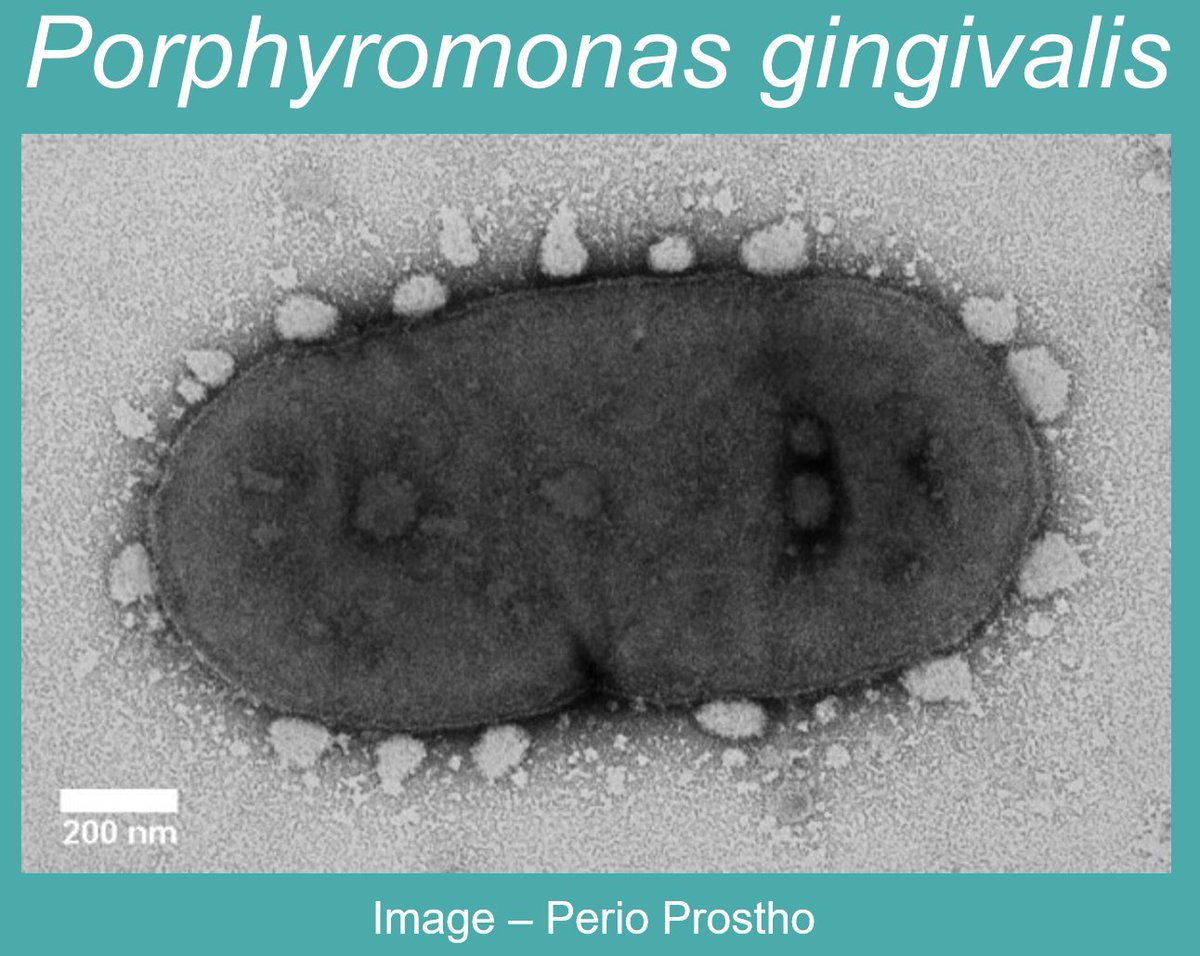
The mouth is a viral factory in the acute phase of the disease. As well as gum disease, changes in the oral microbiome predict severity of acute #COVID.
(The oral microbiome is the spectrum of microorganism species, mainly bacteria, which live in our mouths.)
18/23
(The oral microbiome is the spectrum of microorganism species, mainly bacteria, which live in our mouths.)
18/23
Long COVID, and similar diseases like #MECFS, can be predicted by harmful changes to the oral microbiome. (This is known as oral dysbiosis.)
#OralDysbiosis
19/22
#OralDysbiosis
19/22
Oral dysbiosis is also directly linked to the development of multiple important diseases of the body including cardiovascular disease, diabetes, Alzheimer's, rheumatoid arthritis, inflammatory bowel disease, pregnancy complications, and cancers.
20/23
20/23
This is now my major area of interest.
Put simply, we need to rewrite medicine.
The mouth is not just a cake hole!
Good oral health is vital to body health, not as an add-on extra but as an upstream mechanistic determinant of body health.
21/23
Put simply, we need to rewrite medicine.
The mouth is not just a cake hole!
Good oral health is vital to body health, not as an add-on extra but as an upstream mechanistic determinant of body health.
21/23
What this line of thinking about #COVID has taught me is that the mouth is a lot more important for our overall body health than we previously thought possible.
I don't think there are simple answers but I would encourage you, whoever you are, to look after your mouth.
22/23
I don't think there are simple answers but I would encourage you, whoever you are, to look after your mouth.
22/23
This doesn't only mean good personal oral hygiene or going to the dentist. It means not smoking/vaping. It means not putting foods you are not designed to eat in your mouth. And it means stopping consuming foods/drinks with added sugar or other forms of UPF junk.
23/23
23/23
• • •
Missing some Tweet in this thread? You can try to
force a refresh