COVID INQUIRY: X Megathread 🧵
As module 3 of the @covidinquiryuk draws to a close, I’ve been looking back at what we’ve learned about how it all went so wrong with infection control guidance for hospitals.
This is a long thread, so please grab a cuppa & make yourself comfy…
As module 3 of the @covidinquiryuk draws to a close, I’ve been looking back at what we’ve learned about how it all went so wrong with infection control guidance for hospitals.
This is a long thread, so please grab a cuppa & make yourself comfy…

One thing that really stands out from the Inquiry testimonies is just how many professional bodies repeatedly raised the alarm about the inadequate infection control guidance in hospitals…
…and how their concerns were disregarded at every stage, with profound consequences.
…and how their concerns were disregarded at every stage, with profound consequences.
The lady taking the stand in the clip above is Rosemary Gallagher, IPC Lead at the Royal College of Nursing.
She explains how, in November 2020, the government had just released a video to the public highlighting how coronavirus lingers in the air…
gov.uk/government/new…
She explains how, in November 2020, the government had just released a video to the public highlighting how coronavirus lingers in the air…
gov.uk/government/new…

Below is the government video Rosemary is referring to (released Nov 2020).
It couldn’t be clearer:
“Coronavirus is spread through the air via large droplets & smaller particles.
Lighter coronavirus particles float in the air. They can linger in a room or any enclosed space.”
It couldn’t be clearer:
“Coronavirus is spread through the air via large droplets & smaller particles.
Lighter coronavirus particles float in the air. They can linger in a room or any enclosed space.”
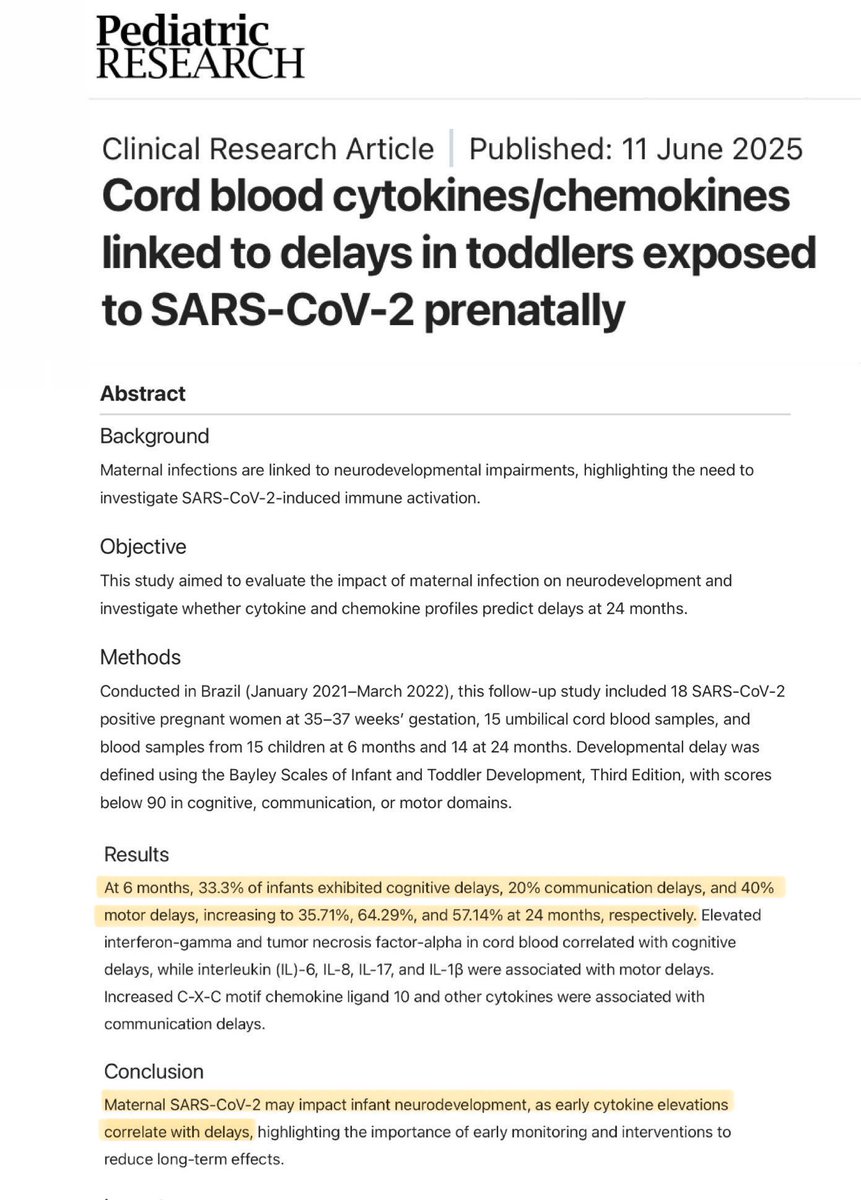
However, NHS staff were being given a very DIFFERENT message at that time.
They were told that Covid was ONLY transmitted via DROPLETS & CONTACT - except during certain procedures which had been designated as aerosol generating procedures (AGPs).
madeinheene.hee.nhs.uk/Portals/0/COVI…
They were told that Covid was ONLY transmitted via DROPLETS & CONTACT - except during certain procedures which had been designated as aerosol generating procedures (AGPs).
madeinheene.hee.nhs.uk/Portals/0/COVI…
In fact, as early as March 2020, Prof Stephen Powis (National Medical Director of NHS England) had sent a letter to the Chief Execs of all NHS Trusts stating:
“Covid-19 is not airborne, it is droplet carried.”
Given the uncertainty at the time, this seems quite remarkable.
“Covid-19 is not airborne, it is droplet carried.”
Given the uncertainty at the time, this seems quite remarkable.
Meanwhile, in the US, President Trump revealed that China had come out with a report and statement very early on that Covid was an airborne disease.
He claims he knew it was airborne from the start.
In fact, he says that “everyone knew it was airborne”.
He claims he knew it was airborne from the start.
In fact, he says that “everyone knew it was airborne”.
Prof @CliveBeggs is an expert witness to the Inquiry, specialising in disease transmission.
In this clip, he discusses why it was initially assumed in the UK that Covid WASN’T airborne…
…and why this was so crucially important in terms of the infection control (IPC) measures.
In this clip, he discusses why it was initially assumed in the UK that Covid WASN’T airborne…
…and why this was so crucially important in terms of the infection control (IPC) measures.
Since Covid was designated as DROPLET spread, the guidance only required surgical masks to be worn (except during AGPs).
If it had been designated as AIRBORNE, FFP3 masks would have been advised (since surgical masks do NOT protect against aerosols).
journalofhospitalinfection.com/article/S0195-…
If it had been designated as AIRBORNE, FFP3 masks would have been advised (since surgical masks do NOT protect against aerosols).
journalofhospitalinfection.com/article/S0195-…

The paper mentioned above was co-authored by Dr Lisa Ritchie, who chaired the IPC Cell (the group responsible for writing IPC guidance).
In the paper, it also mentioned that SARS-CoV-1 was airborne & healthcare workers should wear FFP3 masks when treating SARS-CoV-1 patients...
In the paper, it also mentioned that SARS-CoV-1 was airborne & healthcare workers should wear FFP3 masks when treating SARS-CoV-1 patients...
The odd thing about this is that SARS-CoV-1 was considered the closest ‘relative’ to SARS-CoV-2 (Covid) and was supposed to have guided the initial Covid IPC guidance.
However, SARS-CoV-1 had been treated with AIRBORNE precautions, but Covid was treated with DROPLET precautions.
However, SARS-CoV-1 had been treated with AIRBORNE precautions, but Covid was treated with DROPLET precautions.
Prof Colin McKay (Deputy Director for NHS Greater Glasgow & Clyde) testified that, as early as April 2020, it was increasingly clear to those on the ground that airborne transmission WAS taking place…
…and that infection control advice was INCORRECT, leaving staff unprotected.
…and that infection control advice was INCORRECT, leaving staff unprotected.
Matt Hancock (ex-Health Secretary) testified that he was well aware that, at times, healthcare workers treated Covid patients with inadequate PPE, thereby putting themselves at potential risk…
…and he also knew that FFP3 masks were more protective than FRSM (surgical) masks.
…and he also knew that FFP3 masks were more protective than FRSM (surgical) masks.
We also heard from IPC expert, Dr Ben Warne, that the list of AGPs was a red herring since simply coughing produces as many aerosols as the designated aerosol generating procedures (AGPs).
…and 2 in 3 people who come to hospital with Covid present with coughing.
…and 2 in 3 people who come to hospital with Covid present with coughing.
This was also borne out by the data…
Anaesthetists & intensive care doctors working in the HIGHEST risk areas where AGPs were being performed (who were wearing FFP3 masks) ended up being at LOWER risk than staff on general wards in terms of Covid infection & mortality rates.
Anaesthetists & intensive care doctors working in the HIGHEST risk areas where AGPs were being performed (who were wearing FFP3 masks) ended up being at LOWER risk than staff on general wards in terms of Covid infection & mortality rates.
Baroness Hallett has asked multiple witnesses the million-dollar question about why a precautionary approach was not adopted:
“If you don’t know the route of transmission, surely you should be preparing for & guarding against EVERY possible route of transmission until you know?”
“If you don’t know the route of transmission, surely you should be preparing for & guarding against EVERY possible route of transmission until you know?”
It seems there was one big issue preventing them from being able to adopt a precautionary approach.
Quite simply, there wasn’t enough PPE.
In this clip, Matt Hancock (ex-Health Secretary) explains how availability of PPE had been taken into account when drafting IPC guidance.
Quite simply, there wasn’t enough PPE.
In this clip, Matt Hancock (ex-Health Secretary) explains how availability of PPE had been taken into account when drafting IPC guidance.
A similar story was given by Laura Imrie, a member of the IPC Cell (the group responsible for writing the guidance).
She explained how lack of supply & the need for fit testing meant they weren’t in a position to be able to recommend wider use of FFP3 masks in the guidance.
She explained how lack of supply & the need for fit testing meant they weren’t in a position to be able to recommend wider use of FFP3 masks in the guidance.
The considerations around PPE supply were also apparent from the minutes of the IPC Cell (Dec 2020).
Some members were in favour of a move to advising wider use of FFP3 masks.
But others commented:
“If we increase the use of FFP3 masks, we need to consider stock availability”.
Some members were in favour of a move to advising wider use of FFP3 masks.
But others commented:
“If we increase the use of FFP3 masks, we need to consider stock availability”.

However, we heard a very different story from Dr Lisa Ritchie, who chaired the IPC Cell.
She wrote in her witness statement:
“The supply of PPE did *not* influence the IPC advice provided by the UK IPC Cell.”
It seems someone is perhaps not being completely truthful here.
She wrote in her witness statement:
“The supply of PPE did *not* influence the IPC advice provided by the UK IPC Cell.”
It seems someone is perhaps not being completely truthful here.
The PPE supply issues did not last forever.
Dr Barry Jones (Chair of CATA) testified that, by Autumn 2020, there were sufficient FFP3 masks in stock.
This would have been the perfect opportunity to CHANGE the IPC guidance to ensure healthcare workers were adequately protected.
Dr Barry Jones (Chair of CATA) testified that, by Autumn 2020, there were sufficient FFP3 masks in stock.
This would have been the perfect opportunity to CHANGE the IPC guidance to ensure healthcare workers were adequately protected.
Meanwhile, evidence was mounting about the likelihood that Covid was airborne.
Prof Chris Whitty (CMO) was asked when he realised that Covid was airborne.
He replied:
“…the midpoint of medical & scientific opinion undoubtedly shifted over the course of the FIRST YEAR.”
Prof Chris Whitty (CMO) was asked when he realised that Covid was airborne.
He replied:
“…the midpoint of medical & scientific opinion undoubtedly shifted over the course of the FIRST YEAR.”
In Sept 2020, SAGE produced an important paper titled “Role of Ventilation in Controlling SARS-CoV-2 Transmission”.
This paper discussed ventilation as a way of mitigating airborne spread of Covid, effectively confirming that Covid was indeed AIRBORNE.
assets.publishing.service.gov.uk/media/5f917153…
This paper discussed ventilation as a way of mitigating airborne spread of Covid, effectively confirming that Covid was indeed AIRBORNE.
assets.publishing.service.gov.uk/media/5f917153…
Prof Beggs’ witness statement reinforces this view, stating that:
“By end of Sept 2020, there was enough moderate certainty evidence to strongly suggest that SARS-CoV-2 could be transmitted via the airborne route”.
Pressure began to mount on the IPC Cell to change the guidance.
“By end of Sept 2020, there was enough moderate certainty evidence to strongly suggest that SARS-CoV-2 could be transmitted via the airborne route”.
Pressure began to mount on the IPC Cell to change the guidance.
NHS staff were becoming increasingly aware of the flaws in the IPC guidance - and how they were NOT being adequately protected.
As Rosemary Gallagher from the Royal College of Nurses explains:
“If Covid was in fact airborne, then that had implications for the IPC guidance…”
As Rosemary Gallagher from the Royal College of Nurses explains:
“If Covid was in fact airborne, then that had implications for the IPC guidance…”
In this clip, Prof Banfield (Chair of the BMA Council) states:
“I can say that, overwhelmingly, the majority of people (healthcare workers) felt let down at the time, & STILL feel let down, by the observation that surgical masks are not protective against airborne infections.”
“I can say that, overwhelmingly, the majority of people (healthcare workers) felt let down at the time, & STILL feel let down, by the observation that surgical masks are not protective against airborne infections.”
In Dec 2020, shortly after the Public Health video about airborne transmission was released & under mounting pressure, the IPC Cell convened to review their decision on FFP3 masks in hospitals.
However, they ultimately decided NOT to change the guidance.
assets.publishing.service.gov.uk/media/60803e55…
However, they ultimately decided NOT to change the guidance.
assets.publishing.service.gov.uk/media/60803e55…

During this meeting on 22 Dec 2020, we now know that the decision was NOT unanimous…
A representative from Public Health England is on record as stating:
“Our understanding of aerosol transmission has changed. A precautionary approach to move to FFP3 masks should be advised.”
A representative from Public Health England is on record as stating:
“Our understanding of aerosol transmission has changed. A precautionary approach to move to FFP3 masks should be advised.”
The IPC Cell supposedly drafted the guidance based on ‘consensus’ of cell members - however, as shown above, this consensus was NOT unanimous.
We also discovered that no formal votes were ever taken & it was ultimately up to the Chair (Ritchie) to decide the consensus position.
We also discovered that no formal votes were ever taken & it was ultimately up to the Chair (Ritchie) to decide the consensus position.
Baroness Hallett challenged Lisa Ritchie about the fact that the IPC Cell appeared to have “become wedded to the idea that it was droplet”.
Lisa Ritchie replied that, if they’d been advised that there was a potential for airborne transmission, they’d have changed the guidance.
Lisa Ritchie replied that, if they’d been advised that there was a potential for airborne transmission, they’d have changed the guidance.
Please don’t stop reading here… there’s still more to the story.
Click “Show replies” to see rest of the thread.
⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️
Click “Show replies” to see rest of the thread.
⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️
Despite Ritchie’s assurances that they’d change the guidance if told Covid was airborne, guidance remained unchanged.
In the IPC Cell minutes, someone raised concerns that “it would be easy to give the impression that we got it WRONG the first time” if they changed the guidance.
In the IPC Cell minutes, someone raised concerns that “it would be easy to give the impression that we got it WRONG the first time” if they changed the guidance.
In January 2021, the Chief Executive of the RCN (Dame Donna Kinnair) & Chair of the BMA (Dr Chaand Nagpaul) wrote to HSE’s Chief Exec highlighting serious concerns about the risk of airborne infection and the inadequate protection for healthcare workers.
covid19.public-inquiry.uk/wp-content/upl…
covid19.public-inquiry.uk/wp-content/upl…

In particular, they requested an URGENT review of two things:
1. IPC guidance for healthcare, particularly in respect to aerosol and airborne transmission (including an assessment of appropriate PPE).
2. Guidance & provision of ventilation across the healthcare estate.
1. IPC guidance for healthcare, particularly in respect to aerosol and airborne transmission (including an assessment of appropriate PPE).
2. Guidance & provision of ventilation across the healthcare estate.

At the same time, an alliance of other professional bodies & trade unions had sent a letter to Health Secretary Matt Hancock urging him to intervene to ensure that all healthcare professionals have access to FFP3 masks when working with Covid patients.
rcslt.org/wp-content/upl…
rcslt.org/wp-content/upl…

In Jan 2021, the IPC Cell held a ‘Huddle’ meeting to discuss the mounting pressures.
The minutes of the Huddle included the following:
“…there was a document published advising that Covid could be transmitted via the airborne route… This has been removed from the guidance.”
The minutes of the Huddle included the following:
“…there was a document published advising that Covid could be transmitted via the airborne route… This has been removed from the guidance.”

In Feb 2021, 20 organisations representing healthcare workers and patients across the UK joined forces to write to the Prime Minister (Boris Johnson).
They all shared the same concern about the inadequate IPC guidance for healthcare workers.
rcn.org.uk/-/media/Royal-…
They all shared the same concern about the inadequate IPC guidance for healthcare workers.
rcn.org.uk/-/media/Royal-…

Meanwhile, the RCN commissioned an Independent Review of the UK IPC Guidance.
As Rosemary Gallagher (IPC Lead at RCN) explains in her statement:
“This was not a measure I would have expected the RCN ever to have to take, but the organisation felt forced into a corner...”
As Rosemary Gallagher (IPC Lead at RCN) explains in her statement:
“This was not a measure I would have expected the RCN ever to have to take, but the organisation felt forced into a corner...”

The RCN Independent Review concluded that:
“the Rapid Review methodology undertaken (...) does NOT meet contemporary standards for the conduct of rapid reviews & consequently the UK IPC guidelines that draw on it have not been appropriately updated.”
rcn.org.uk/-/media/Royal-…
“the Rapid Review methodology undertaken (...) does NOT meet contemporary standards for the conduct of rapid reviews & consequently the UK IPC guidelines that draw on it have not been appropriately updated.”
rcn.org.uk/-/media/Royal-…

Further letters were sent to the CMOs of the four nations, plus leaders at DHSC & Healthwatch England.
But all to no avail.
At each stage, concerns raised by the professional organisations representing the interests of healthcare workers and patients were dismissed or ignored.
But all to no avail.
At each stage, concerns raised by the professional organisations representing the interests of healthcare workers and patients were dismissed or ignored.

Dr @barryjmjones chaired the alliance of medical organisations, royal colleges & trade unions formed to jointly raise their concerns over the inadequate IPC guidance in healthcare settings.
He testified that the alliance (CATA) were repeatedly “managed out of raising concerns”.
He testified that the alliance (CATA) were repeatedly “managed out of raising concerns”.
@barryjmjones This is in stark contrast to testimony from IPC Cell members who claim that IPC guidance was created in consultation with many groups, including doctor & nurse IPC networks.
Here’s a clip from Laura Imrie (IPC Cell member) suggesting it was always “a two-way conversation”.
Here’s a clip from Laura Imrie (IPC Cell member) suggesting it was always “a two-way conversation”.
Three months after the RCN & other organisations had sent their letter to the Prime Minister, they finally received a response on 7 May 2021.
Once again, their concerns were dismissed.
In desperation, the alliance went public with their concerns, issuing a press release…
Once again, their concerns were dismissed.
In desperation, the alliance went public with their concerns, issuing a press release…
Here’s the critical part of their press release:
“Global recognition that COVID-19 is airborne shows UK is lagging behind.
Infection control guidance & PPE provision are out of date and are placing health and care staff at risk.”
nnng.org.uk/wp-content/upl…
“Global recognition that COVID-19 is airborne shows UK is lagging behind.
Infection control guidance & PPE provision are out of date and are placing health and care staff at risk.”
nnng.org.uk/wp-content/upl…

On 3 June 2021, an EXTREMELY important meeting took place…
An IPC Guidance Stakeholder Engagement meeting, hosted by the DHSC.
Members of the alliance of professional organisations & trade unions were invited.
This was a HUGE opportunity to finally have their voices heard…
An IPC Guidance Stakeholder Engagement meeting, hosted by the DHSC.
Members of the alliance of professional organisations & trade unions were invited.
This was a HUGE opportunity to finally have their voices heard…

In this clip, Rosemary Gallagher (IPC Lead at the RCN) is asked about this meeting.
Going into the meeting, it’s clear that hopes were high that this would be a turning point...
…that airborne transmission would finally be acknowledged and IPC guidance changed as a result.
Going into the meeting, it’s clear that hopes were high that this would be a turning point...
…that airborne transmission would finally be acknowledged and IPC guidance changed as a result.
However, concerns raised by the RCN & other members of the alliance were once again ignored & the IPC guidance remained unchanged.
“I think by that time for whatever reason the IPC guidance was so wedded to being predicated on droplets that it just didn’t change.”
“I think by that time for whatever reason the IPC guidance was so wedded to being predicated on droplets that it just didn’t change.”
In Rosemary Gallagher’s written statement, she reflects on what happened during that meeting on 3 June 2021:
“The questions we asked were not answered and our concerns were dismissed almost out of hand.”
“It did not deliver and we came away feeling belittled and patronised.”
“The questions we asked were not answered and our concerns were dismissed almost out of hand.”
“It did not deliver and we came away feeling belittled and patronised.”

You can read the full transcript from this meeting held on 3 June 2021 and see how it all played out in this fascinating thread from @1goodtern ⬇️
https://twitter.com/1goodtern/status/1860780623855505438
@1goodtern This brings us up to June 2021. That was nearly 3.5 years ago now.
So where are we TODAY?
First & foremost, as Prof Whitty & Prof Harries state in this Inquiry compilation clip, there is no longer any question amongst the scientific community as to whether Covid is airborne…
So where are we TODAY?
First & foremost, as Prof Whitty & Prof Harries state in this Inquiry compilation clip, there is no longer any question amongst the scientific community as to whether Covid is airborne…
@1goodtern …and the IPC experts (Dr Warne & Dr Shin) who provided independent specialist advice to the Covid Inquiry agreed that the IPC guidelines should now be updated to recommend the routine use of FFP3 masks when caring for patients with Covid - or indeed any other respiratory virus.
@1goodtern So why has this not happened already?
Well, there’s one big problem…
As shown in this clip, the current head of infection prevention & control for England, Dr Lisa Ritchie, STILL believes that DROPLET & CONTACT are the only modes of transmission that matter for Covid…
Well, there’s one big problem…
As shown in this clip, the current head of infection prevention & control for England, Dr Lisa Ritchie, STILL believes that DROPLET & CONTACT are the only modes of transmission that matter for Covid…
@1goodtern During her Inquiry hearing, Dr Ritchie was asked whether the IPC Cell had ever reached a point where they collectively thought that airborne transmission was a significant threat which needed to be guarded against (eg. With routine use of FFP3 masks)…
Dr Ritchie replied: “No.”
Dr Ritchie replied: “No.”
…and so, there are STILL no airborne mitigations for patients or staff in hospitals.
There are STILL no FFP3 masks for healthcare workers when dealing with Covid positive patients.
In fact, there are generally NO masks at all in hospitals anymore, not even surgical masks.
There are STILL no FFP3 masks for healthcare workers when dealing with Covid positive patients.
In fact, there are generally NO masks at all in hospitals anymore, not even surgical masks.

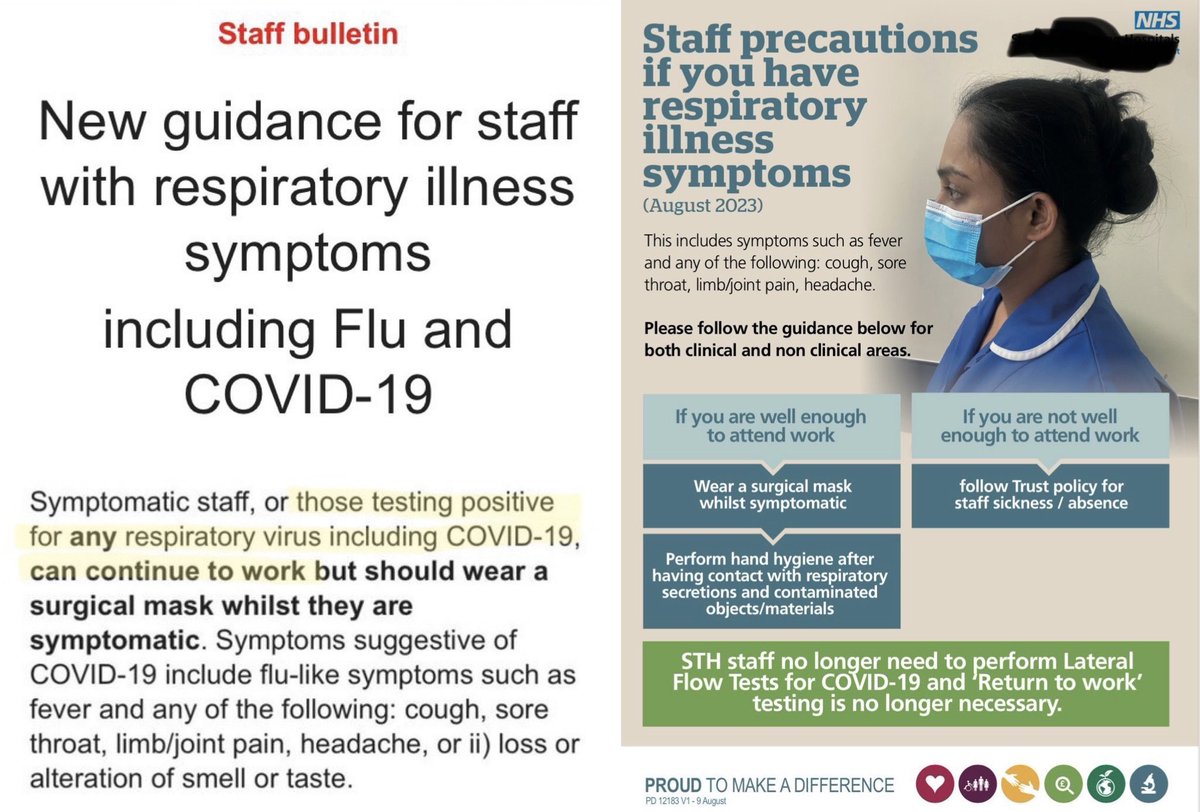
If NHS staff have Covid symptoms, they are told they don’t need to test & should still go to work.
If they go against guidance by testing & it’s POSITIVE, they should *still* go to work & just wear a flimsy surgical mask which does not protect against airborne transmission.
If they go against guidance by testing & it’s POSITIVE, they should *still* go to work & just wear a flimsy surgical mask which does not protect against airborne transmission.
As Matt Hancock pointed out during his testimony, the NHS had (and *still* has) a cultural problem with nosocomial (hospital-acquired) infections.
“…some hospitals said they didn’t want to test their staff because they might find too many staff with Covid.”
“…some hospitals said they didn’t want to test their staff because they might find too many staff with Covid.”
As Prof Beggs explains, the big problem with Covid transmission is that people are MOST infectious before developing symptoms.
Ms Carey sums it up perfectly:
“It’s a dangerous situation where people are walking around, feeling well, but could in fact be transmitting the virus.”
Ms Carey sums it up perfectly:
“It’s a dangerous situation where people are walking around, feeling well, but could in fact be transmitting the virus.”
In this short clip (from a lecture given in March 2023), Dr Fauci clearly explains the issues with asymptomatic transmission.
Importantly, he highlights that up to 59% of infections are thought to result from asymptomatic transmission.
Full lecture here:
Importantly, he highlights that up to 59% of infections are thought to result from asymptomatic transmission.
Full lecture here:
In April 2023, routine Covid testing for hospitalised patients was axed…
…so any asymptomatic cases which would previously have been flagged now go undetected.
Even symptomatic patients are generally not tested (unless it would inform treatment).
gov.uk/guidance/covid…
…so any asymptomatic cases which would previously have been flagged now go undetected.
Even symptomatic patients are generally not tested (unless it would inform treatment).
gov.uk/guidance/covid…

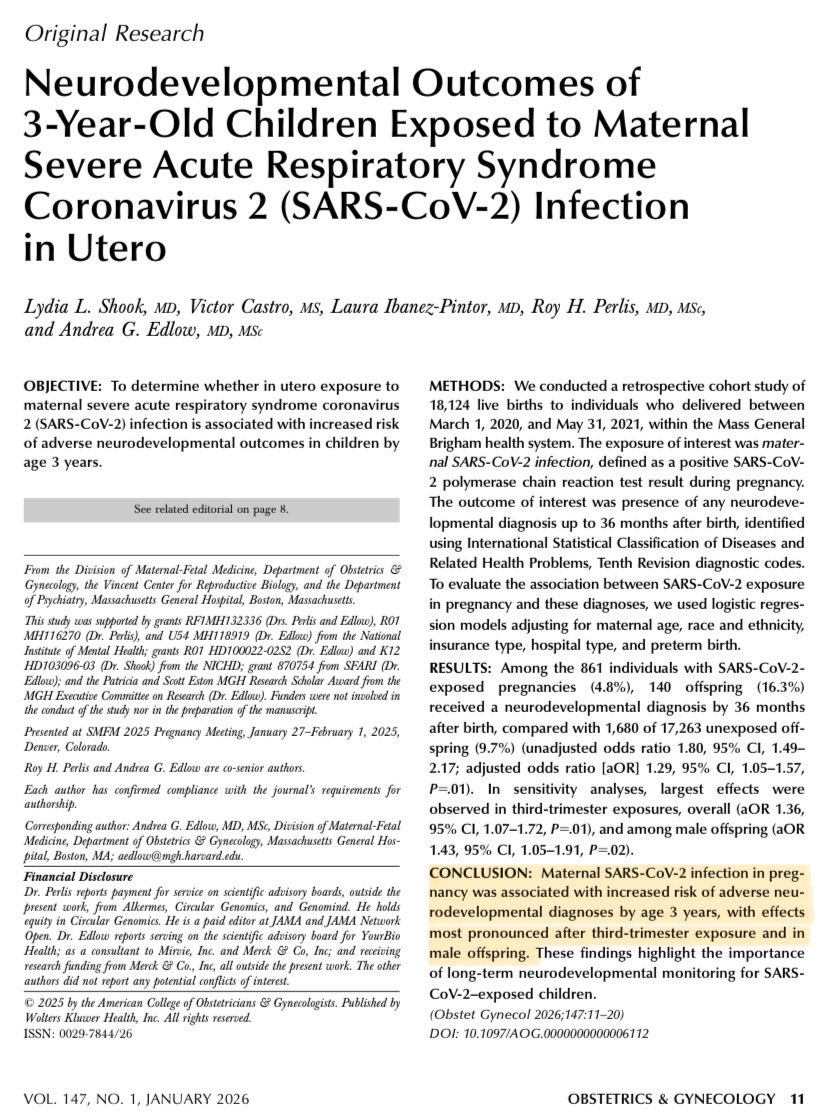
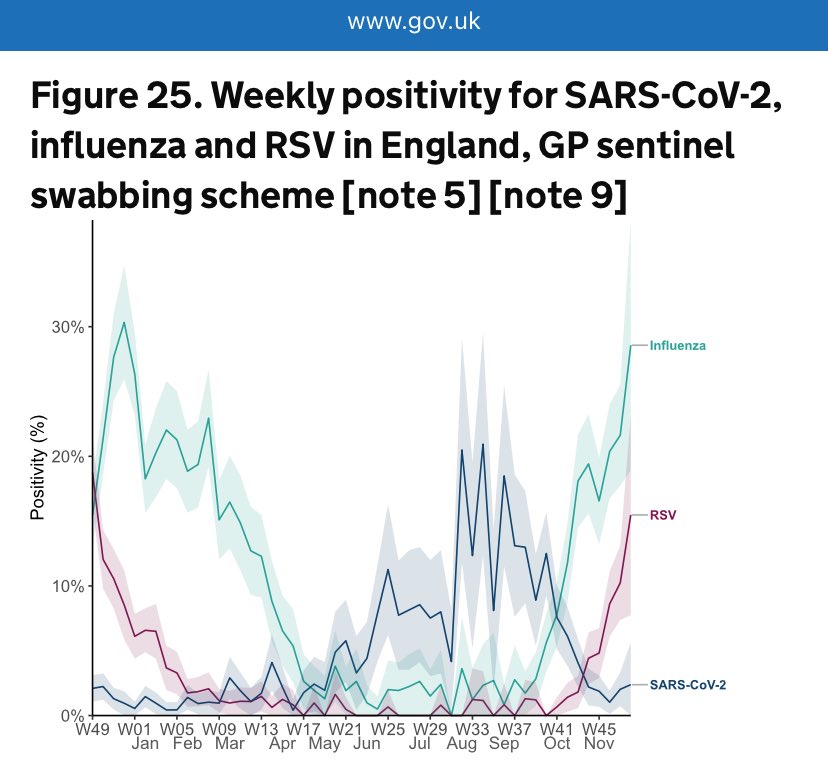
The SIREN healthcare study is based on fortnightly testing of a cohort of 6,000 health workers across the UK (irrespective of whether they have symptoms or not).
This chart really demonstrates the immense impact of Covid infections across the NHS workforce throughout the year.
This chart really demonstrates the immense impact of Covid infections across the NHS workforce throughout the year.

If you’ve made it this far, well done and thank you. 😊
But there’s still a little more to this story.
Please click “Show replies” one more time to view the last part of the thread.
⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️
But there’s still a little more to this story.
Please click “Show replies” one more time to view the last part of the thread.
⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️⬇️
Back to the SIREN study…
Even at the peak of last winter’s flu season, far more healthcare workers were infected with Covid than either flu or RSV.
During the Covid peaks (Sep 2023 & Jan 2024), prevalence hit ~4.5%.
That’s 1 in every 22 healthcare workers infected.
Even at the peak of last winter’s flu season, far more healthcare workers were infected with Covid than either flu or RSV.
During the Covid peaks (Sep 2023 & Jan 2024), prevalence hit ~4.5%.
That’s 1 in every 22 healthcare workers infected.

The chart below shows sickness absence rates for all NHS staff from Jan 2011 - May 2024.
It’s clear to see just how much more sickness absence there is since the start of the pandemic…
…because nothing is done to prevent it.
(Chart: @1goodtern)
digital.nhs.uk/data-and-infor…
It’s clear to see just how much more sickness absence there is since the start of the pandemic…
…because nothing is done to prevent it.
(Chart: @1goodtern)
digital.nhs.uk/data-and-infor…

But short-term illness is only the tip of the iceberg.
The other huge problem is long-term illness which results from repeated Covid infections.
This heart-breaking report from the BMA chronicles the debilitating effect Long Covid has on many doctors.
bma.org.uk/media/7318/bma…
The other huge problem is long-term illness which results from repeated Covid infections.
This heart-breaking report from the BMA chronicles the debilitating effect Long Covid has on many doctors.
bma.org.uk/media/7318/bma…

In this clip, Patricia Temple (Staff Nurse) discusses the impact of Long Covid on nurses:
“I have a lot of nurses that I know who are trying very very hard to stay in the workplace and are unable to do so.”
“You can’t be clapped for one minute and declared disposable the next.”
“I have a lot of nurses that I know who are trying very very hard to stay in the workplace and are unable to do so.”
“You can’t be clapped for one minute and declared disposable the next.”
This issue of NHS staff leaving the workforce due to Long Covid is more common than most people realise.
The BMA report revealed:
“The impact on doctors' ability to work is considerable & devastating, with nearly 1 in 5 responding doctors [with Long Covid] left unable to work.”
The BMA report revealed:
“The impact on doctors' ability to work is considerable & devastating, with nearly 1 in 5 responding doctors [with Long Covid] left unable to work.”

And it’s not just doctors.
This 1 in 5 number comes up again & again as the approximate proportion of people with Long Covid who are severely affected, with their ability to undertake day-to-day activities “limited a lot”.
ons.gov.uk/peoplepopulati…
This 1 in 5 number comes up again & again as the approximate proportion of people with Long Covid who are severely affected, with their ability to undertake day-to-day activities “limited a lot”.
ons.gov.uk/peoplepopulati…

The really concerning thing is that a recent study from King’s College London revealed that:
▪️Over a THIRD (33.6%) of healthcare workers in England are now suffering from Long Covid.
This is not sustainable.
kcl.ac.uk/news/long-covi…
▪️Over a THIRD (33.6%) of healthcare workers in England are now suffering from Long Covid.
This is not sustainable.
kcl.ac.uk/news/long-covi…

Of course, it’s not just staff affected by high rates of Covid transmission in hospitals.
Patients are too.
Hospital-acquired infections are no longer reported in England, but they are in Wales where a staggering 70% of patients currently in hospital with Covid caught it there.
Patients are too.
Hospital-acquired infections are no longer reported in England, but they are in Wales where a staggering 70% of patients currently in hospital with Covid caught it there.

This meta-analysis amalgamated the results of 21 studies across 8 countries to reveal that:
🚨Hospital-acquired Covid infection increases the in-hospital death rate by 30%.
🚨For immunocompromised patients, the in-hospital death rate is DOUBLED.
frontiersin.org/journals/immun…
🚨Hospital-acquired Covid infection increases the in-hospital death rate by 30%.
🚨For immunocompromised patients, the in-hospital death rate is DOUBLED.
frontiersin.org/journals/immun…

During her testimony, Dr @Cathy_Finnis from Clinically Vulnerable Families perfectly articulated the terrible situation which clinically vulnerable patients face when needing to access healthcare.
The question she asks at 1:05 in this clip left the whole room speechless.
The question she asks at 1:05 in this clip left the whole room speechless.
As you can hopefully see from the reams of evidence above, the Covid Inquiry has highlighted serious flaws in the current infection control (IPC) guidance, particularly in terms of PPE & ventilation in hospitals.
Surely there’s enough evidence for the NHS to finally take action?
Surely there’s enough evidence for the NHS to finally take action?
But there’s a problem…
The letter below, sent to @EvonneTCurran from the Chief Nursing Officers, suggests that any relevant learnings from the Inquiry will only be incorporated AFTER publication of the Inquiry's module 3 findings…
…but that could be a year or more away! 🤯
The letter below, sent to @EvonneTCurran from the Chief Nursing Officers, suggests that any relevant learnings from the Inquiry will only be incorporated AFTER publication of the Inquiry's module 3 findings…
…but that could be a year or more away! 🤯

Thankfully the alliance (CATA) are on the case once more…
They’ve published an open letter highlighting that it is “completely unacceptable” & an “abrogation of responsibility” to await publication of the Inquiry’s findings before addressing the issues.
bapen.org.uk/pdfs/covid-19/…
They’ve published an open letter highlighting that it is “completely unacceptable” & an “abrogation of responsibility” to await publication of the Inquiry’s findings before addressing the issues.
bapen.org.uk/pdfs/covid-19/…

Enough is enough.
“The level of criminal incompetence exposed by recent witnesses to the UK COVID-19 Inquiry … has proven that many, if not most, of over 230,000 deaths were preventable.”
It’s time for change.
thelancet.com/journals/lance…
“The level of criminal incompetence exposed by recent witnesses to the UK COVID-19 Inquiry … has proven that many, if not most, of over 230,000 deaths were preventable.”
It’s time for change.
thelancet.com/journals/lance…

A new petition calling on the govt to introduce of new air quality & PPE guidelines in health & social care settings has been set up.
If you agree that, after nearly 5 yrs of inaction, it’s high time this situation was addressed, please sign & share ✍🏻
petition.parliament.uk/petitions/7003…
If you agree that, after nearly 5 yrs of inaction, it’s high time this situation was addressed, please sign & share ✍🏻
petition.parliament.uk/petitions/7003…

A couple of extra points I want to add…
Remember when I mentioned how NHS staff sickness absences are still far higher than pre-pandemic?
This is a really useful chart from @1goodtern which shows the clear correlation between NHS staff absences & Covid patients in hospital.
Remember when I mentioned how NHS staff sickness absences are still far higher than pre-pandemic?
This is a really useful chart from @1goodtern which shows the clear correlation between NHS staff absences & Covid patients in hospital.
https://twitter.com/_CatintheHat/status/1861047246470406561

I also wanted to add a few additional points about the importance of VENTILATION in infection control…
During Prof Beggs’ hearing, he described how the current hospital ventilation guidelines (for general areas & wards) are hopelessly out of date & completely unfit for purpose.
During Prof Beggs’ hearing, he described how the current hospital ventilation guidelines (for general areas & wards) are hopelessly out of date & completely unfit for purpose.
Prof Beggs also discussed how the ventilation rates on hospital wards are often well below those specified in the guidelines…
…and bear in mind that those guidelines are deemed to be inadequate for infection control purposes, so most wards aren’t even meeting that low bar.
…and bear in mind that those guidelines are deemed to be inadequate for infection control purposes, so most wards aren’t even meeting that low bar.
Prof Beggs then talked about the “huge potential” of using HEPA air filters.
It would “costs a fortune” to change the whole mechanical ventilation system in hospitals…
“…but you can bring in portable air cleaners and, in theory, achieve the same effect, relatively cheaply.”
It would “costs a fortune” to change the whole mechanical ventilation system in hospitals…
“…but you can bring in portable air cleaners and, in theory, achieve the same effect, relatively cheaply.”
Prof Chris Whitty (Chief Medical Officer) also emphasised the importance of ventilation during his Covid Inquiry testimony…
“We should be taking ventilation of public buildings a lot more seriously and probably more vigorously than we previously had.”
“We should be taking ventilation of public buildings a lot more seriously and probably more vigorously than we previously had.”
This view is further endorsed by a report from the Royal Academy of Engineering where they urged the government to undertake a major upgrade of ventilation & air filtration systems, particularly in community buildings like HOSPITALS and SCHOOLS.
raeng.org.uk/media/dmkplpl0…
raeng.org.uk/media/dmkplpl0…

Earlier this year, Sir Patrick Vallance warned that another pandemic is “absolutely inevitable” & urged the incoming government to focus on preparing for it.
Improvements to ventilation will not only reduce the spread of illness now; it will also be an investment for the future.
Improvements to ventilation will not only reduce the spread of illness now; it will also be an investment for the future.

I’ll end with some wise words written by Florence Nightingale back in 1859:
“The very first canon of nursing […] the first essential to the patient, without which all the rest you can do for him is as nothing[…] is this: TO KEEP THE AIR HE BREATHES AS PURE AS THE EXTERNAL AIR”
“The very first canon of nursing […] the first essential to the patient, without which all the rest you can do for him is as nothing[…] is this: TO KEEP THE AIR HE BREATHES AS PURE AS THE EXTERNAL AIR”

• • •
Missing some Tweet in this thread? You can try to
force a refresh