1 in 3 COVID-19 survivors may develop a neuropsychiatric or neurological condition within 6 months.
From anosmia to strokes, the virus can leave lasting effects on the brain.
Research shows over 33% of post-COVID patients develop conditions like anxiety, depression, or cognitive dysfunction (Taquet et al., 2021).
Here’s how SARS-CoV-2 impacts the Central Nervous System (CNS), its neuropsychiatric sequelae, and the key considerations for clinicians 👇🧵
From anosmia to strokes, the virus can leave lasting effects on the brain.
Research shows over 33% of post-COVID patients develop conditions like anxiety, depression, or cognitive dysfunction (Taquet et al., 2021).
Here’s how SARS-CoV-2 impacts the Central Nervous System (CNS), its neuropsychiatric sequelae, and the key considerations for clinicians 👇🧵
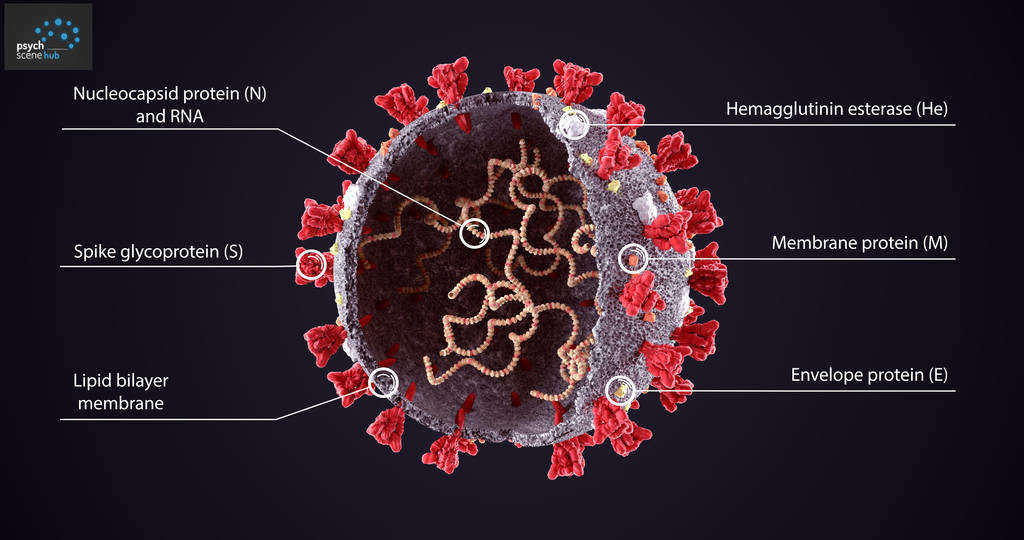
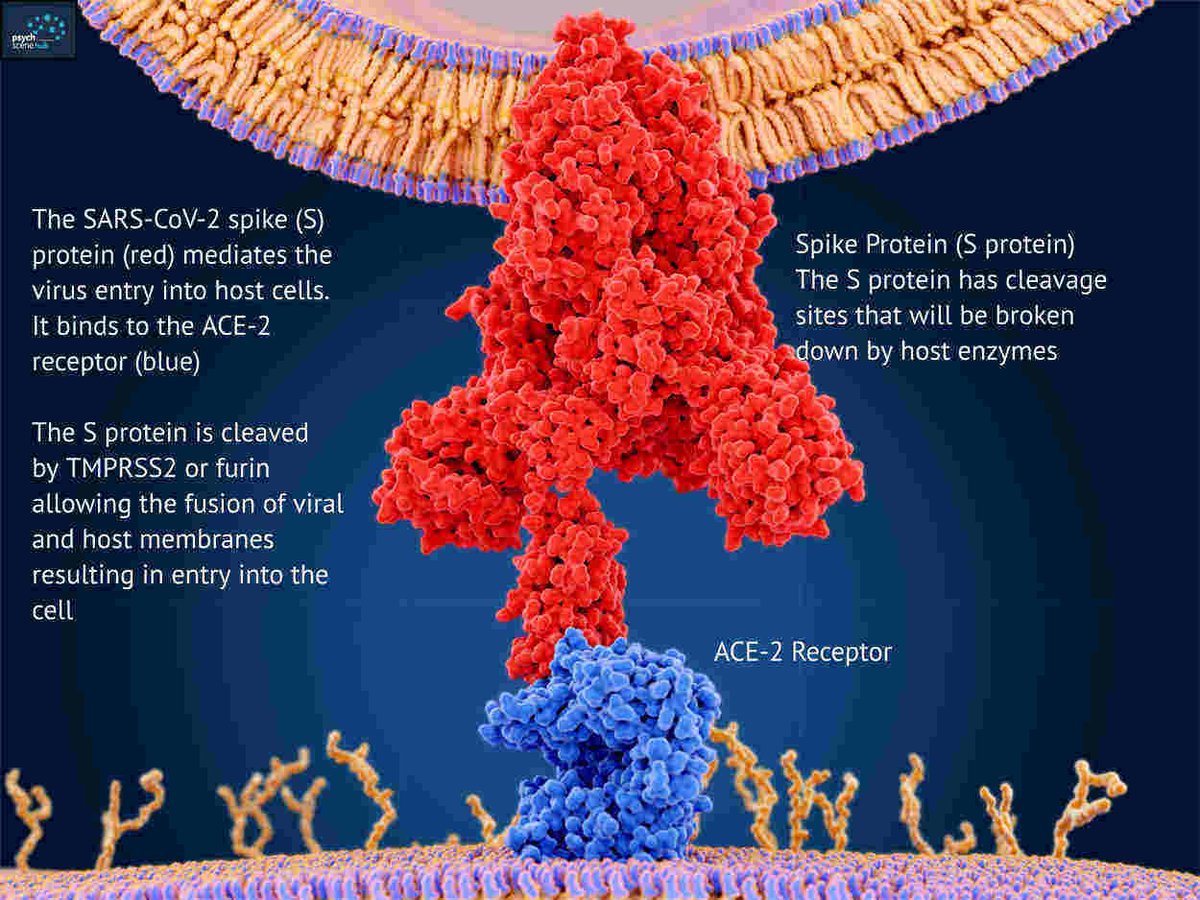
How does SARS-CoV-2 'invade' the CNS (central nervous system)?
Olfactory route: The virus binds ACE2 (angiotensin-converting enzyme 2) receptors, travels via the olfactory bulb and enters the brain.
Bloodstream: Disrupted BBB (blood-brain barrier) allows infected monocytes and cytokines to enter.
Viral RNA in cerebrospinal fluid supports CNS involvement (Moriguchi et al., 2020).
Olfactory route: The virus binds ACE2 (angiotensin-converting enzyme 2) receptors, travels via the olfactory bulb and enters the brain.
Bloodstream: Disrupted BBB (blood-brain barrier) allows infected monocytes and cytokines to enter.
Viral RNA in cerebrospinal fluid supports CNS involvement (Moriguchi et al., 2020).
Anosmia And Dysgeusia
Anosmia (loss of smell) and dysgeusia (loss of taste) occur as SARS-CoV-2 targets ACE2 receptors in the olfactory epithelium, impairing neural pathways.
Research shows anosmia often precedes respiratory symptoms (Spinato et al., 2020).
💡 Psych Scene Tip: Persistent anosmia >6 weeks may indicate neuroinflammation—monitor recovery timelines closely.
Anosmia (loss of smell) and dysgeusia (loss of taste) occur as SARS-CoV-2 targets ACE2 receptors in the olfactory epithelium, impairing neural pathways.
Research shows anosmia often precedes respiratory symptoms (Spinato et al., 2020).
💡 Psych Scene Tip: Persistent anosmia >6 weeks may indicate neuroinflammation—monitor recovery timelines closely.

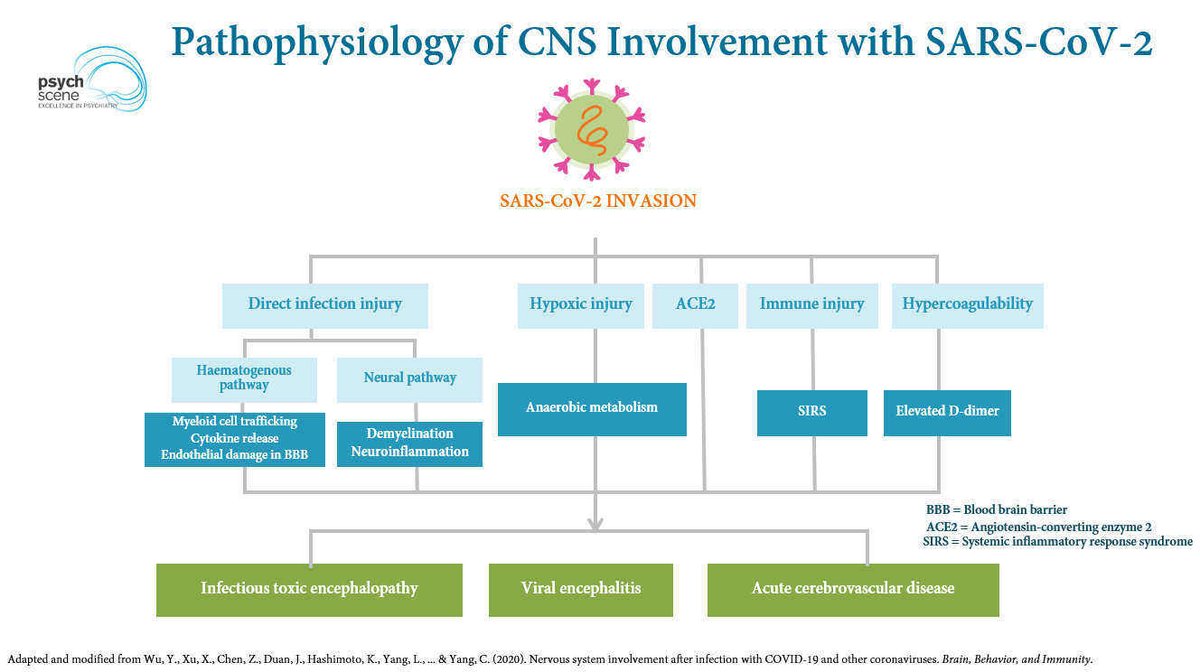
Pathophysiology Of CNS Involvement
SARS-CoV-2 affects the CNS via:
Direct infection: Viral invasion damages neurons.
Hypoxia: Oxygen deprivation triggers neuronal injury.
Cytokine storm: Pro-inflammatory cytokines disrupt the BBB.
Hypercoagulability: Microthrombi increase stroke risk.
SARS-CoV-2 affects the CNS via:
Direct infection: Viral invasion damages neurons.
Hypoxia: Oxygen deprivation triggers neuronal injury.
Cytokine storm: Pro-inflammatory cytokines disrupt the BBB.
Hypercoagulability: Microthrombi increase stroke risk.
Neuropsychiatric Symptoms In COVID-19 Patients
Hospitalised patients often present with delirium, agitation, or encephalopathy. Long-COVID symptoms include brain fog, anxiety, and PTSD (post-traumatic stress disorder).
69% of ICU survivors had agitation, and 33% developed dysexecutive syndrome (Helms et al., 2020).
💡 Psych Scene Tip: Use tools like the FAB (Frontal Assessment Battery) to evaluate dysexecutive symptoms post-ICU.
Hospitalised patients often present with delirium, agitation, or encephalopathy. Long-COVID symptoms include brain fog, anxiety, and PTSD (post-traumatic stress disorder).
69% of ICU survivors had agitation, and 33% developed dysexecutive syndrome (Helms et al., 2020).
💡 Psych Scene Tip: Use tools like the FAB (Frontal Assessment Battery) to evaluate dysexecutive symptoms post-ICU.
The Long Tail of COVID-19
Long-COVID includes:
• Chronic fatigue.
• Cognitive deficits resembling encephalopathy.
• Sleep disturbances and PTSD.
32% of long-COVID patients report persistent neurocognitive symptoms (Evans et al., 2021).
Long-COVID includes:
• Chronic fatigue.
• Cognitive deficits resembling encephalopathy.
• Sleep disturbances and PTSD.
32% of long-COVID patients report persistent neurocognitive symptoms (Evans et al., 2021).
COVID-19 increases stroke risk
Hypercoagulability in COVID-19 causes:
Ischaemic strokes (microthrombi).
Haemorrhages (endothelial damage).
Elevated D-dimer correlates with thrombotic complications (Mao et al., 2020).
💡 Psych Scene Tip: Assess post-COVID patients for subtle neurovascular signs like aphasia or hemiparesis.
Hypercoagulability in COVID-19 causes:
Ischaemic strokes (microthrombi).
Haemorrhages (endothelial damage).
Elevated D-dimer correlates with thrombotic complications (Mao et al., 2020).
💡 Psych Scene Tip: Assess post-COVID patients for subtle neurovascular signs like aphasia or hemiparesis.
Psychiatric Manifestations In ICU Survivors
ICU stays often result in long-term psychiatric effects like PTSD, depression, or anxiety.
25–50% of ICU survivors experience lasting psychiatric symptoms (Sukantarat et al., 2007).
💡 Psych Scene Tip: For ICU survivors with PTSD, consider trauma-focused CBT (cognitive behavioural therapy) and short-term psychotropics.
ICU stays often result in long-term psychiatric effects like PTSD, depression, or anxiety.
25–50% of ICU survivors experience lasting psychiatric symptoms (Sukantarat et al., 2007).
💡 Psych Scene Tip: For ICU survivors with PTSD, consider trauma-focused CBT (cognitive behavioural therapy) and short-term psychotropics.
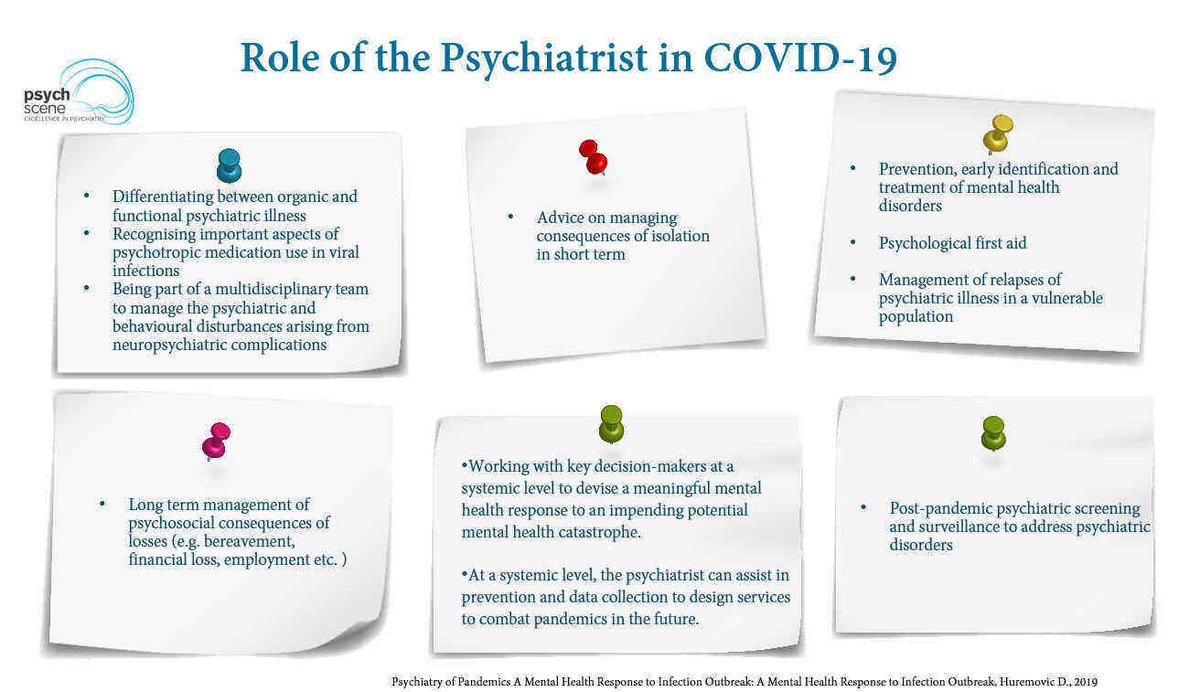
The Psychiatrist’s Role In Covid-19 Care
When addressing neuropsychiatric complications like PTSD, depression, and cognitive dysfunction. Multidisciplinary collaboration is key.
Research shows early intervention reduces pandemic-related mental health fallout (Huremović et al., 2019).
When addressing neuropsychiatric complications like PTSD, depression, and cognitive dysfunction. Multidisciplinary collaboration is key.
Research shows early intervention reduces pandemic-related mental health fallout (Huremović et al., 2019).
Brain fog, fatigue, PTSD, and cognitive impairment are common post-COVID.
Improve your expertise in assessing and managing these conditions.
Join our Chronic Fatigue Syndrome (ME/CFS) & Long COVID Masterclass to learn:
✅ Neuropsychiatric sequelae of SARS-CoV-2
✅ Cognitive impairment & fatigue management
✅ Practical treatment strategies for Long COVID
Click the link below to get access:
psychscene.co/3Q3gpDn
Improve your expertise in assessing and managing these conditions.
Join our Chronic Fatigue Syndrome (ME/CFS) & Long COVID Masterclass to learn:
✅ Neuropsychiatric sequelae of SARS-CoV-2
✅ Cognitive impairment & fatigue management
✅ Practical treatment strategies for Long COVID
Click the link below to get access:
psychscene.co/3Q3gpDn
• • •
Missing some Tweet in this thread? You can try to
force a refresh