
We provide psychiatry education for Psychiatrists, GPs & Mental Health Practitioners. • Join The Academy 👇
3 subscribers
How to get URL link on X (Twitter) App

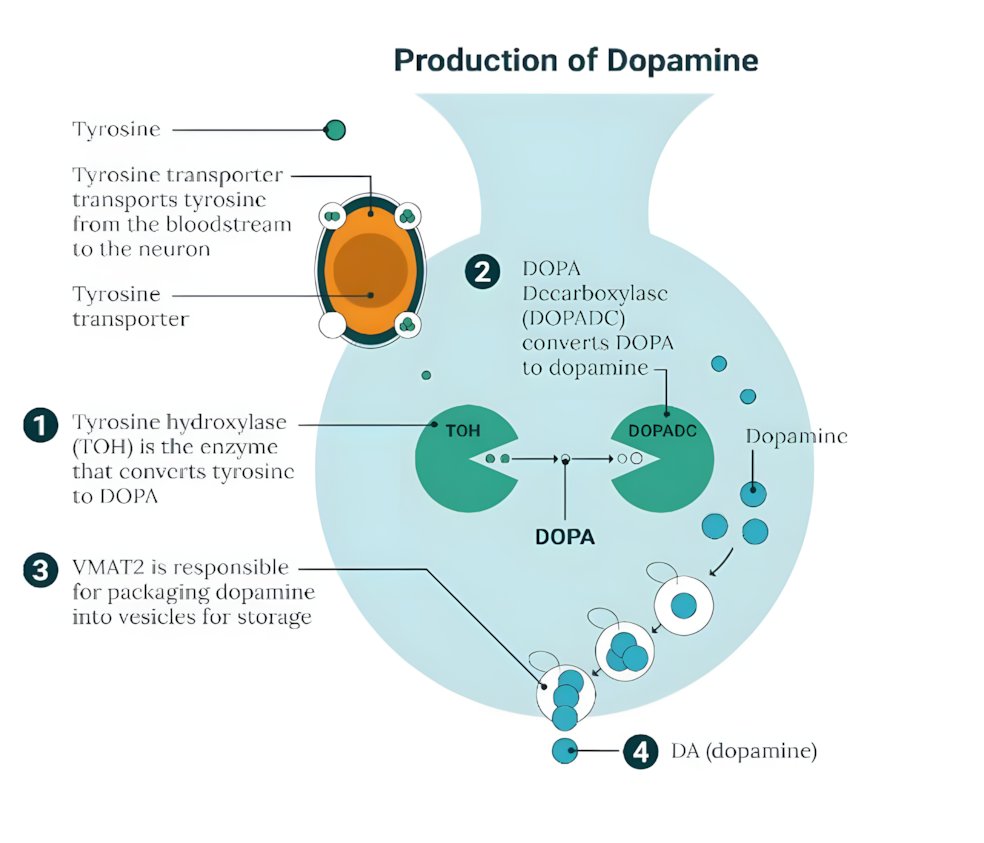
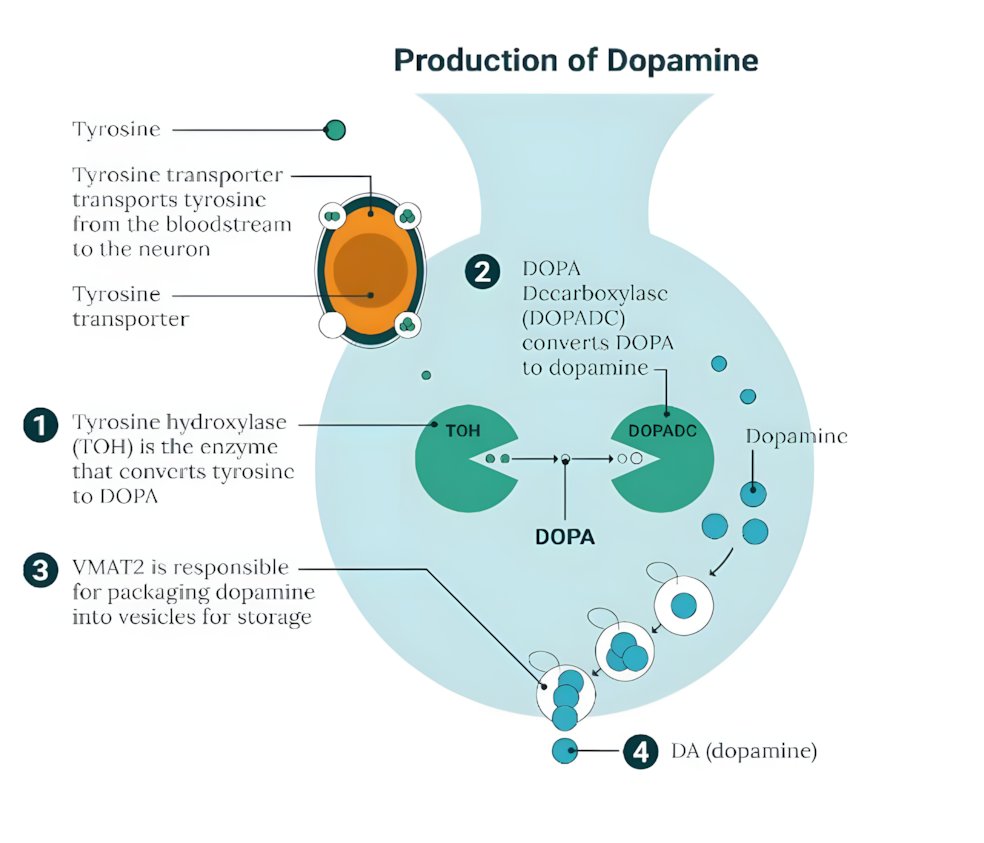 The primary mechanism linking low iron to ADHD involves the enzymatic production of dopamine.
The primary mechanism linking low iron to ADHD involves the enzymatic production of dopamine.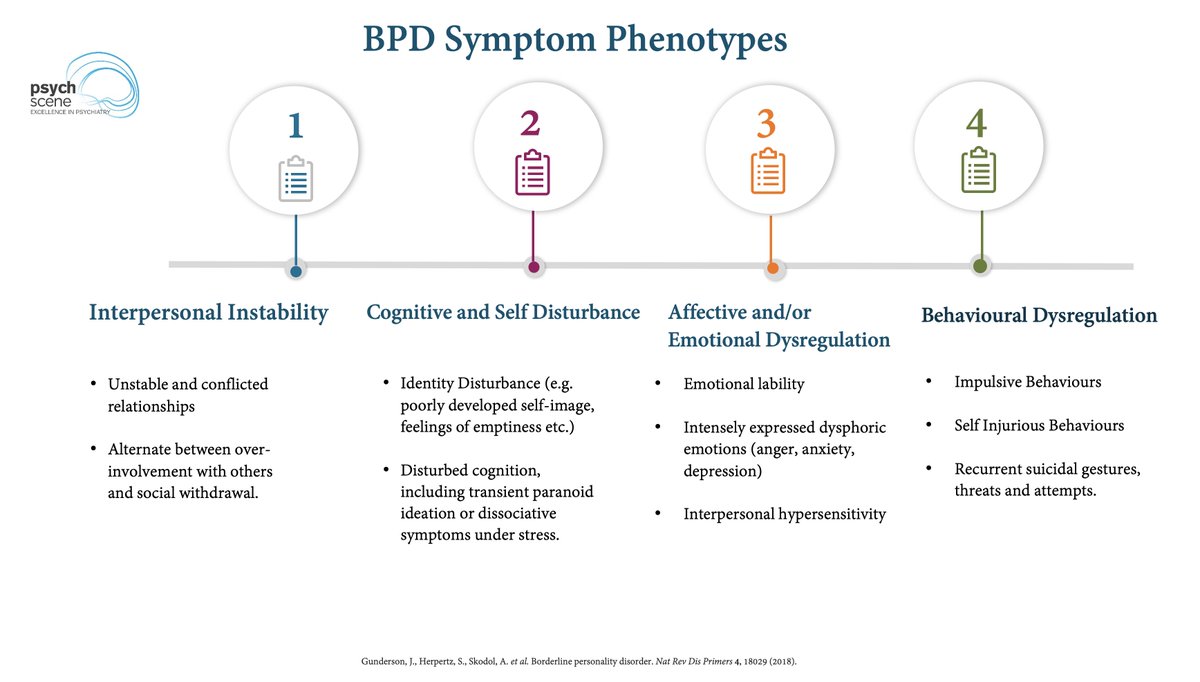
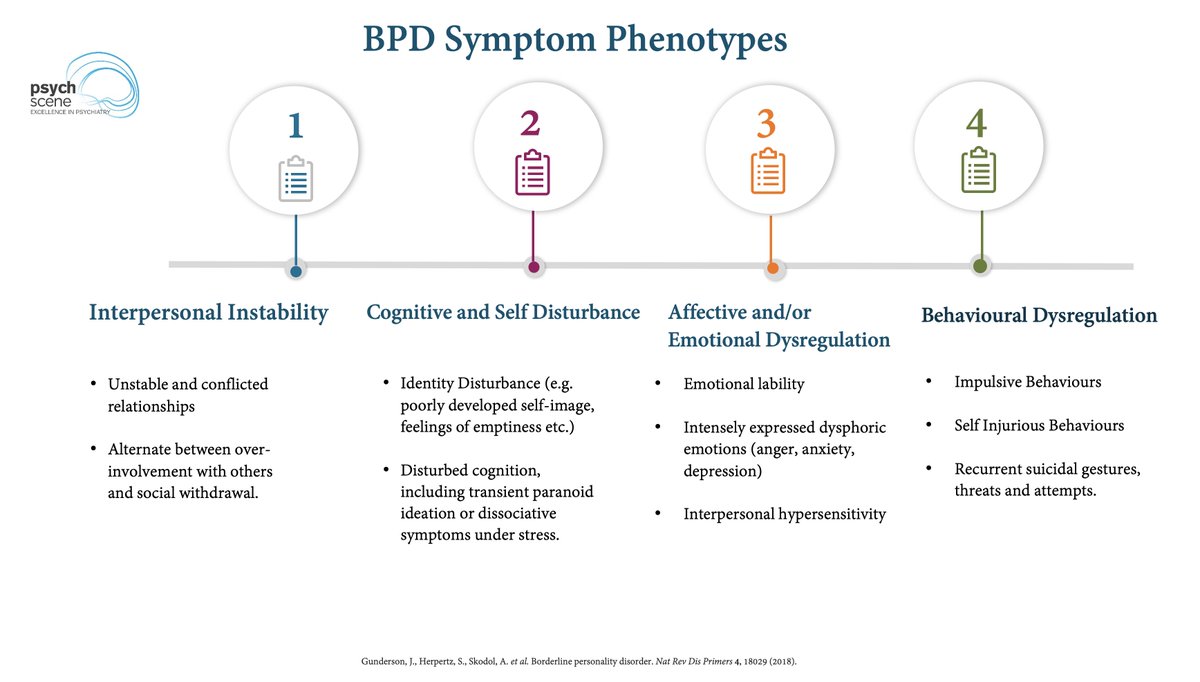 Antidepressants aren’t ‘designed’ for core BPD pathology
Antidepressants aren’t ‘designed’ for core BPD pathology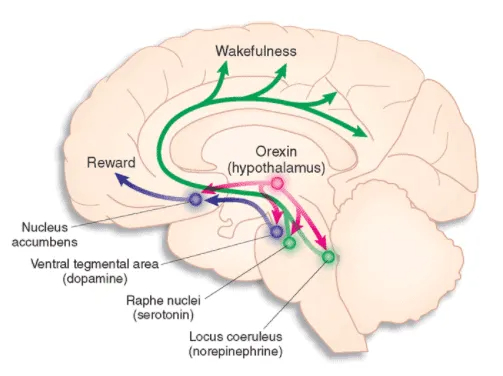
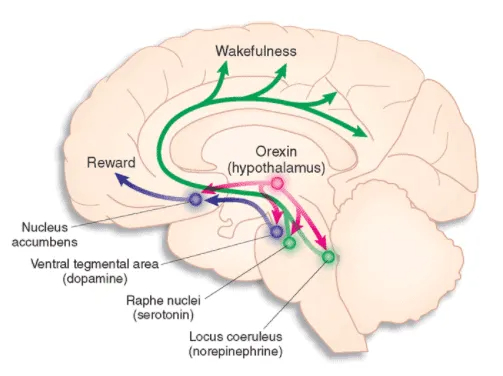 Classic view: LC goes quiet at night.
Classic view: LC goes quiet at night.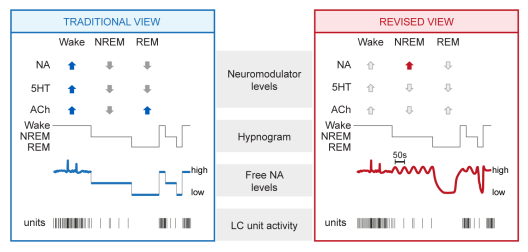
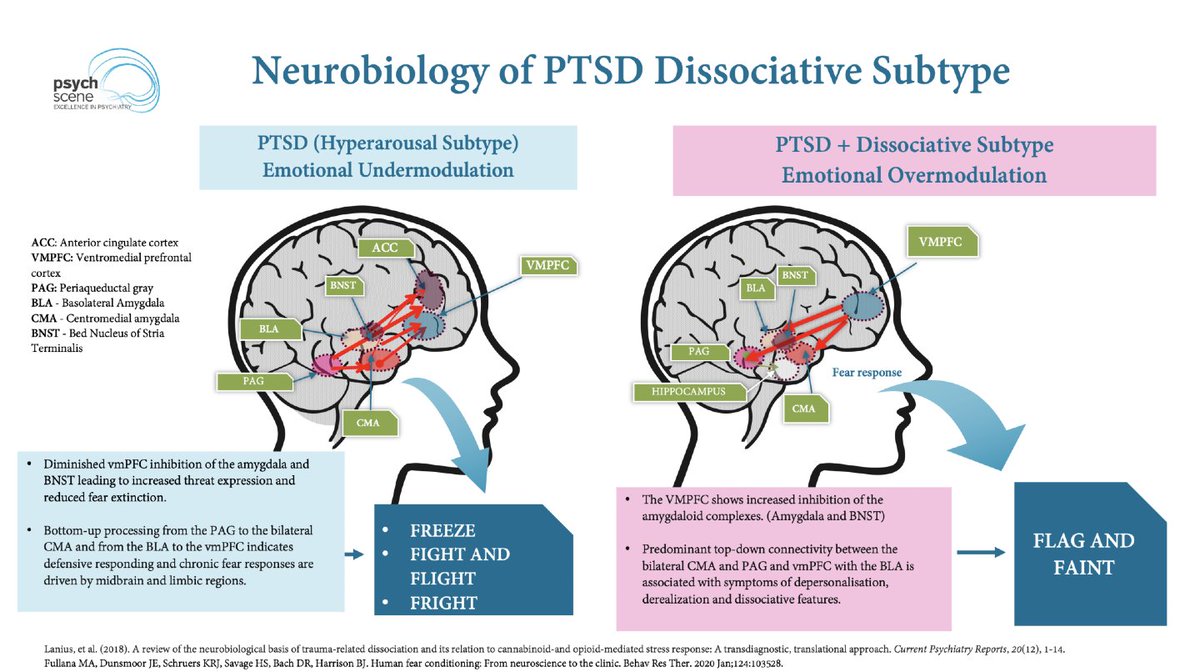 Dissociation in PTSD is often associated with the emotional overmodulation subtype (PTSD+DS).
Dissociation in PTSD is often associated with the emotional overmodulation subtype (PTSD+DS).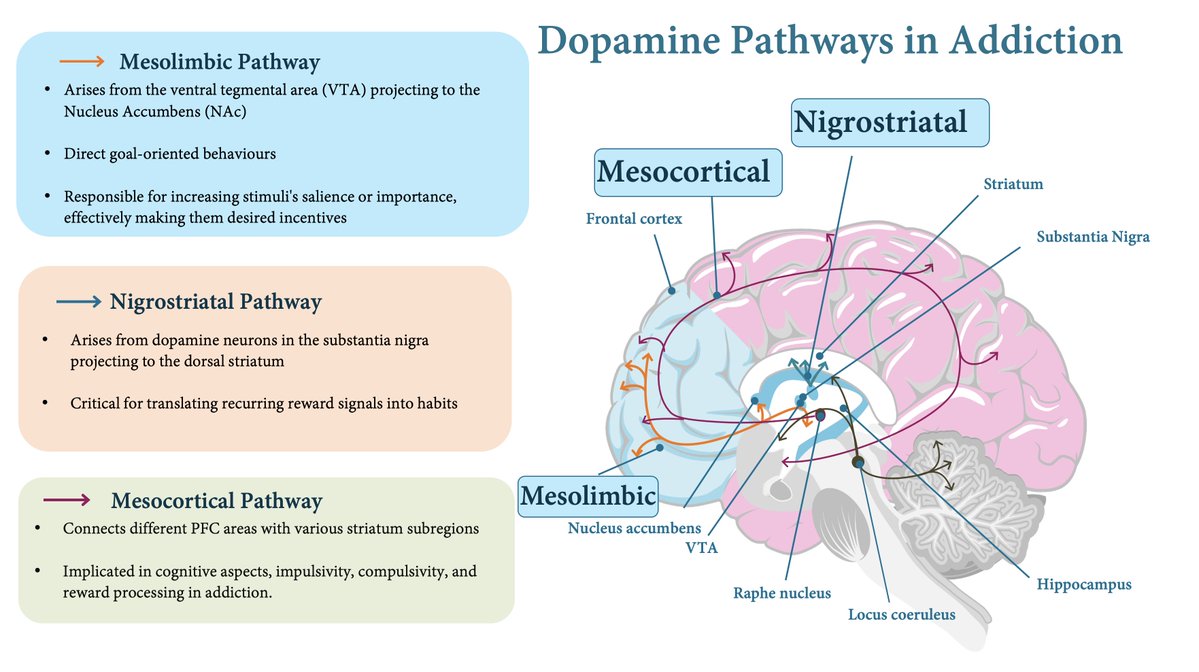
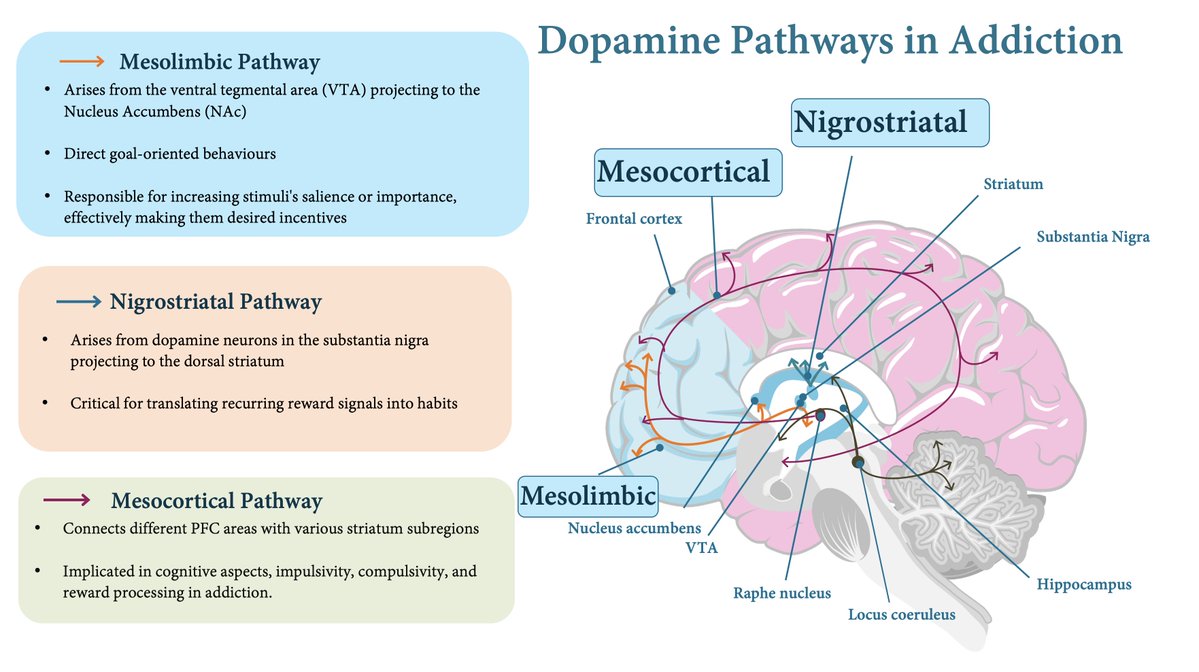 Addiction Impairs Prefrontal Control (“Hypofrontality”)
Addiction Impairs Prefrontal Control (“Hypofrontality”)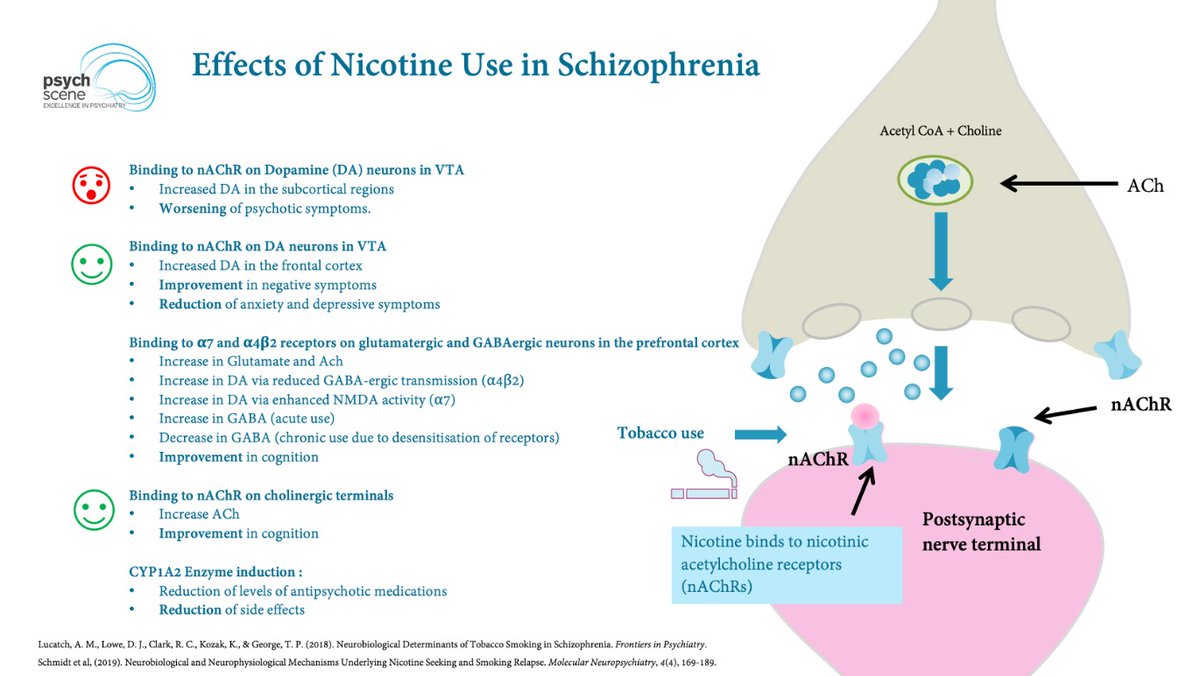
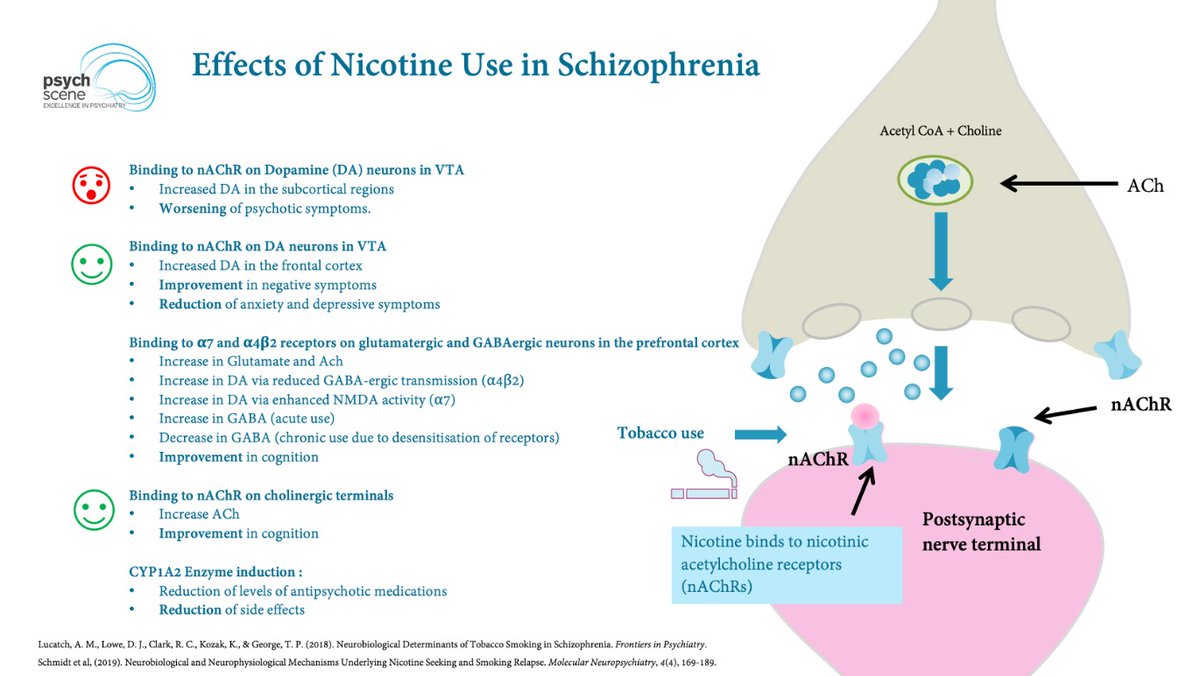 The isoenzyme CYP1A2 is highly induced by smoking tobacco.
The isoenzyme CYP1A2 is highly induced by smoking tobacco.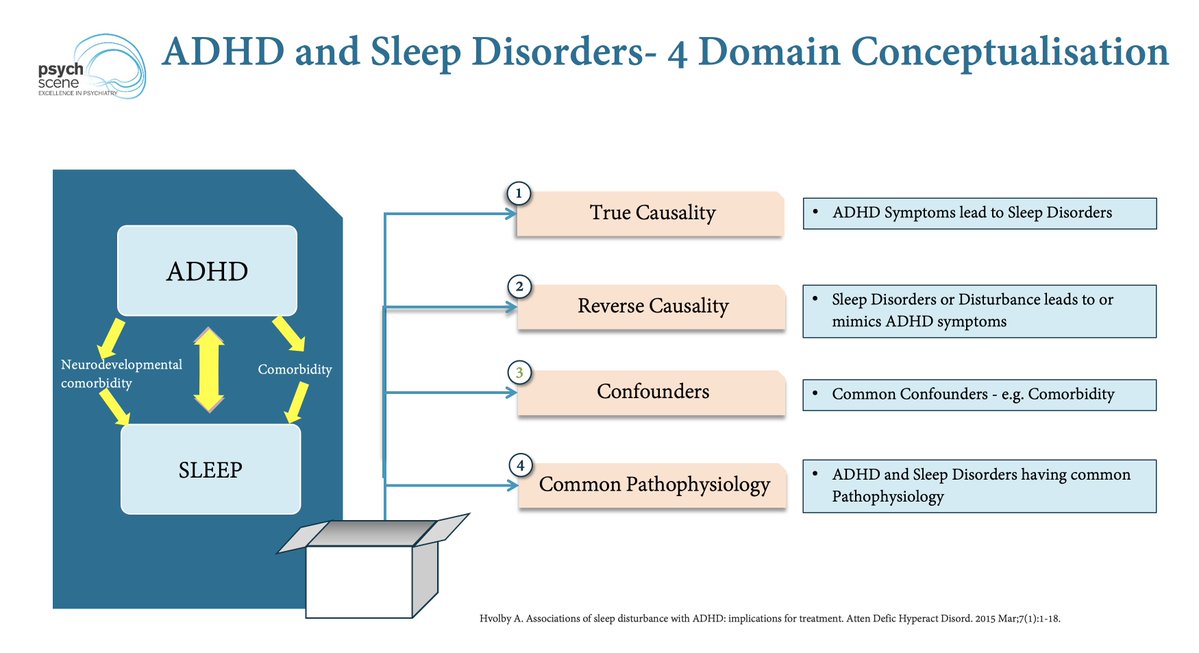
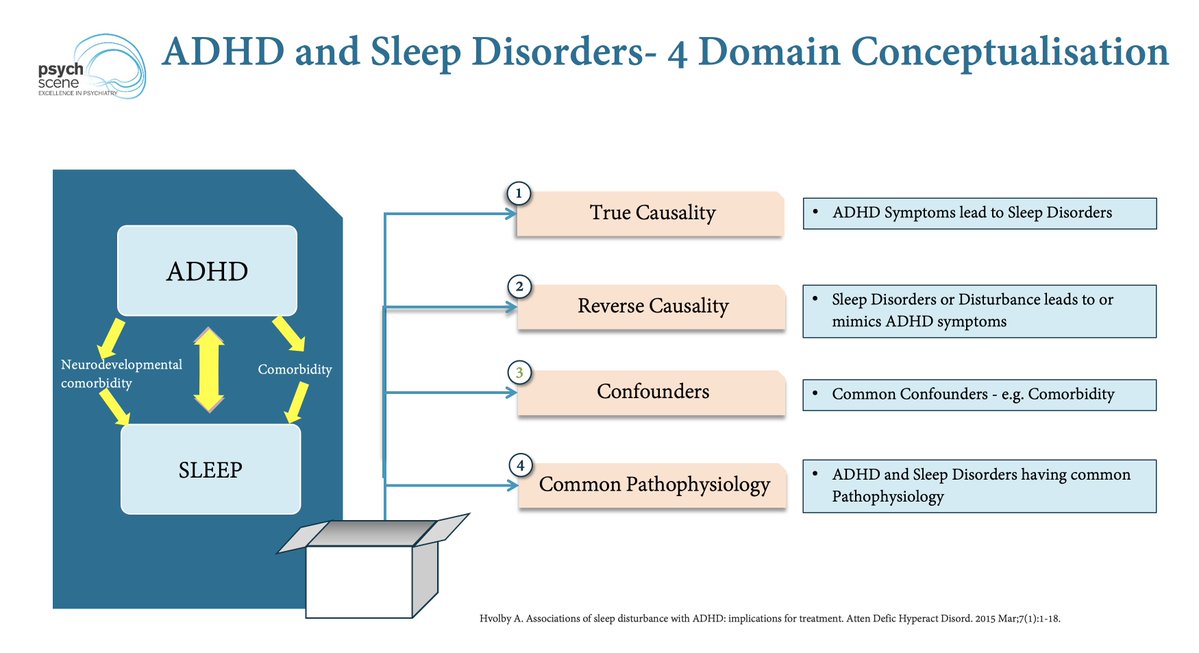 The reason why standard sleep therapy falls short often begins with ADHD's "intrinsic" biological clock.
The reason why standard sleep therapy falls short often begins with ADHD's "intrinsic" biological clock.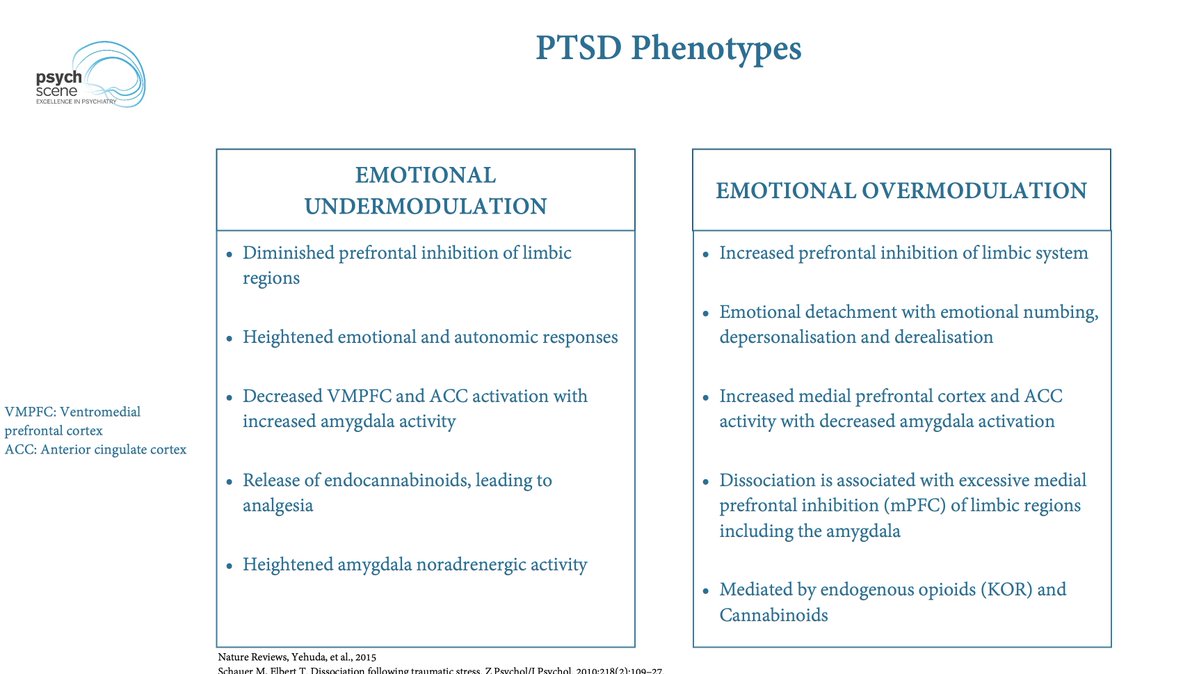
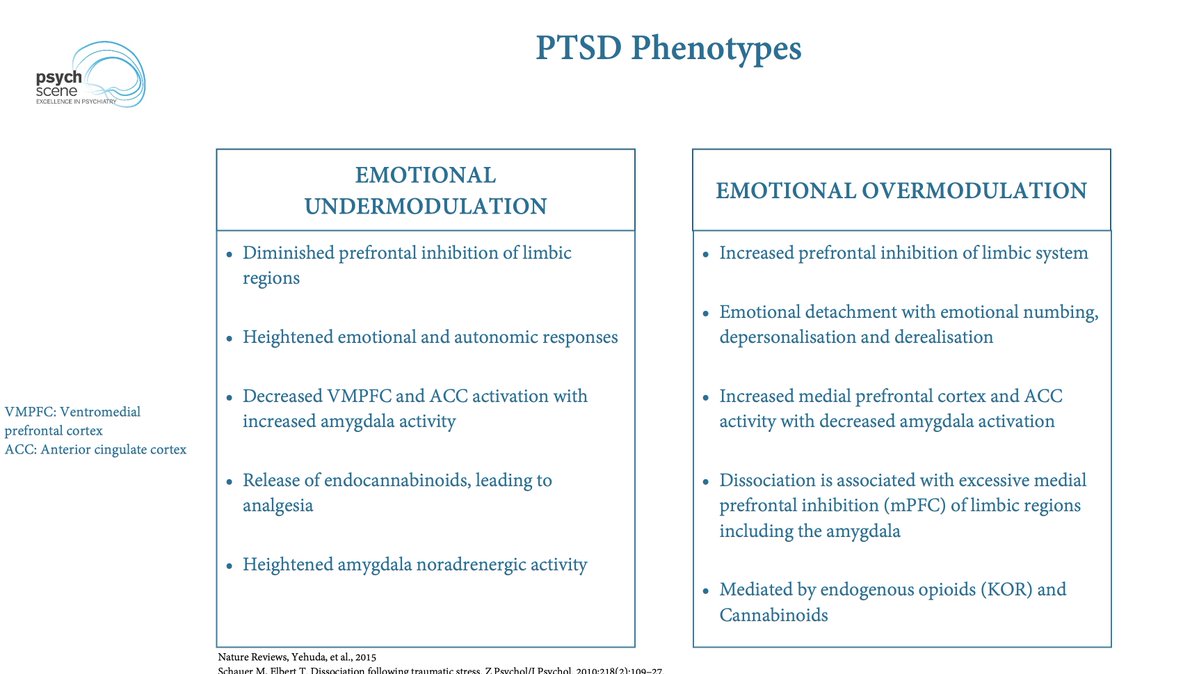 The classic hyperarousal PTSD phenotype represents emotional under-modulation.
The classic hyperarousal PTSD phenotype represents emotional under-modulation.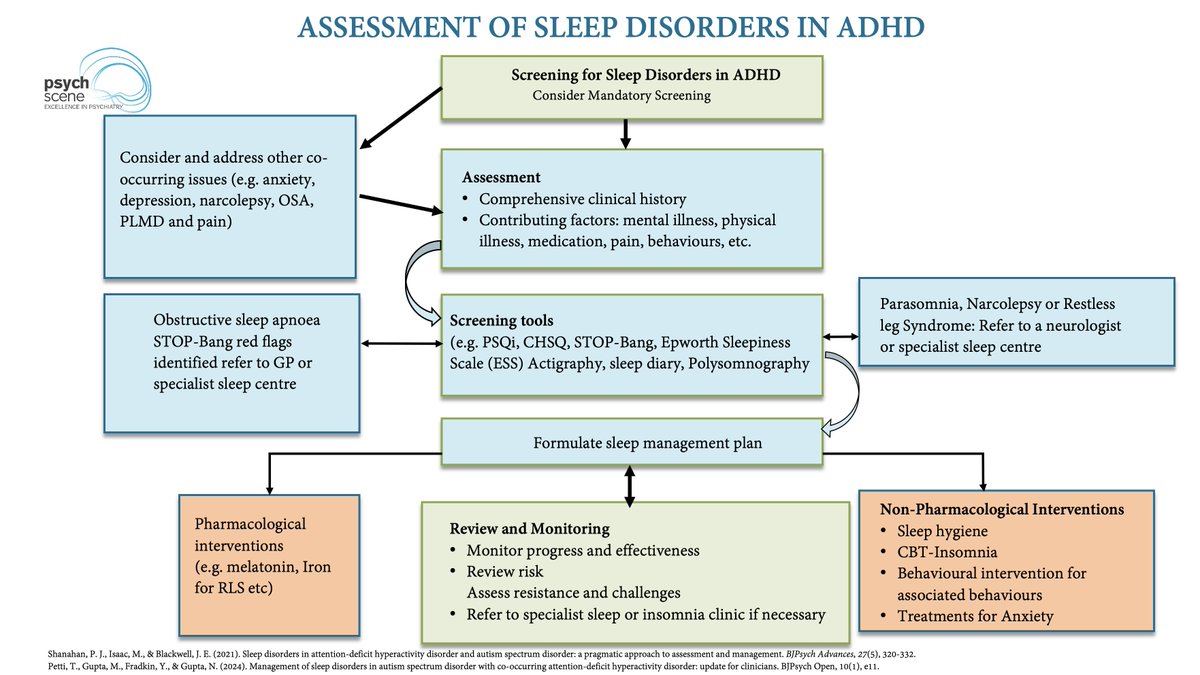
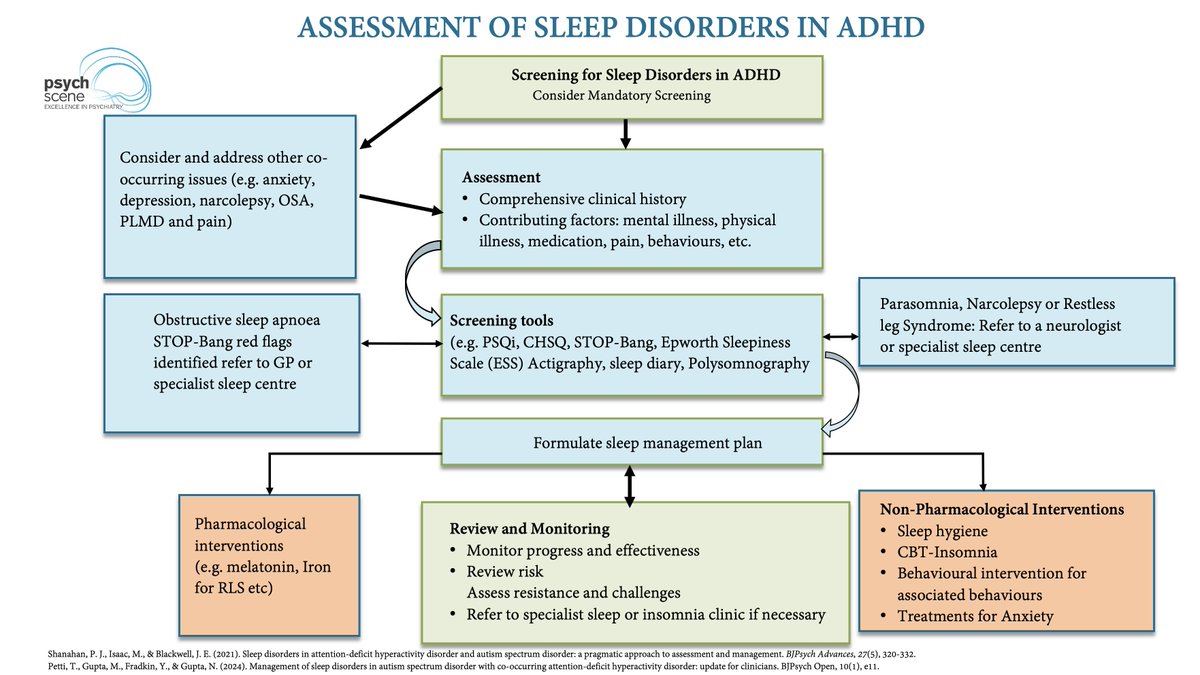 The mechanism of OSA-induced ADHD exacerbation is driven by severe sleep fragmentation.
The mechanism of OSA-induced ADHD exacerbation is driven by severe sleep fragmentation.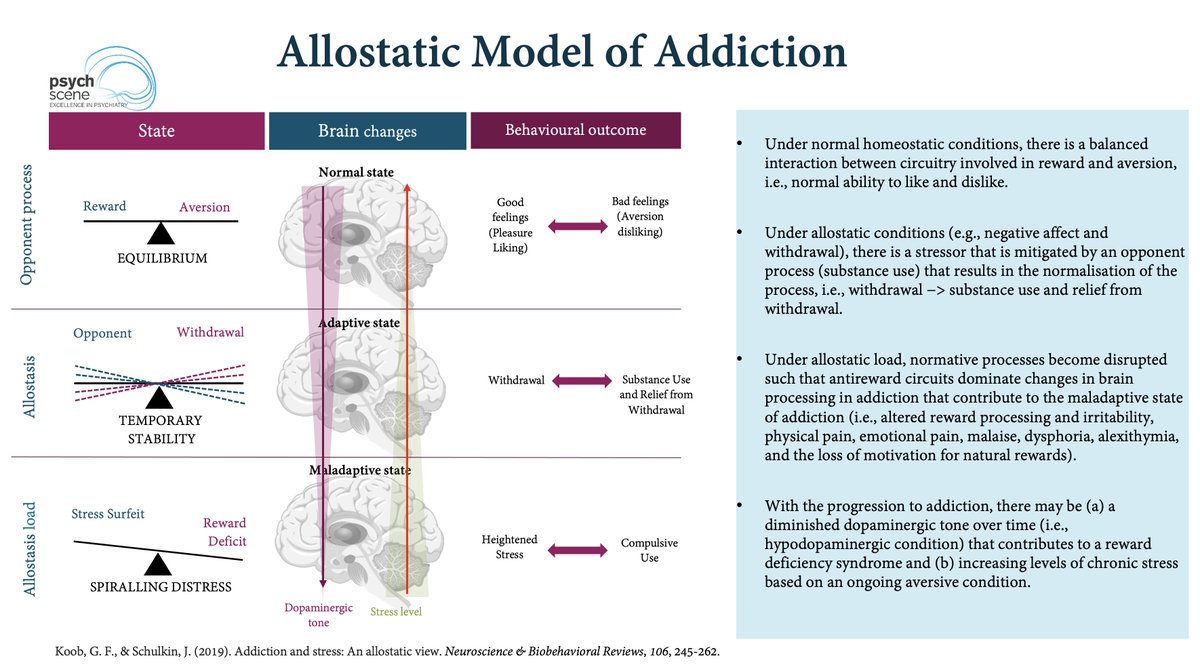
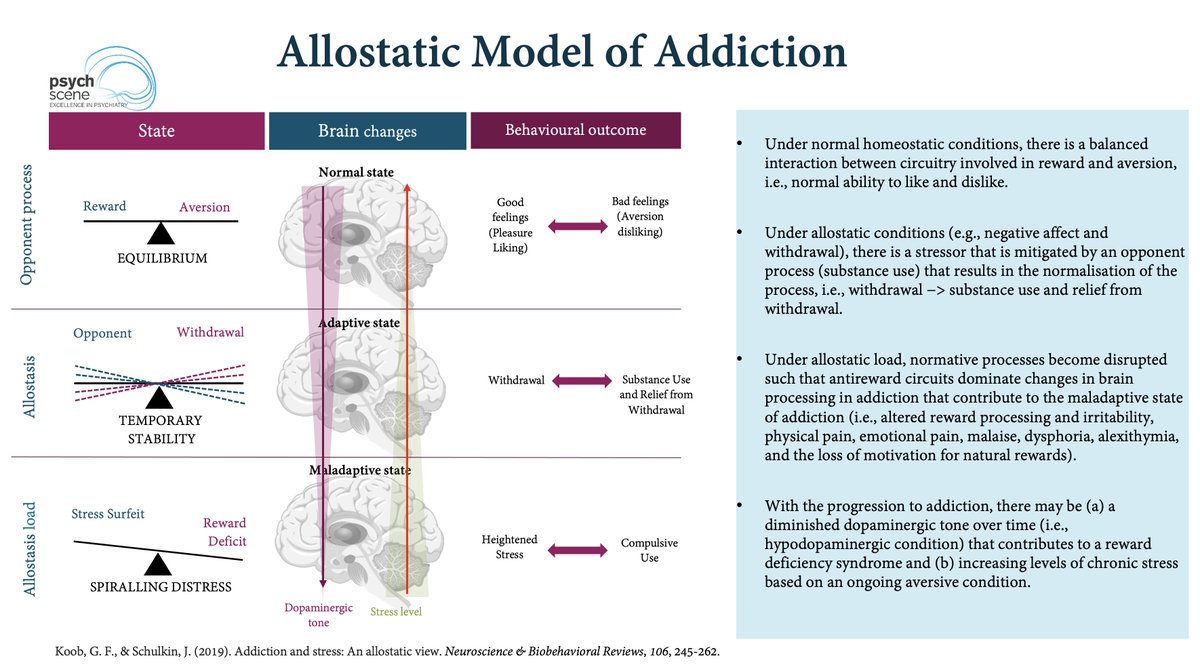 The shift from Anhedonia to Hyperkatifeia is driven by a "Between-System" neuroadaptation.
The shift from Anhedonia to Hyperkatifeia is driven by a "Between-System" neuroadaptation.
 1. Interpersonal Instability:
1. Interpersonal Instability: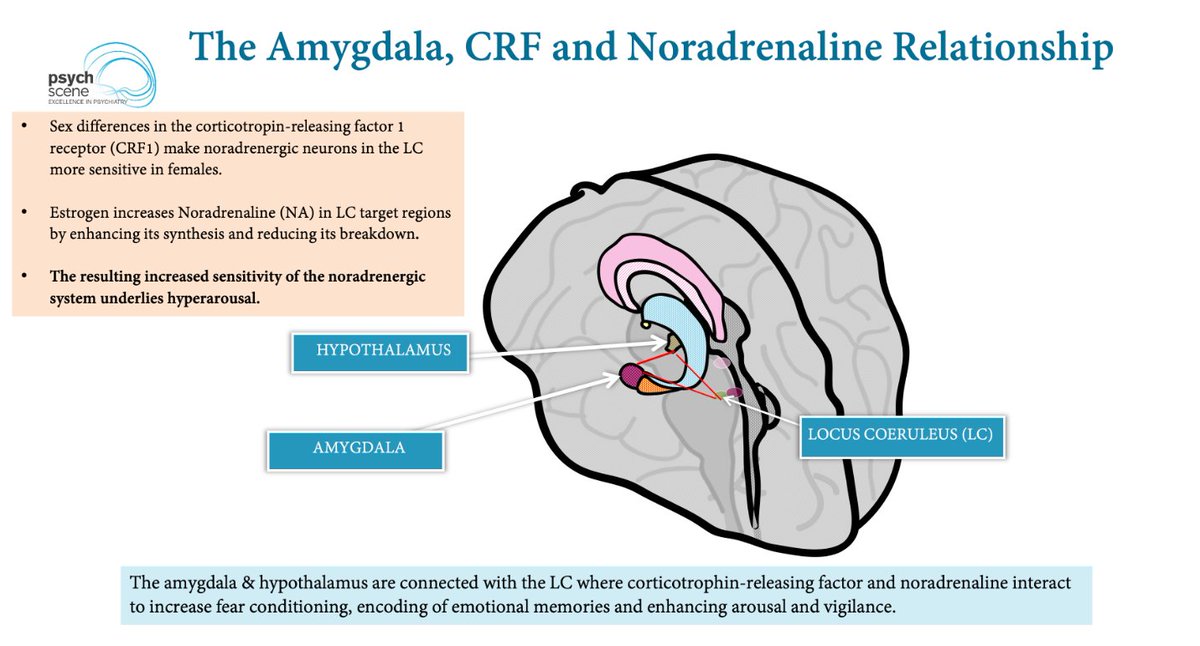
 Misdiagnosing BPD as BDII in women starts when "affective instability" is misinterpreted.
Misdiagnosing BPD as BDII in women starts when "affective instability" is misinterpreted.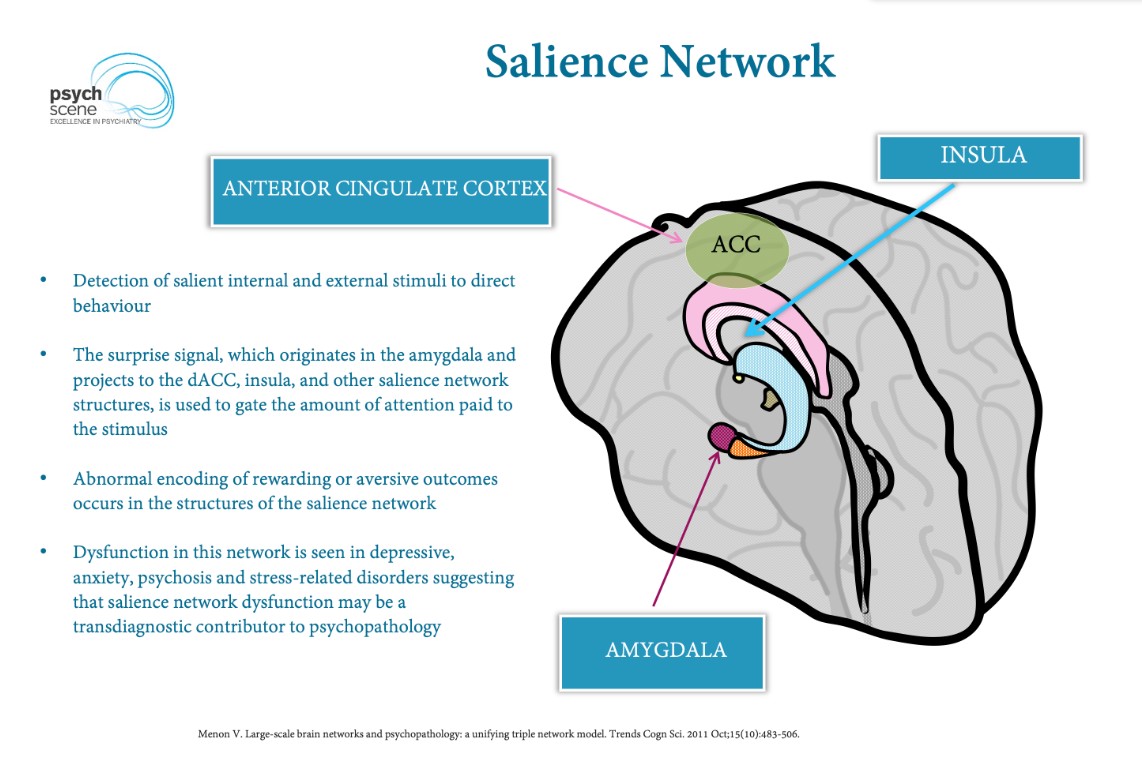
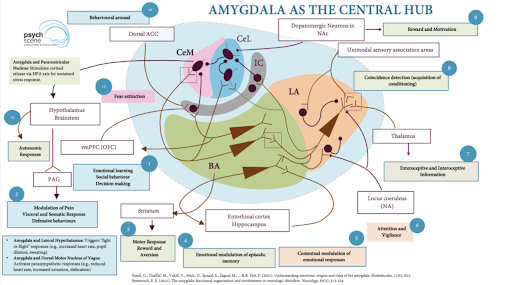
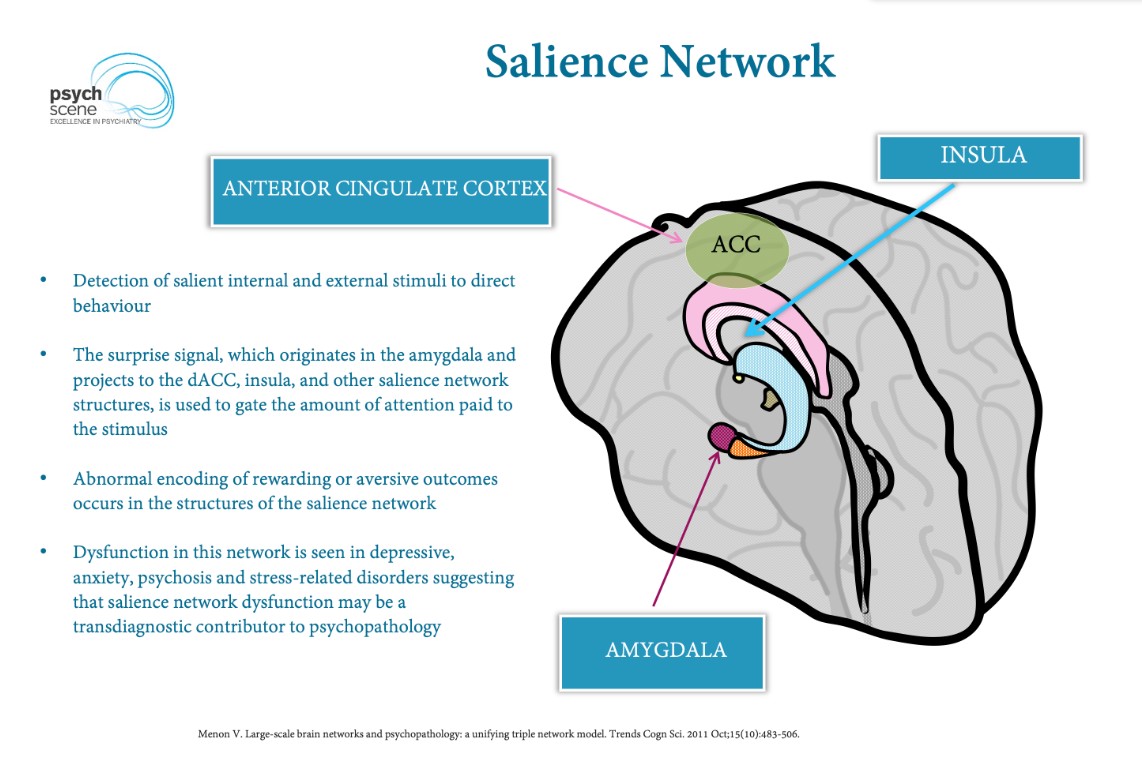 The Neural Substrate of “Emotion”
The Neural Substrate of “Emotion”
 The Connectivity Paradox
The Connectivity Paradox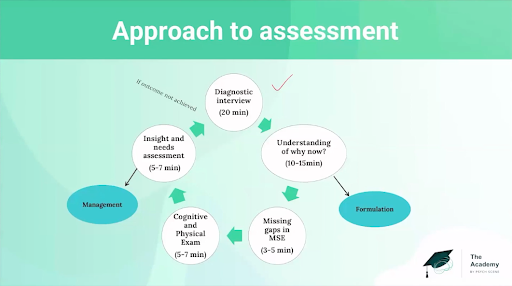
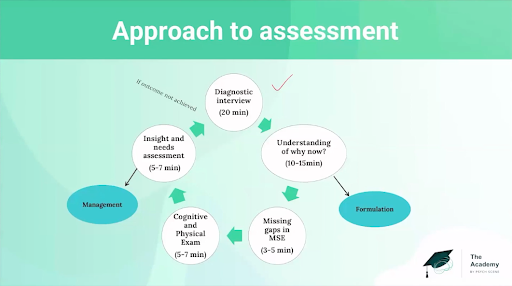 1. Formulation is not reflective writing, it is the architecture of care.
1. Formulation is not reflective writing, it is the architecture of care.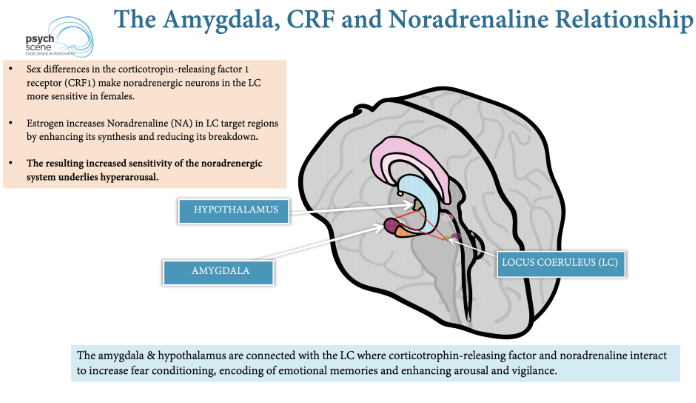
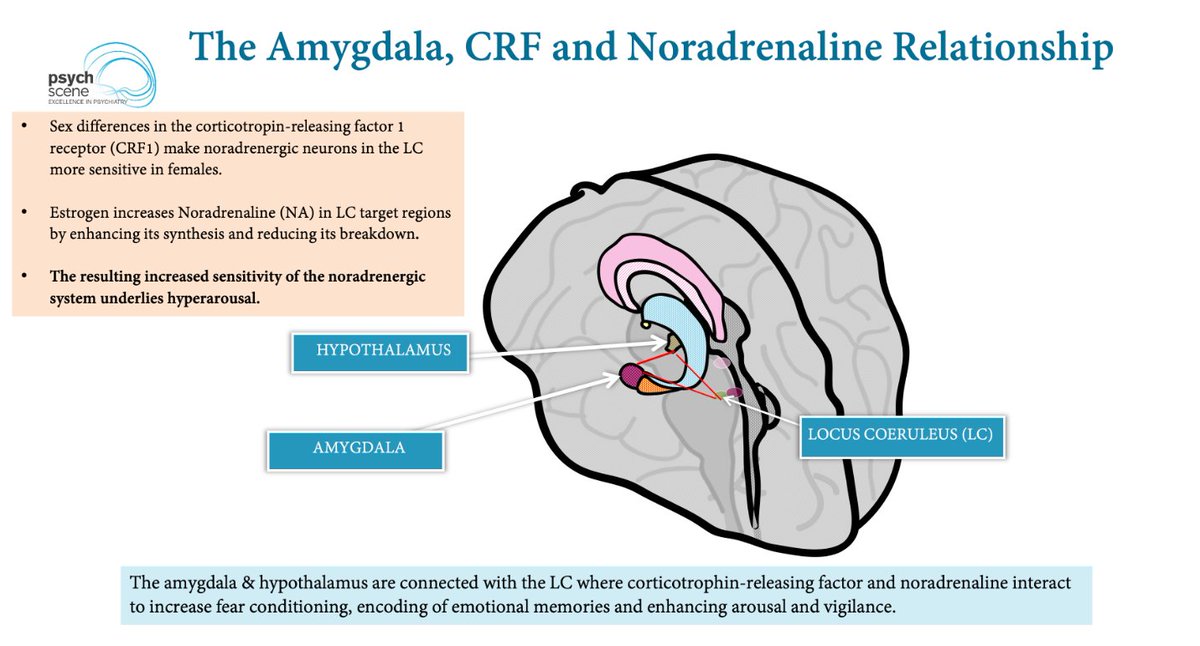
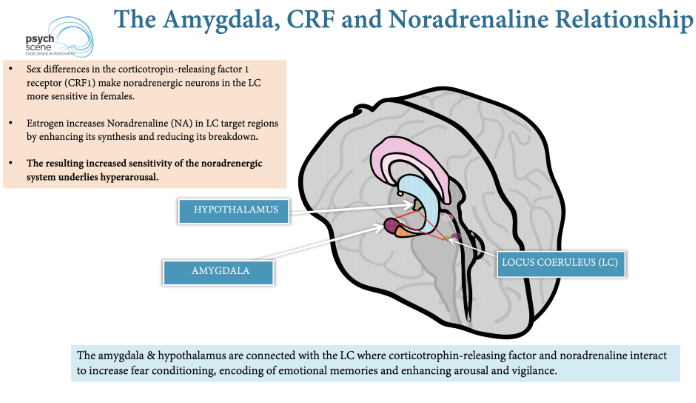 The Female CRF Substrate
The Female CRF Substrate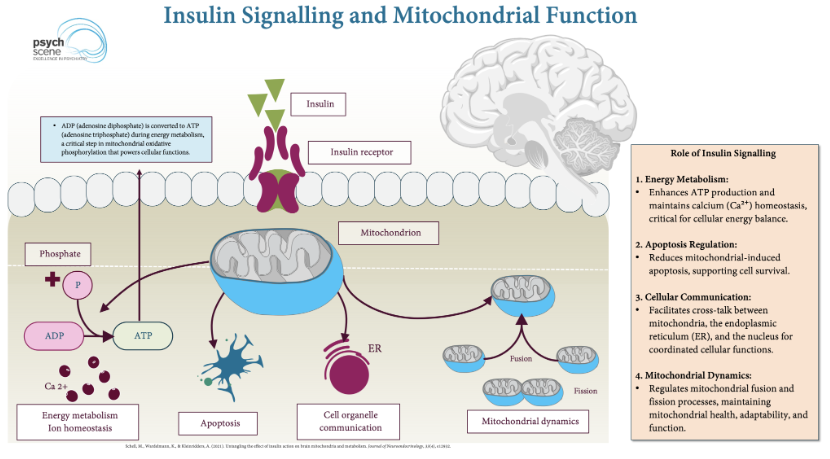
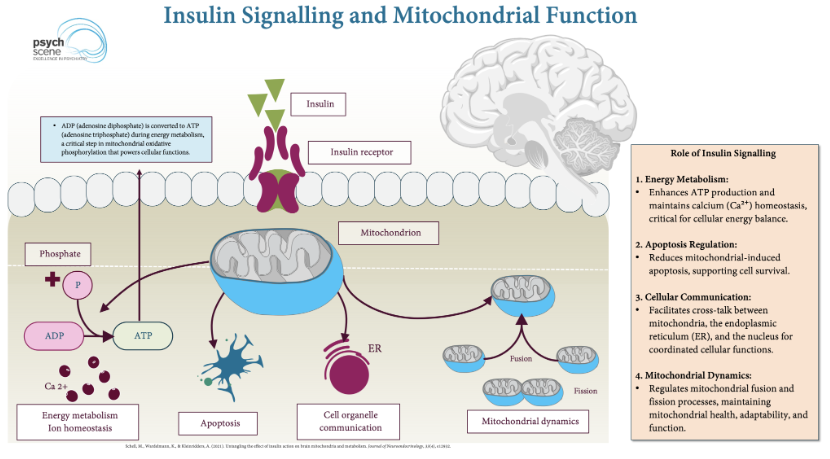 The brain is metabolically demanding.
The brain is metabolically demanding.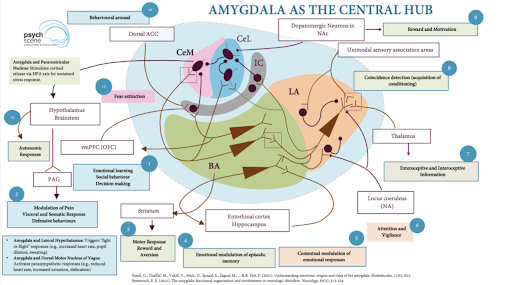
 Most people exposed to trauma do not develop PTSD.
Most people exposed to trauma do not develop PTSD.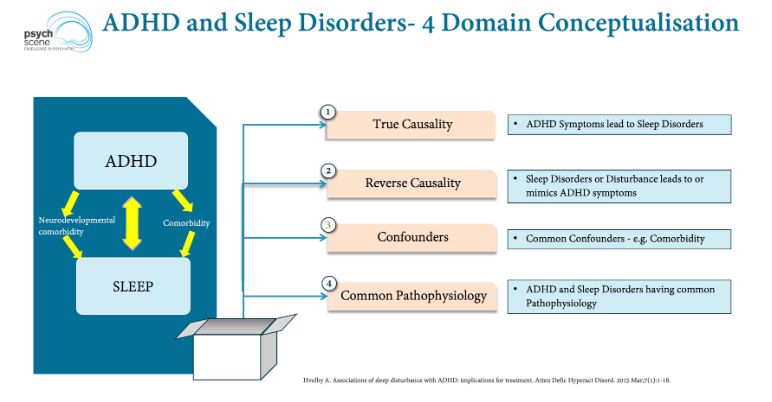
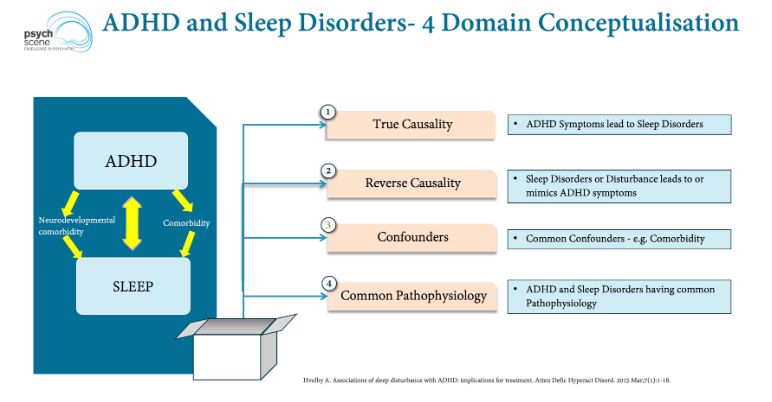 Some often assume sleep issues in ADHD—such as delayed onset, bedtime resistance, and irregular sleep-wake patterns—are "behavioural," the result of poor routine or bedtime procrastination.
Some often assume sleep issues in ADHD—such as delayed onset, bedtime resistance, and irregular sleep-wake patterns—are "behavioural," the result of poor routine or bedtime procrastination.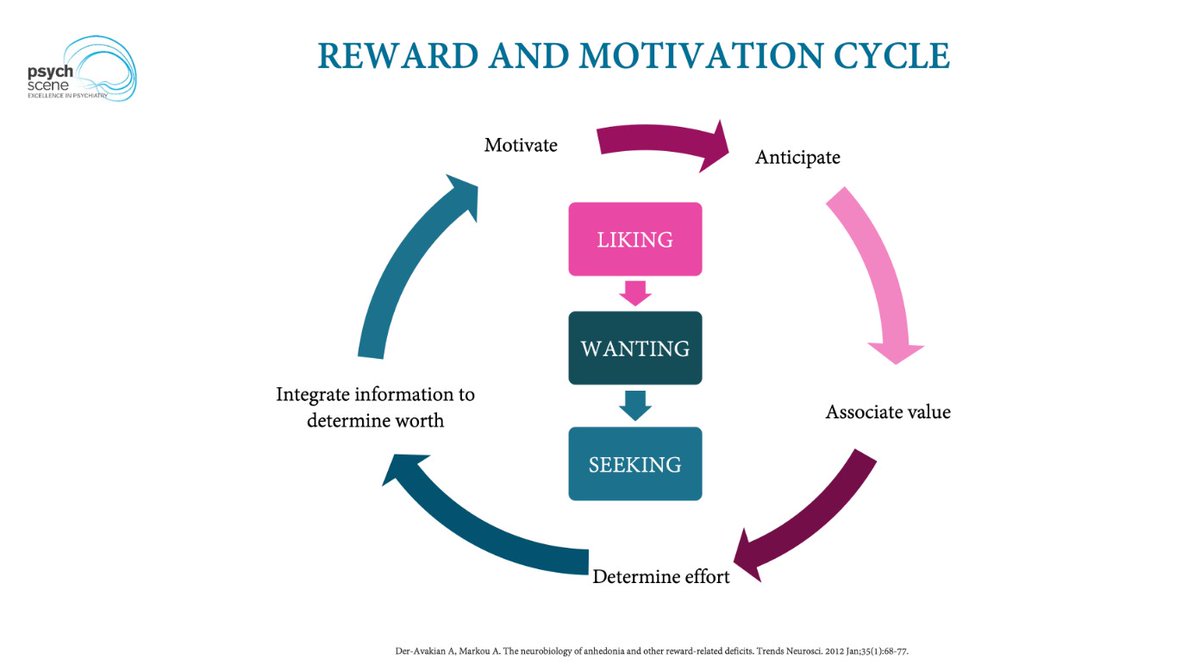
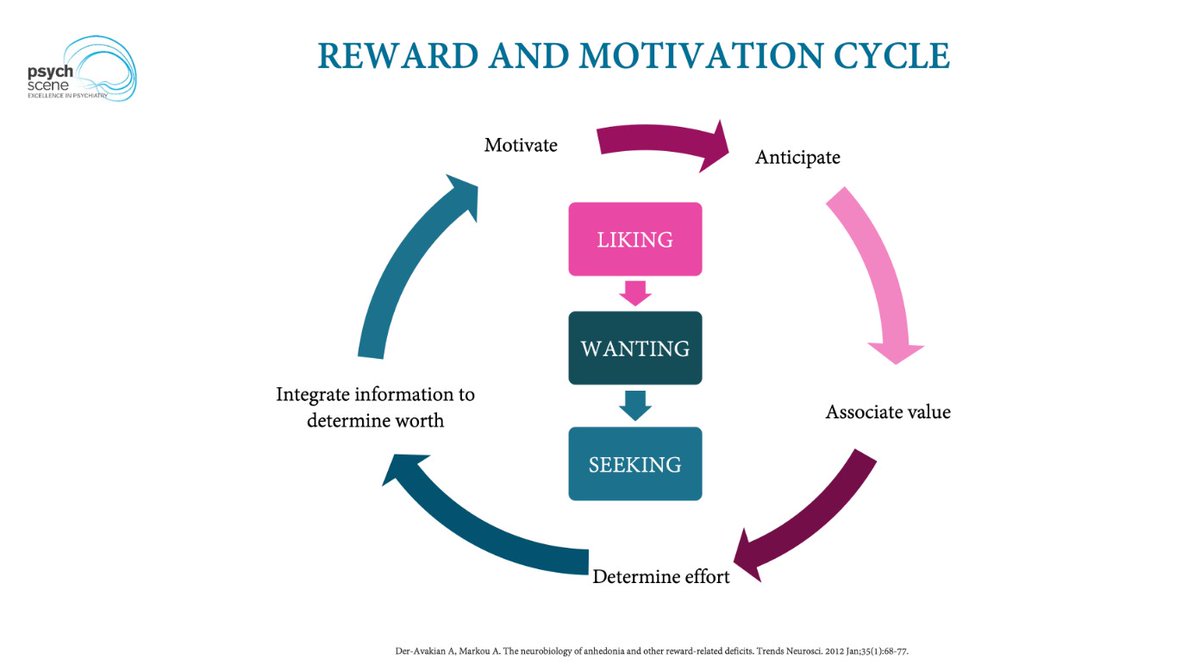 1) Reward Deficiency Syndrome (RDS) Theory
1) Reward Deficiency Syndrome (RDS) Theory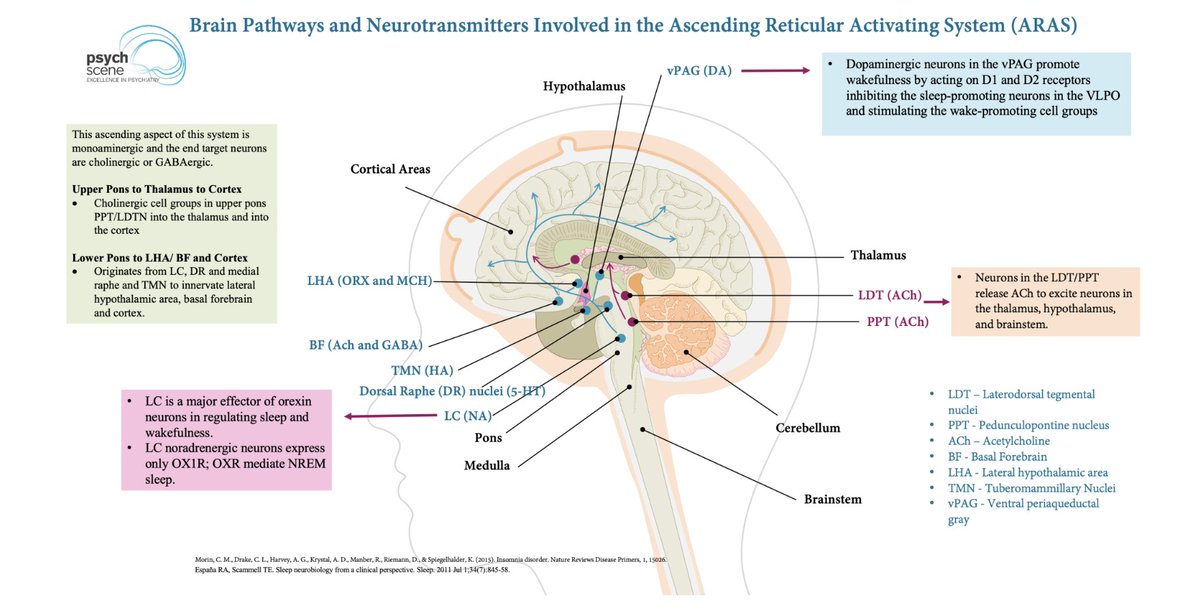
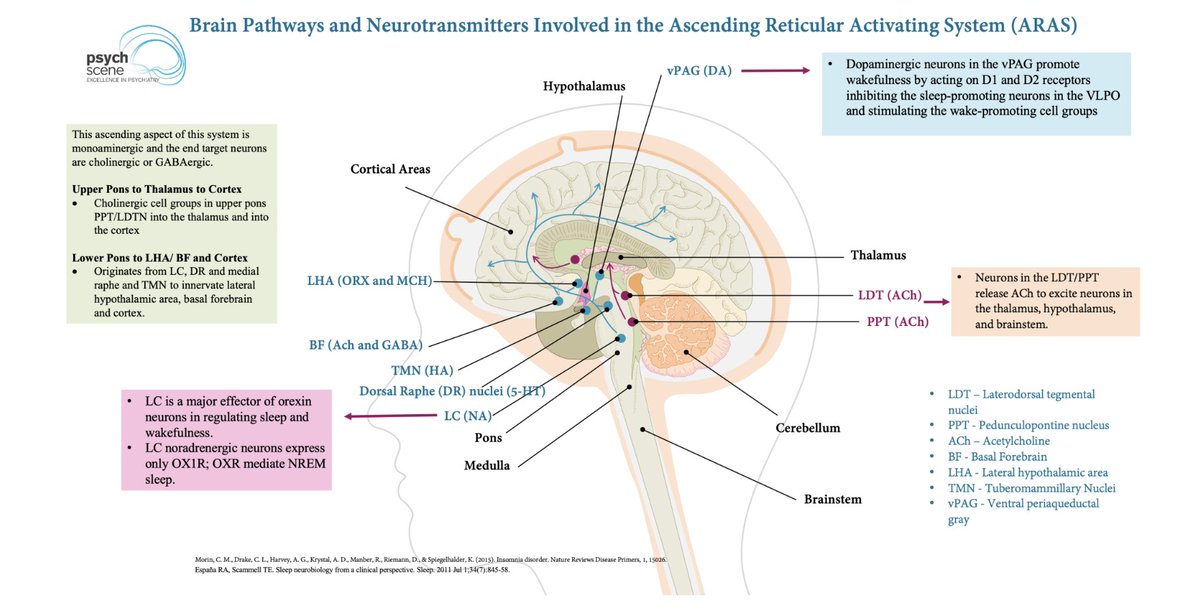 Consciousness has two separable components:
Consciousness has two separable components: