Why SARS-CoV-2 bounces back after #Paxlovid treatment
A NEW study found that the antiviral treatment, especially when given early in the course of the infection, can leave behind target cells that can still be infected with the virus. 1/
A NEW study found that the antiviral treatment, especially when given early in the course of the infection, can leave behind target cells that can still be infected with the virus. 1/

In addition, the treatment may not completely clear the virus, leaving behind infectious particles that invade the target cells. 2/
If at the end of 5 days of treatment, there's still virus and target cells around, then the infection can basically restart. Though the antiviral stops existing viruses from replicating, it doesn't remove the viral particles or the infected cells. 3/ 

Paxlovid, an antiviral combination of nirmatrelvir and ritonavir, is beneficial for mild COVID-19 symptoms with a high hospitalization risk. The virus returns in some patients, who may develop more symptoms and spread the illness. 4/
To better understand the underlying mechanism, researchers used a mathematical model to analyze changes in the viral load of 51 patients, all treated with nirmatrelvir-ritonavir and 20 of whom experienced a rebound case. 5/
The model incorporated what researchers knew about how the viral load changed over the course of an infection. The amount of virus grows rapidly at first and peaks after 3 or 4 days, which is when symptoms become apparent. 6/
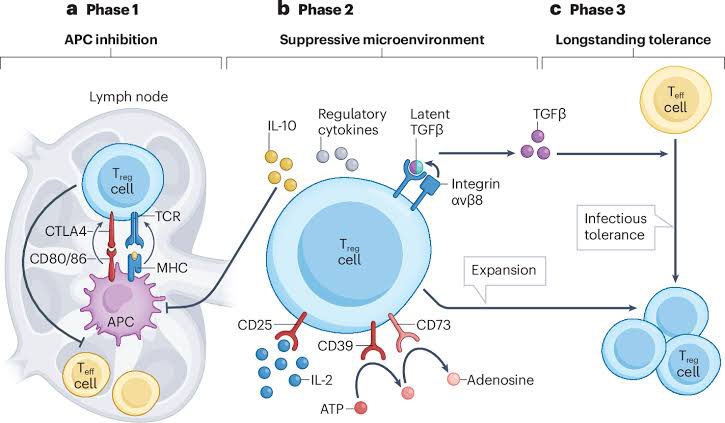
Cells respond by secreting interferons that interferes with infection. Over first week, the adaptive immune system responds by producing antibodies that coat the virus & prevent spreading & infection. The real cleaning up of the virus is done by the adaptive immune response 7/ 

When they added patient data about the antiviral treatment to the model, they observed that the dynamics changed. While the remaining virus could no longer replicate, it could still infect cells that hadn't been killed by the virus or were not protected by interferon. 8/ 

Notably, starting antiviral treatment earlier preserved more target cells, which increased the likelihood of a rebound after treatment was stopped. 9/
Patients take antiviral treatment for 5 days as the standard of care. The new study suggests that a 10-day course may more effectively reduce a person's risk of a rebound. That duration may give the body enough time to develop a robust immune response. 10/ 

• • •
Missing some Tweet in this thread? You can try to
force a refresh