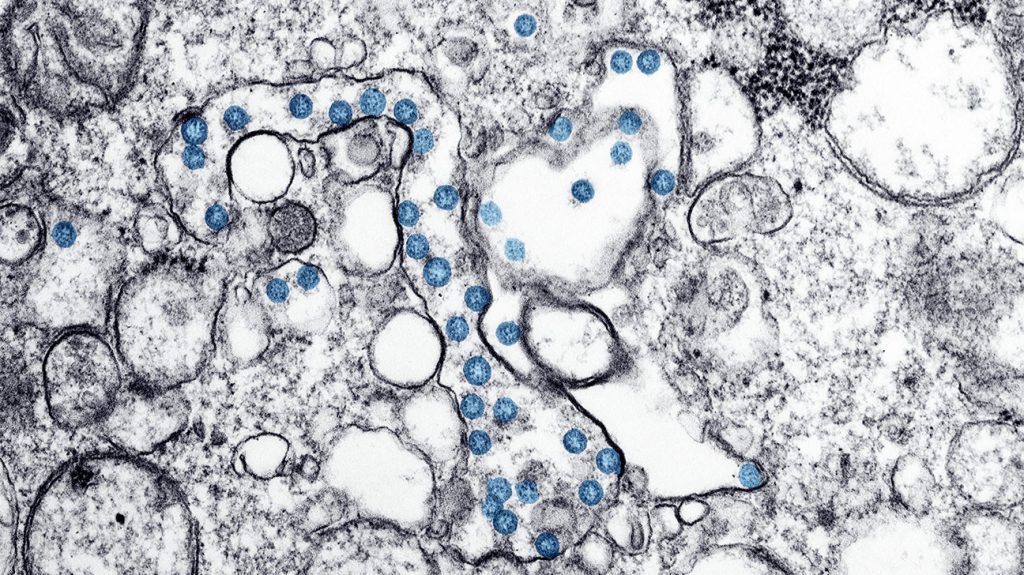
Even after 5 yrs since its arrival, SARS-CoV-2 mutations keep emerging. A new variant LP.8.1 is rising. Almost 1 in 5 COVID cases in New South Wales are it. In the UK, it accounts for at least 3 in 5 cases. Just what is LP.8.1? Is it worrying? 1/ 

LP.8.1 was first detected in July 2024. It’s a descendant of Omicron, specifically of KP.1.1.3, which is descended from JN.1, a subvariant that caused large waves of COVID infections around the world in late 2023 and early 2024. 2/ 

The WHO designated LP.8.1 as a variant under monitoring in January. This was in response to its significant growth globally, and reflects that it has genetic changes which may allow the virus to spread more easily and pose a greater risk to human health. 3/ 

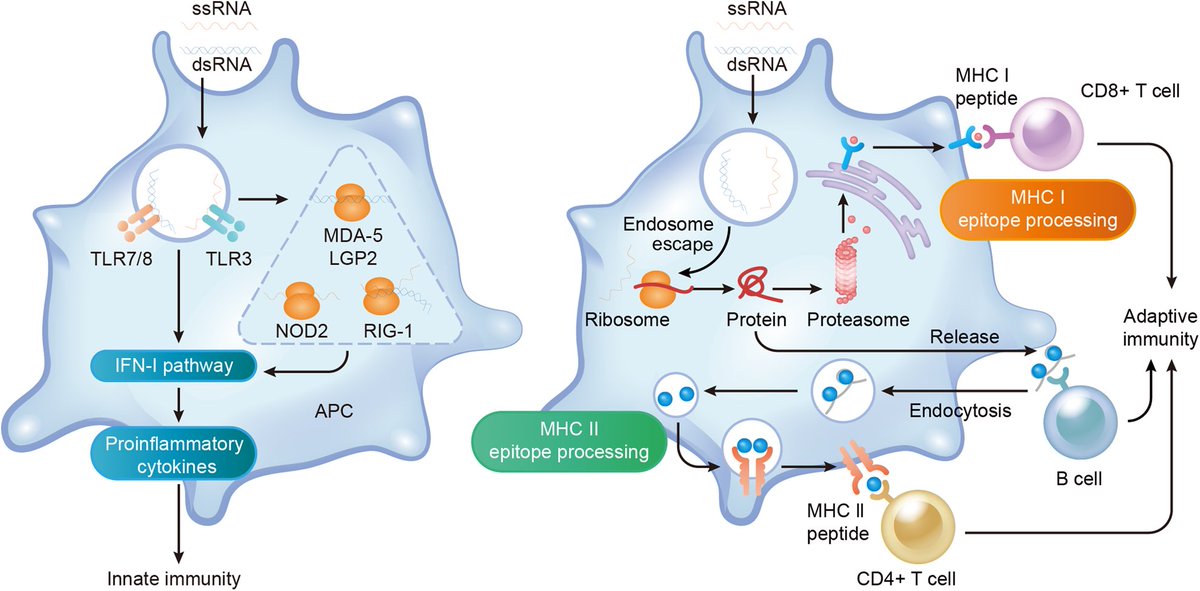
SARS-CoV-2 attaches to our cells via its spike protein, which LP.8.1 has six mutations in. One mutation, V445R, may let this variant spread faster than others. Lab tests demonstrate V445R increases lung cell binding. 4/ 
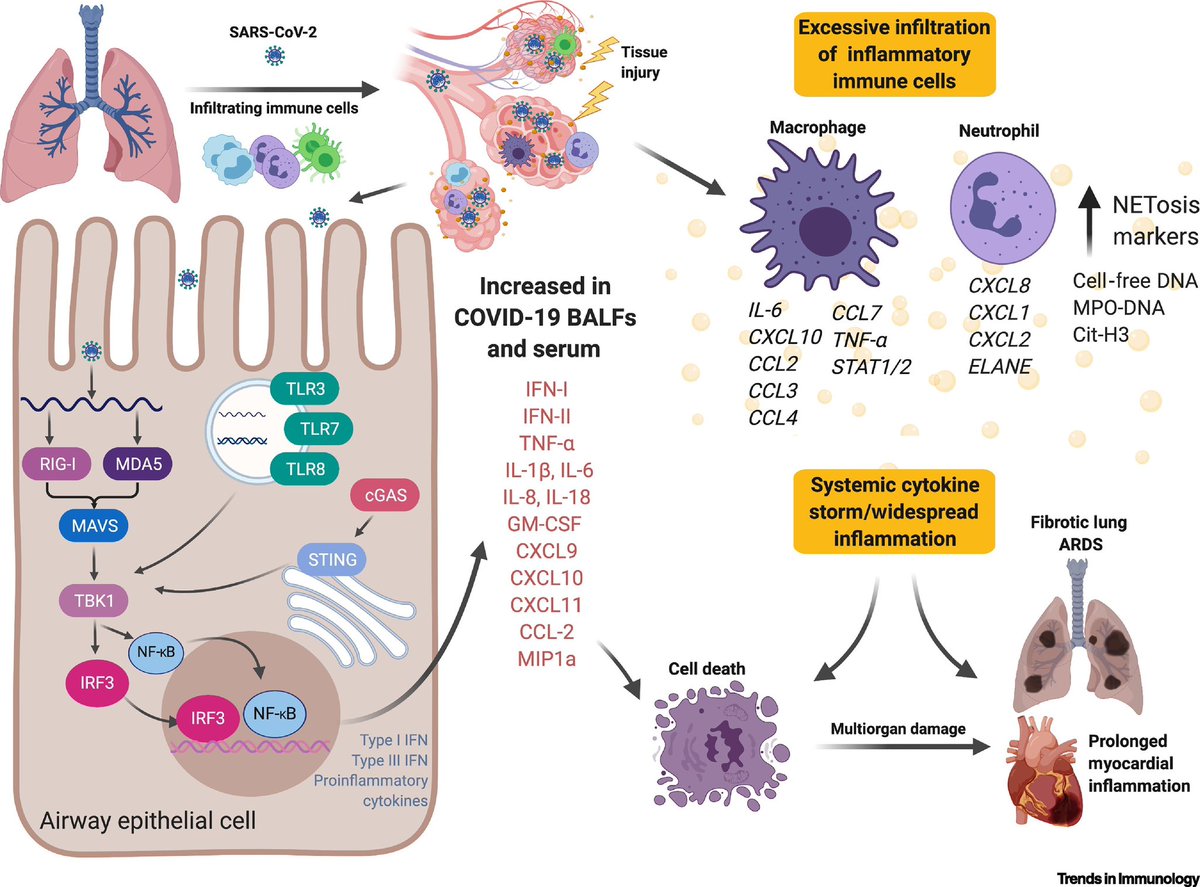
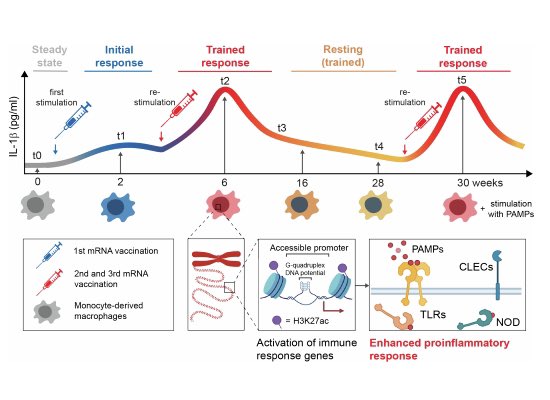
Notably, the symptoms of LP.8.1 don’t appear to be any more severe than other circulating strains. Current COVID vaccines, including the most recently available JN.1 shots, are still expected to offer good protection against symptomatic and severe disease with LP.8.1. 5/
That doesn’t mean cases won’t rise!
COVID remains a global health threat. Australia has had over 45,000 new cases this year, with 260 people in hospitals. Because many people no longer test or report infections, the true figure is likely far higher. 6/
COVID remains a global health threat. Australia has had over 45,000 new cases this year, with 260 people in hospitals. Because many people no longer test or report infections, the true figure is likely far higher. 6/
Since the LP.8.1 variety is under monitoring, WHO member countries will continue to investigate its behavior, particularly its ability to circumvent human immunity. 7/
While LP.8.1 variant isn't a cause for concern, COVID can still be severe for individuals. Vigilance and vaccination, especially for medically susceptible groups, are crucial to minimizing illness effect. 8/8
thelancet.com/journals/lanin…
thelancet.com/journals/lanin…
• • •
Missing some Tweet in this thread? You can try to
force a refresh