The state of Louisiana has managed to reduce its Hepatitis C death rate by nearly a sixth in just a few years through a clever public health program🧵 

Louisiana's success has to do with the recent development of a miraculous change in how Hepatitis C (HCV) is treated.
Prior to 2013, HCV was primarily treated with drugs like interferon and ribavirin, but the drugs were not consistently effective at clearing the virus.
Prior to 2013, HCV was primarily treated with drugs like interferon and ribavirin, but the drugs were not consistently effective at clearing the virus.

But then the FDA approved the first direct-acting antiviral (DAA), sofosbuvir, a liver-targeting NS5B protein inhibitor that, combined with another protein inhibitor (velpatasvir), is effective in treating 95-99% of HCV patients.
That's basically everyone!
That's basically everyone!

A few more DAAs have come out since then, but they all share an annoying problem: They're expensive.
It would cost over $300 billion to treat every HCV-positive person in the U.S. That's a very large share of the budget of Medicaid, so it's not really feasible.
It would cost over $300 billion to treat every HCV-positive person in the U.S. That's a very large share of the budget of Medicaid, so it's not really feasible.
But Louisiana figured out how to make it feasible.
Where other states negotiate with multiple drug producers at once, Louisiana negotiated with just one company to give them the state's full $30m, if they provided unrestricted medication access
Asegua Therapeutics took the deal
Where other states negotiate with multiple drug producers at once, Louisiana negotiated with just one company to give them the state's full $30m, if they provided unrestricted medication access
Asegua Therapeutics took the deal
Being the sole supplier for an unlimited amount might seem like it would be bad for the company, but their prices are far from costs, and they were actually likely to get far higher returns this way than if they had been one of six suppliers.
So the marginal cost fell to zero.
So the marginal cost fell to zero.
Louisiana had a goal of curing at least 10,000 Medicaid-enrolled and incarcerated persons by 2020 and to screen and identify 90% of HCV patients, with 80% cured, by 2024.
With that in mind, the state started diagnosing people left-and-right, immediately:
With that in mind, the state started diagnosing people left-and-right, immediately:

Louisiana also rapidly increased prescriptions for Epclusa, the generic drug they had made a contract for to get whatever amount they wanted. 

In this effort, Louisiana showed out.
The state went from below-average prescription numbers to beating the national average handily.
The state went from below-average prescription numbers to beating the national average handily.

Given this clear increase in diagnoses, prescriptions, and so on, you can guess that a lot of the graphs look similar.
And they do!
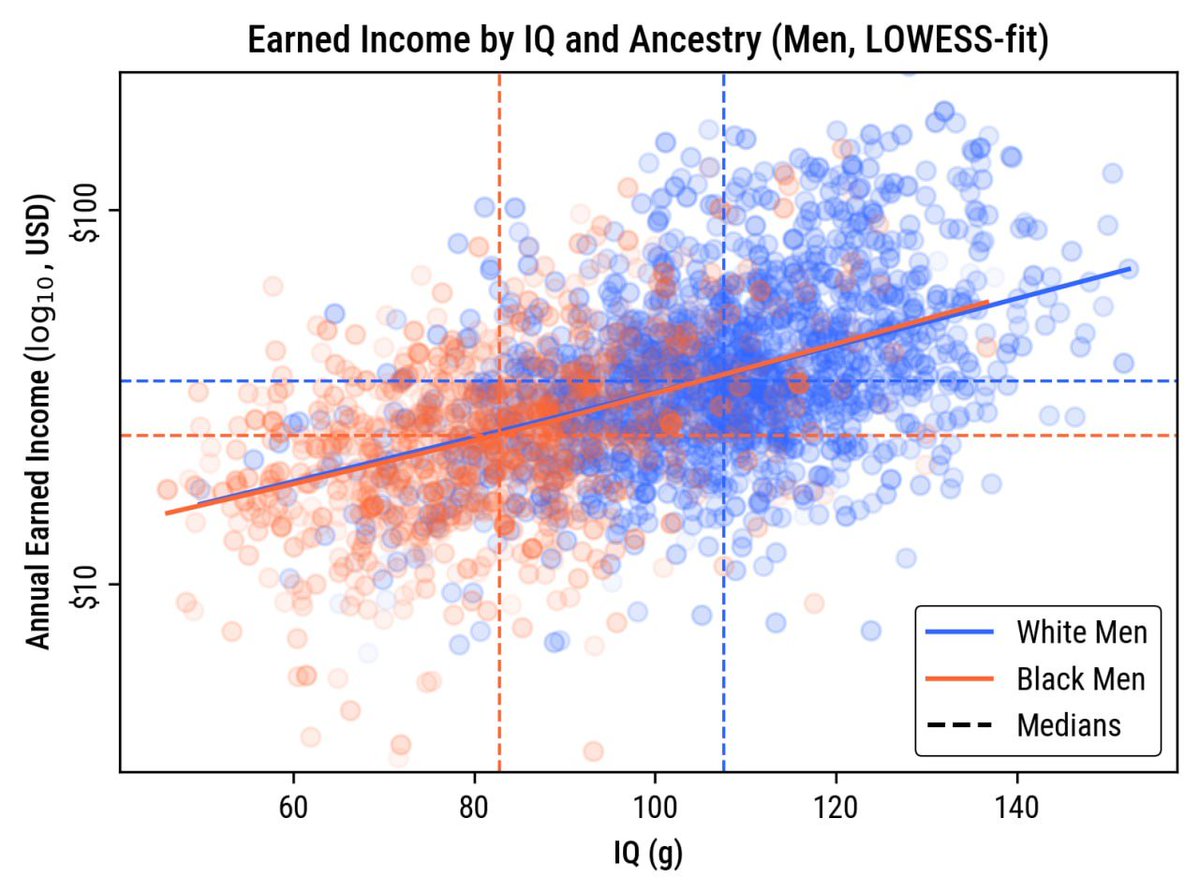
In this image, you can see HCV deaths falling straight away via event-study:
And they do!
In this image, you can see HCV deaths falling straight away via event-study:
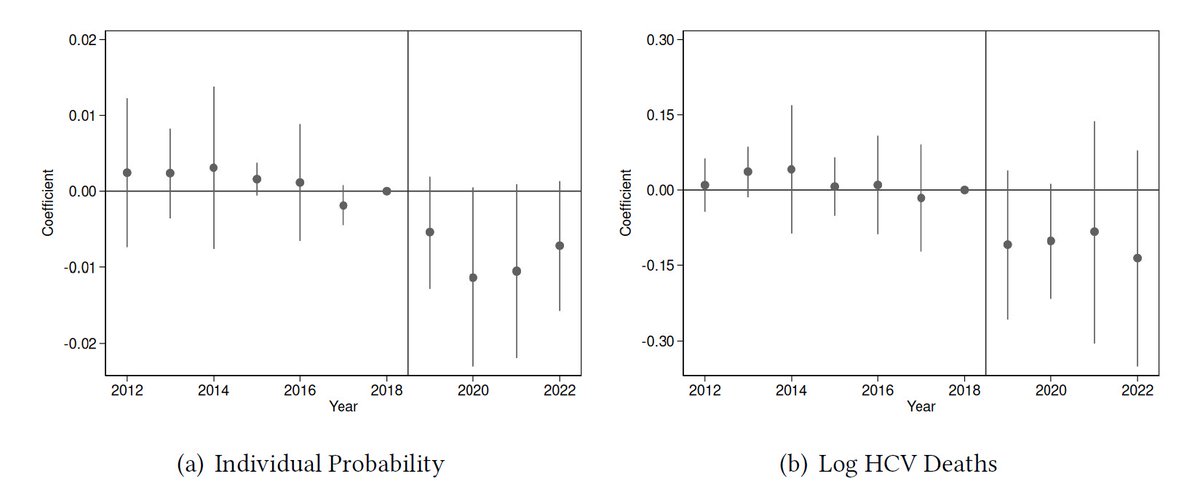
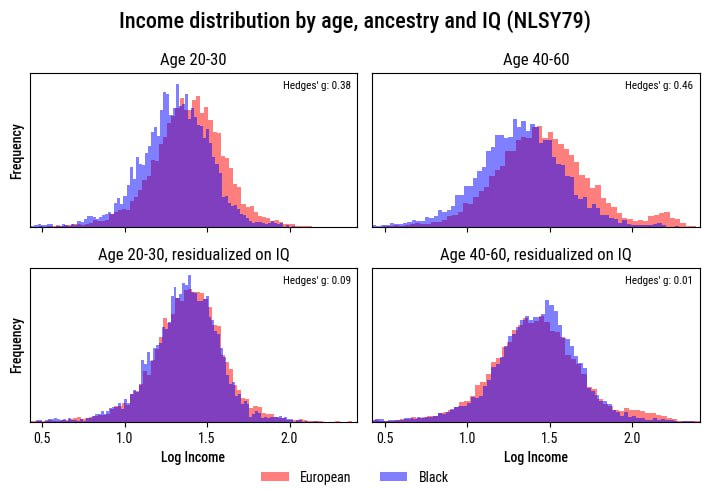
And in this, you can see a knock-on consequence: the number of people in need of liver transplants fell.
Moreover, they started being in better condition, enjoying better-functioning livers while they were seeking a new one.
Moreover, they started being in better condition, enjoying better-functioning livers while they were seeking a new one.

Before continuing: Everything shown here holds up whether using synthetic controls or an event-study.
This is a really impressive study, and it's showing some credible and important results.
This is a really impressive study, and it's showing some credible and important results.

So, let me recap.
Louisiana negotiated an exclusive deal to have the state provide certain very at-risk populations with essential drugs on the cheap.
This worked amazingly: they saved lives, they helped clear their transplant backlogs, and they might've done more.
Louisiana negotiated an exclusive deal to have the state provide certain very at-risk populations with essential drugs on the cheap.
This worked amazingly: they saved lives, they helped clear their transplant backlogs, and they might've done more.
Hepatitis C is variable. Sometimes it takes a short while to show symptoms, sometimes it takes decades
By curing so many people, Louisiana might've cut down on future transmission, saving more money than expected
Oh, and already, this program more than paid for itself!
By curing so many people, Louisiana might've cut down on future transmission, saving more money than expected
Oh, and already, this program more than paid for itself!
I highly recommend giving this study a read. In my opinion, it gives a solid vision for future, affordable public health initiatives that can easily pay for themselves, like Louisiana's effort to eliminate Hepatitis C.
Sources:
nature.com/articles/natur…
nber.org/papers/w33617
Sources:
nature.com/articles/natur…
nber.org/papers/w33617
• • •
Missing some Tweet in this thread? You can try to
force a refresh