A potent Covid-19 vaccine in the making!
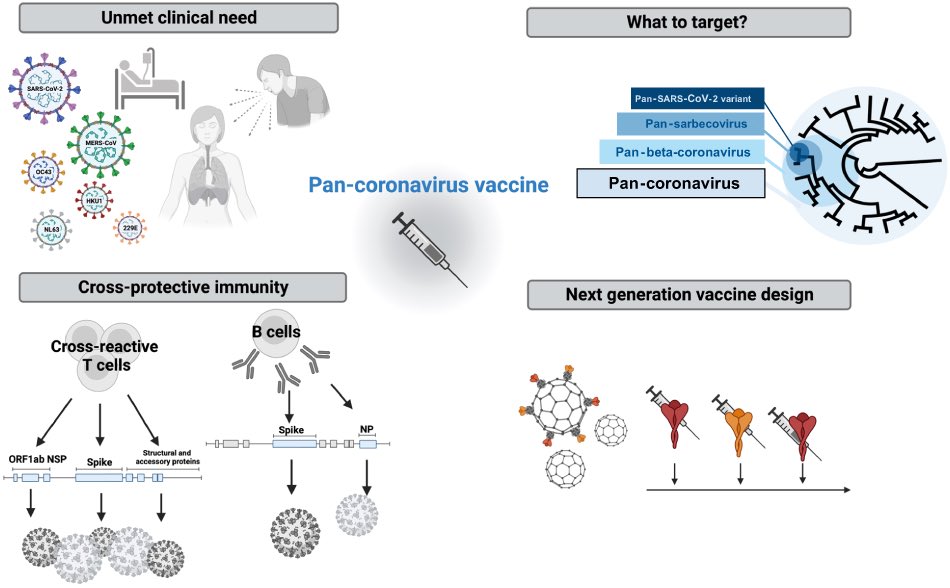
The RBD of the SARS-CoV-2 spike protein often mutates to help it evade immunity.
➡️ A modified COVID vaccine (SΔRBD) lacking the spike’s RBD showed strong lung protection, even better than mRNA vaccine in macaques. 1/
The RBD of the SARS-CoV-2 spike protein often mutates to help it evade immunity.
➡️ A modified COVID vaccine (SΔRBD) lacking the spike’s RBD showed strong lung protection, even better than mRNA vaccine in macaques. 1/
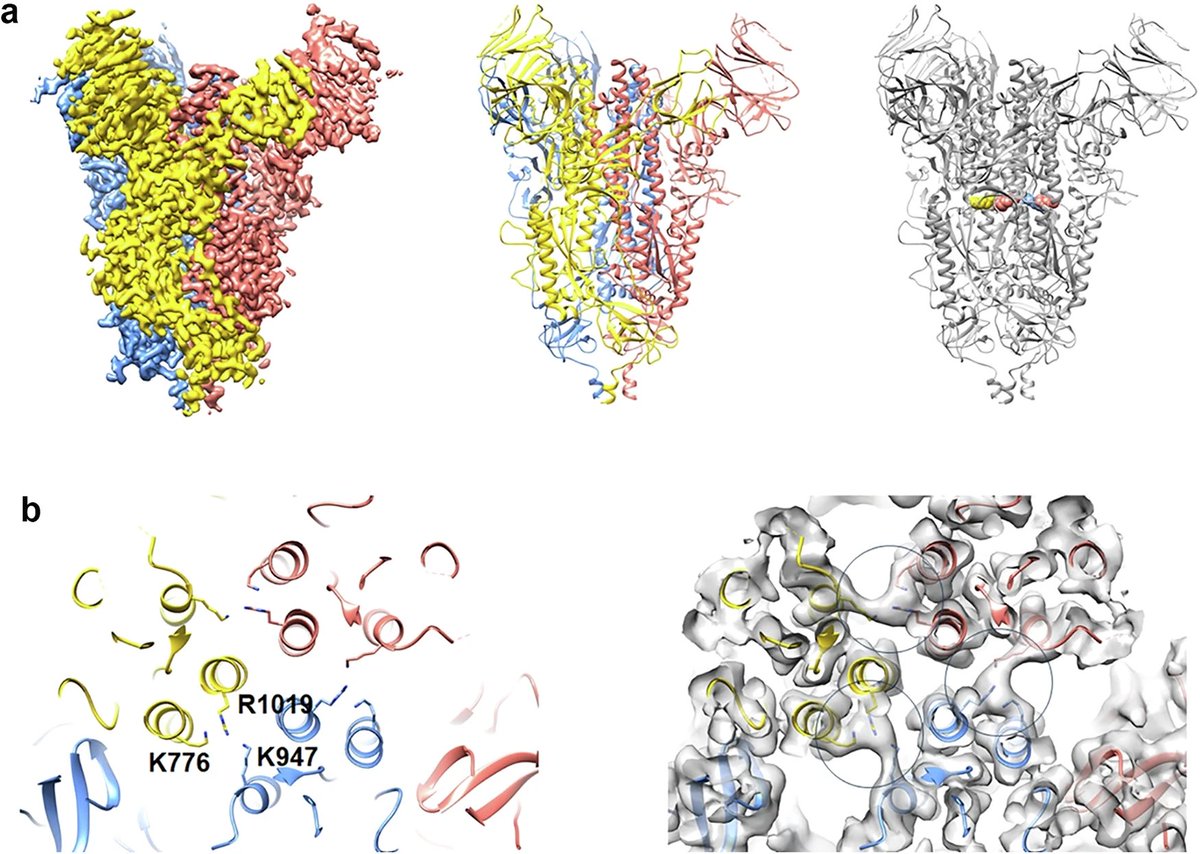
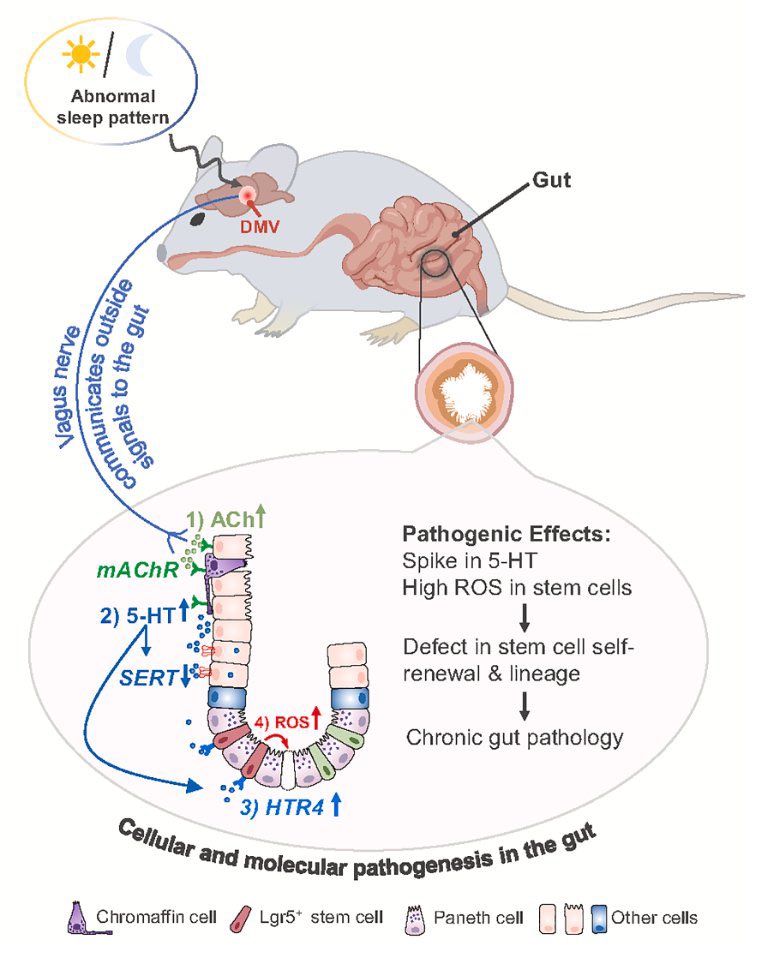
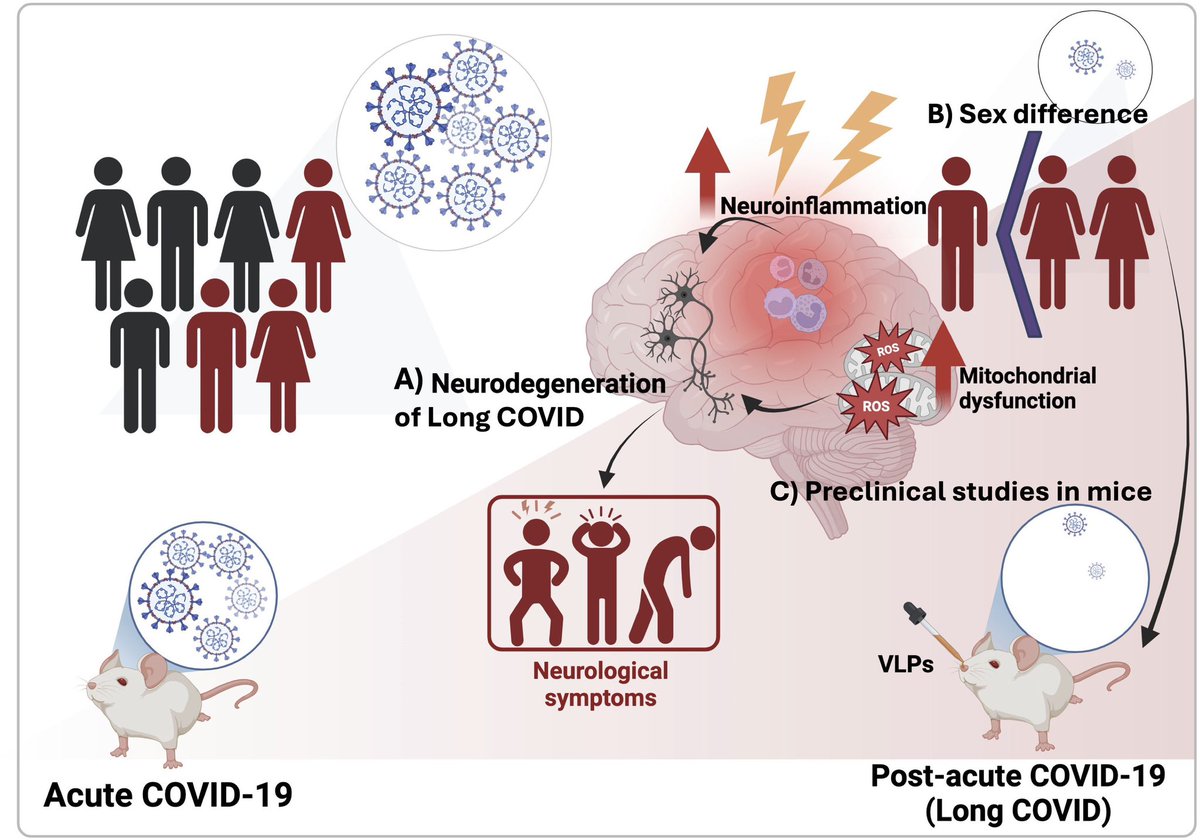
In order to steer the immune response away from RBD epitopes to more conserved domains, researchers generated S glycoprotein trimers without RBD and stabilized them by formaldehyde cross-linking. 2/ 
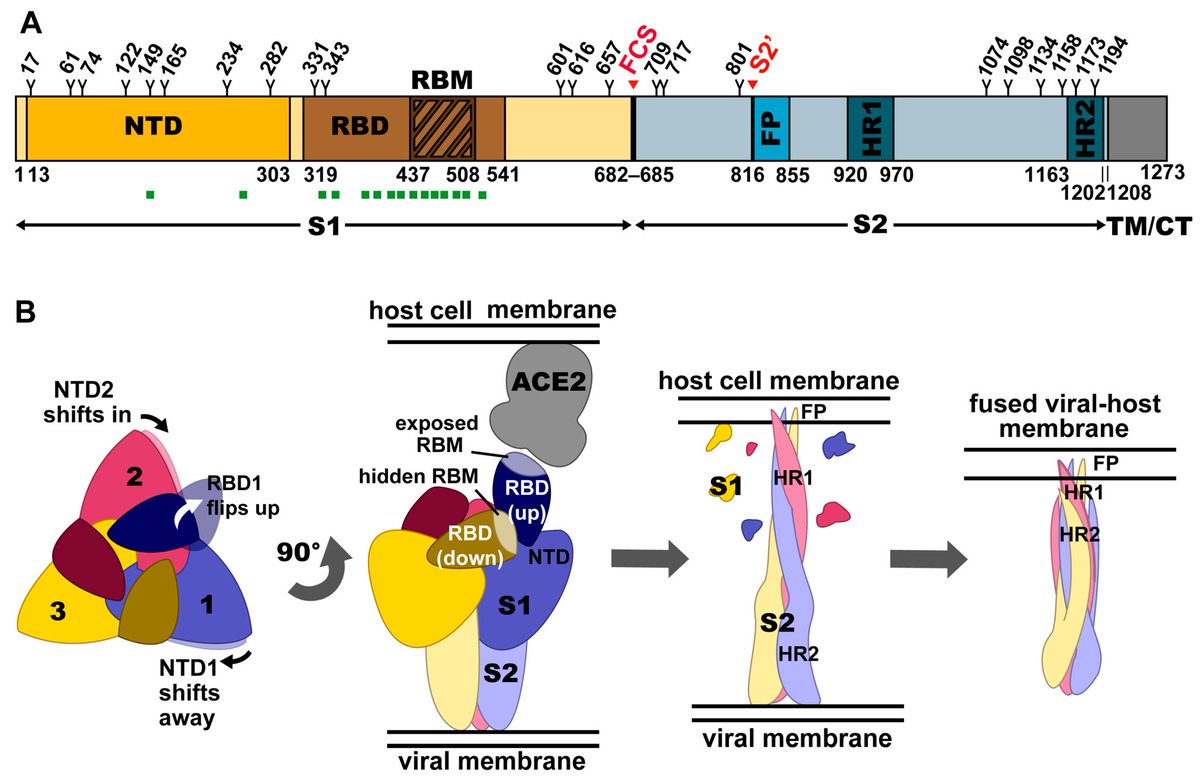
The cryoEM structure demonstrated, SΔRBD folds into native prefusion conformation, stabilized by one specific cross-link between S2 protomers.
SΔRBD was coated onto lipid vesicles, to produce synthetic virus-like particles & utilized in a heterologous prime-boost strategy 3/
SΔRBD was coated onto lipid vesicles, to produce synthetic virus-like particles & utilized in a heterologous prime-boost strategy 3/
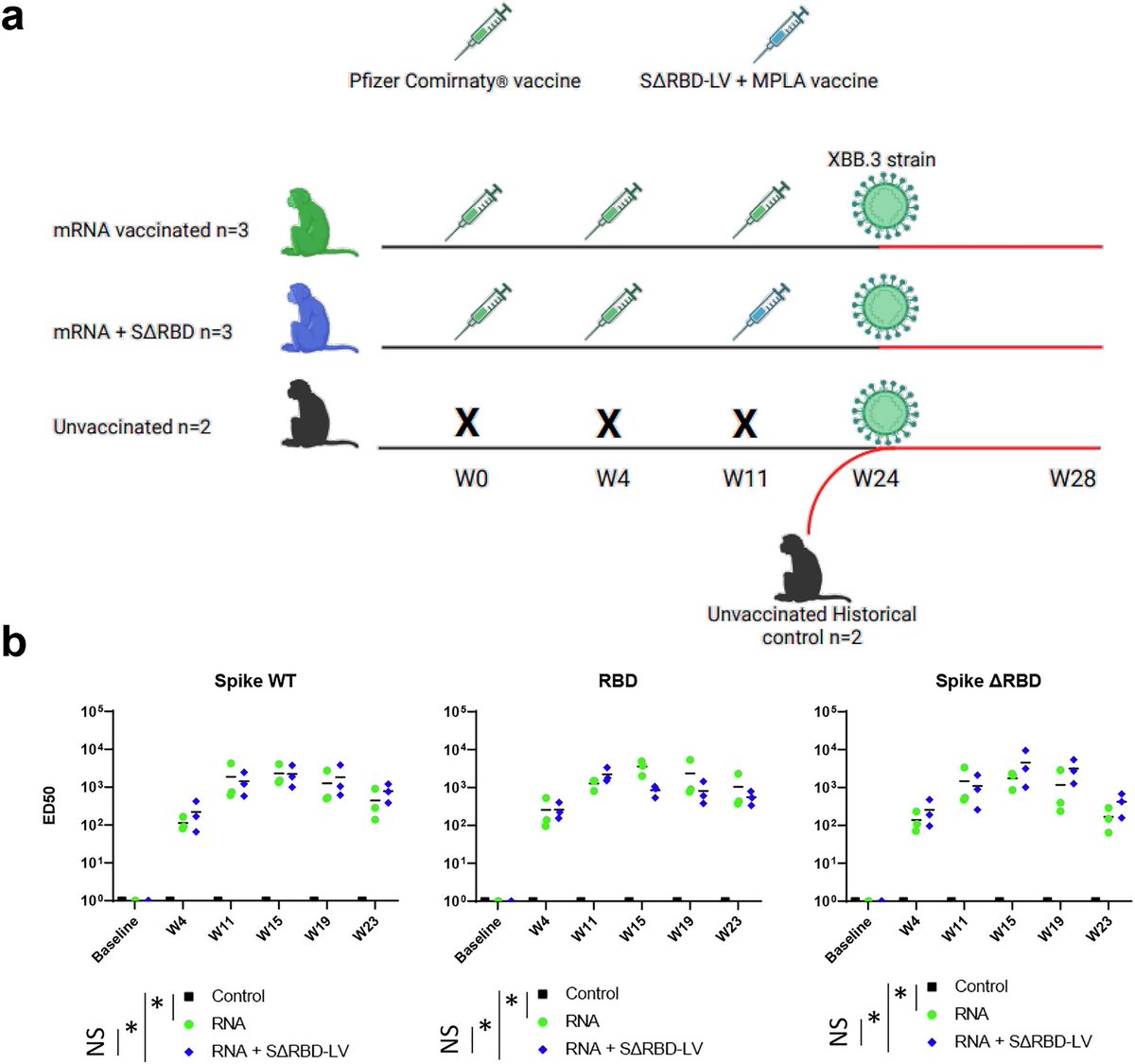
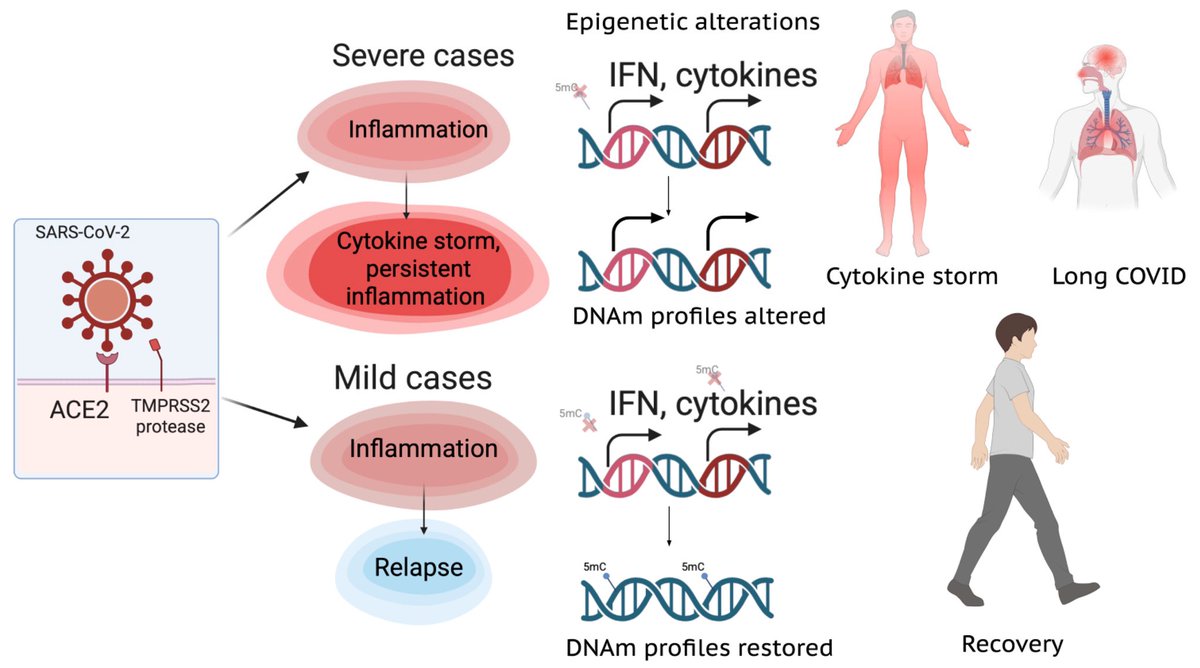
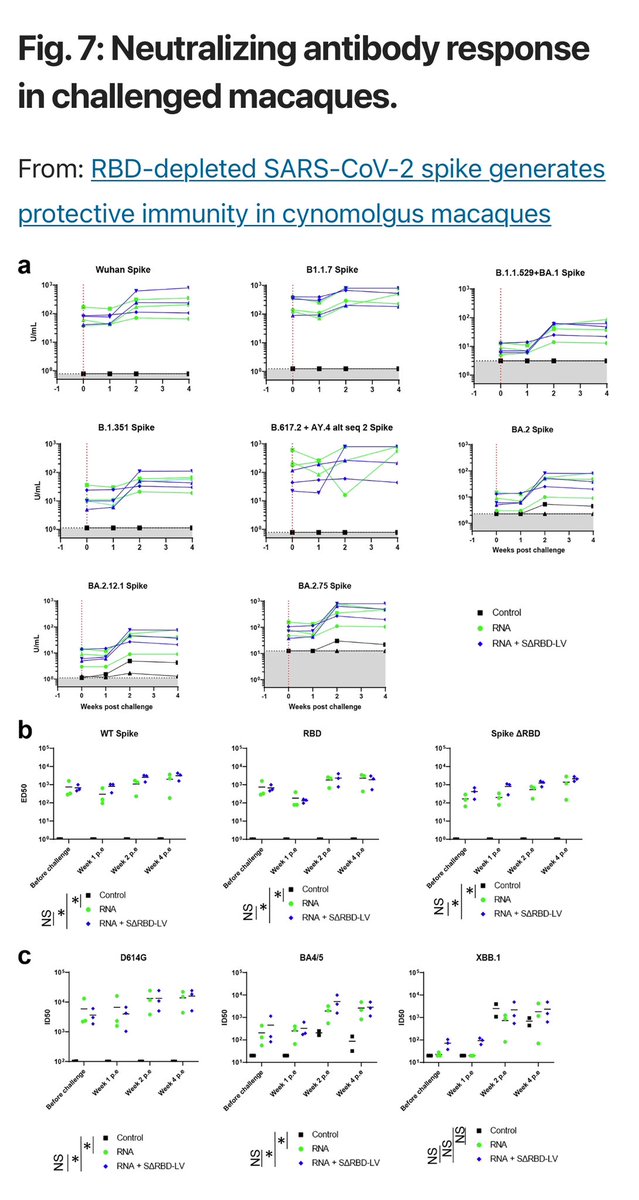
Immunization of cynomolgus macaques either 3 times with the Pfizer mRNA vaccine or 2 times followed by SΔRBD-LV showed that the SΔRBD-LV boost induced similar antibody titers and neutralization of different variants, including omicron. 4/ 
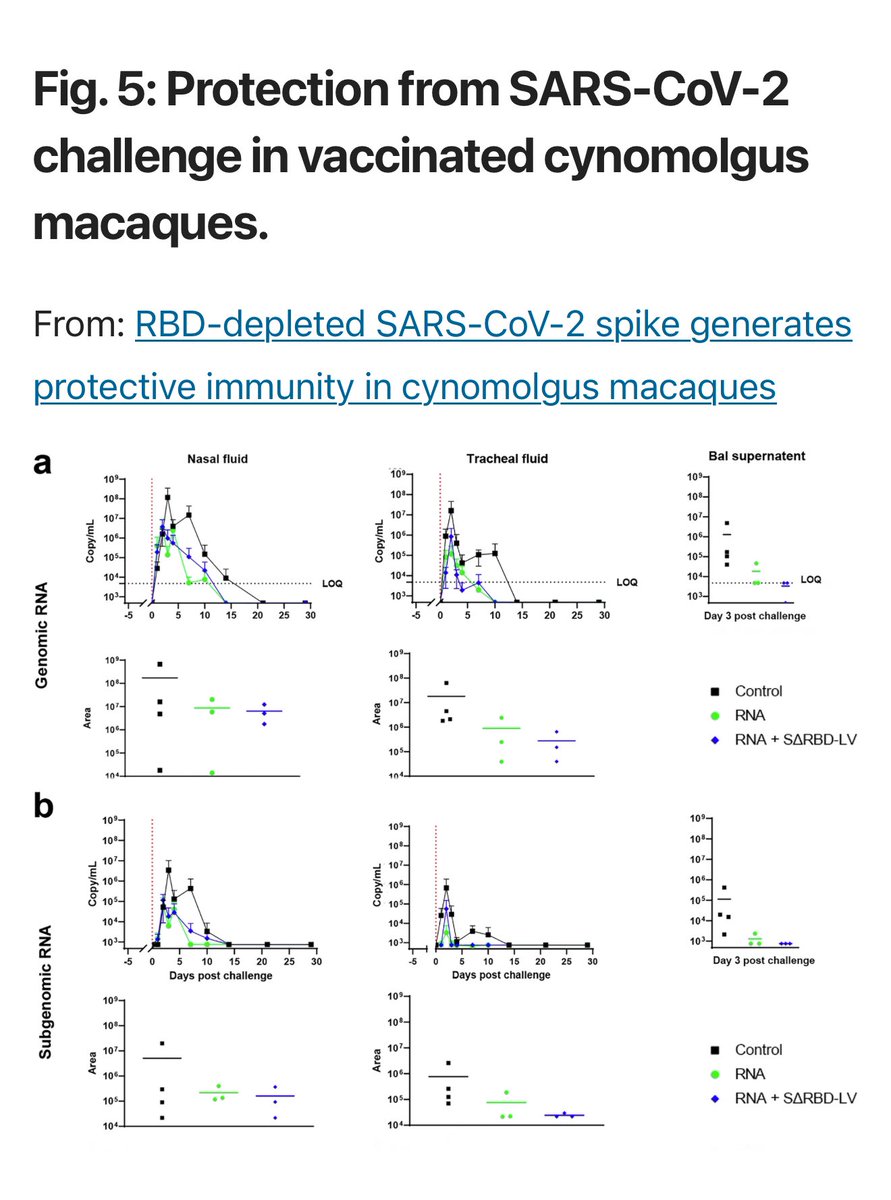
The SΔRBD-LV boost indicated better protection against lung infection than the Pfizer-BioNTech mRNA vaccine strategy alone. 5/ 
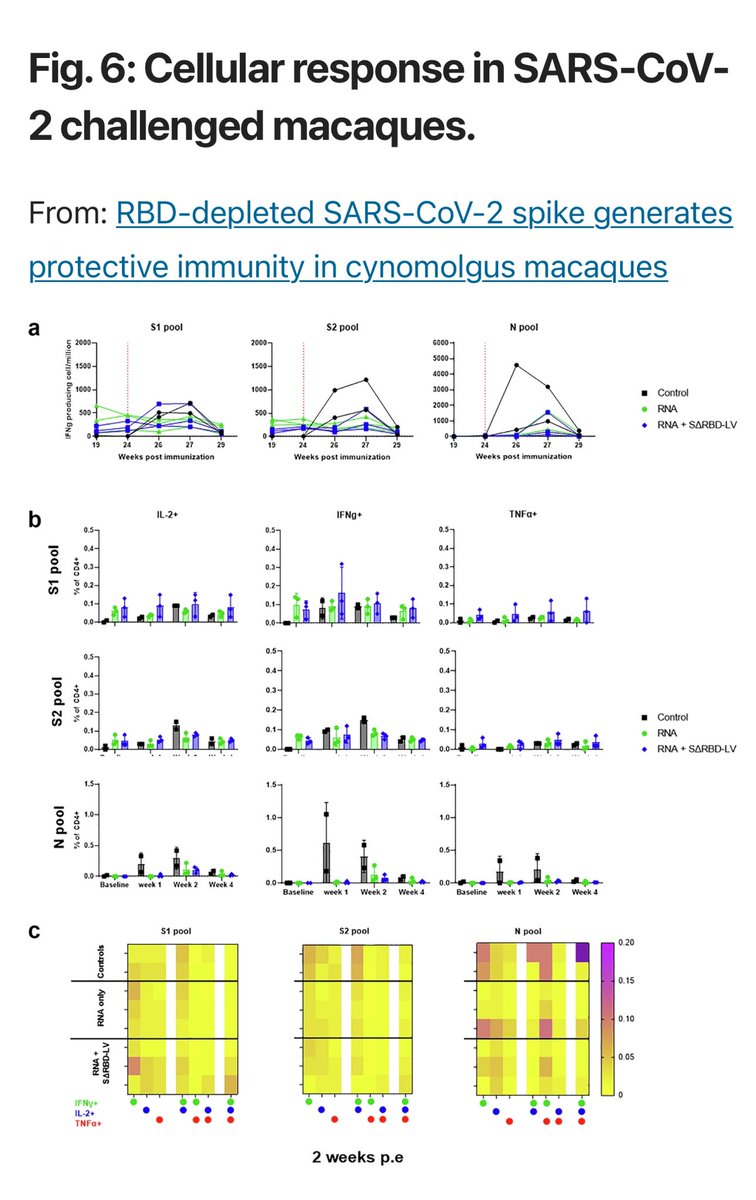
This, SΔRBD is highly immunogenic and provides improved protection compared to a third mRNA boost indicative of superior antibody-based protection. 6/ 
The study suggesting that vaccines targeting more stable regions of the virus may offer broader, longer-lasting protection. 7/7
nature.com/articles/s4154…
nature.com/articles/s4154…
• • •
Missing some Tweet in this thread? You can try to
force a refresh