Up to 60% of individuals with schizophrenia experience persistent negative symptoms (Correll C & Schooler N et al., 2020).
These symptoms contribute more to functional impairment than positive symptoms and are often under-recognised in clinical settings.
Let’s explore the neurobiology, diagnostic challenges, and treatment strategies that guide clinician care in managing negative symptoms. 🧵👇
These symptoms contribute more to functional impairment than positive symptoms and are often under-recognised in clinical settings.
Let’s explore the neurobiology, diagnostic challenges, and treatment strategies that guide clinician care in managing negative symptoms. 🧵👇

Defining Negative Symptoms
Negative symptoms represent deficits in normal functioning and are classified into:
• Avolition
• Anhedonia
• Asociality
• Alogia
• Blunted affect
They are distinct from depression or cognitive impairment and require targeted assessment.
Negative symptoms represent deficits in normal functioning and are classified into:
• Avolition
• Anhedonia
• Asociality
• Alogia
• Blunted affect
They are distinct from depression or cognitive impairment and require targeted assessment.
Clinical Burden and Long-Term Impact
Negative symptoms predict poorer outcomes in social, occupational, and cognitive domains.
They are less responsive to standard antipsychotics and more likely to persist throughout the illness.
Avolition, in particular, is the strongest predictor of real-world disability.
Negative symptoms predict poorer outcomes in social, occupational, and cognitive domains.
They are less responsive to standard antipsychotics and more likely to persist throughout the illness.
Avolition, in particular, is the strongest predictor of real-world disability.
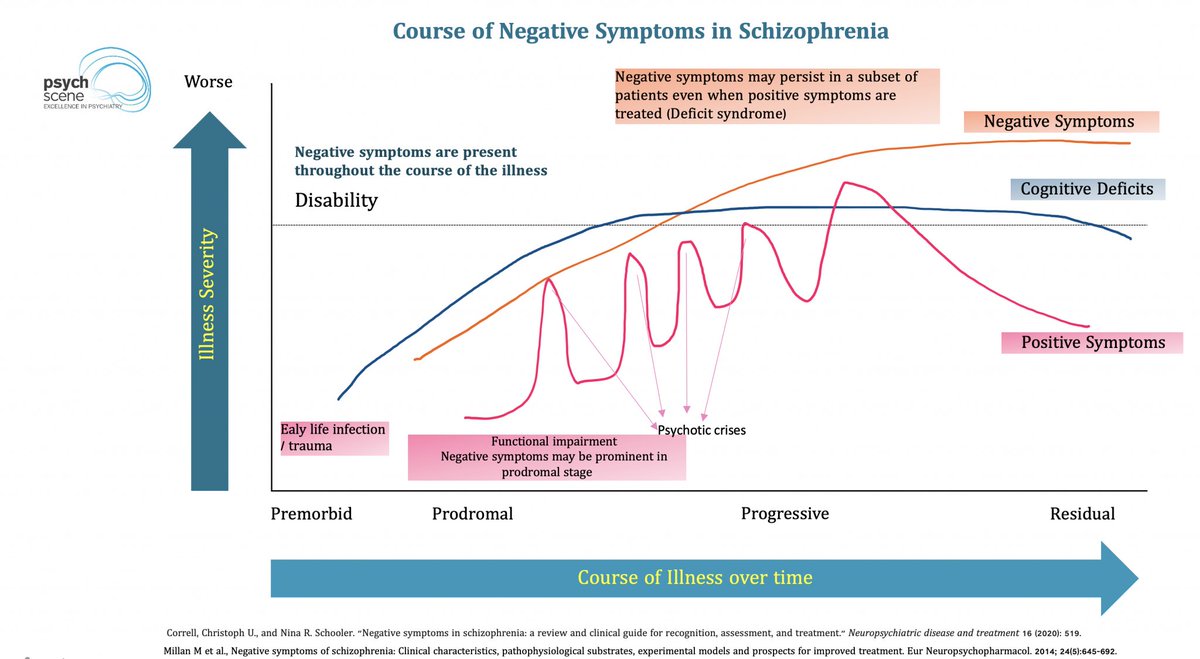
Symptom Trajectory and Persistence
Negative symptoms often emerge early and persist beyond the resolution of positive symptoms.
Their course is typically chronic and poorly responsive without specific intervention.
Negative symptoms often emerge early and persist beyond the resolution of positive symptoms.
Their course is typically chronic and poorly responsive without specific intervention.
Neural Circuitry Involved
Disrupted fronto-striatal pathways underlie the core features of negative symptoms.
Key circuits include:
• DLPFC to dorsal striatum – goal-directed behaviour
• ACC to ventral striatum – cost–effort estimation
• OFC to limbic regions – reward valuation
Disrupted fronto-striatal pathways underlie the core features of negative symptoms.
Key circuits include:
• DLPFC to dorsal striatum – goal-directed behaviour
• ACC to ventral striatum – cost–effort estimation
• OFC to limbic regions – reward valuation
Glutamate and NMDA Receptor Dysfunction
Hypofunction of NMDA receptors leads to impaired GABAergic inhibition and disrupted excitatory–inhibitory balance.
This contributes to cortical–subcortical disconnection, which underpins blunted motivation and hedonic tone.
Hypofunction of NMDA receptors leads to impaired GABAergic inhibition and disrupted excitatory–inhibitory balance.
This contributes to cortical–subcortical disconnection, which underpins blunted motivation and hedonic tone.
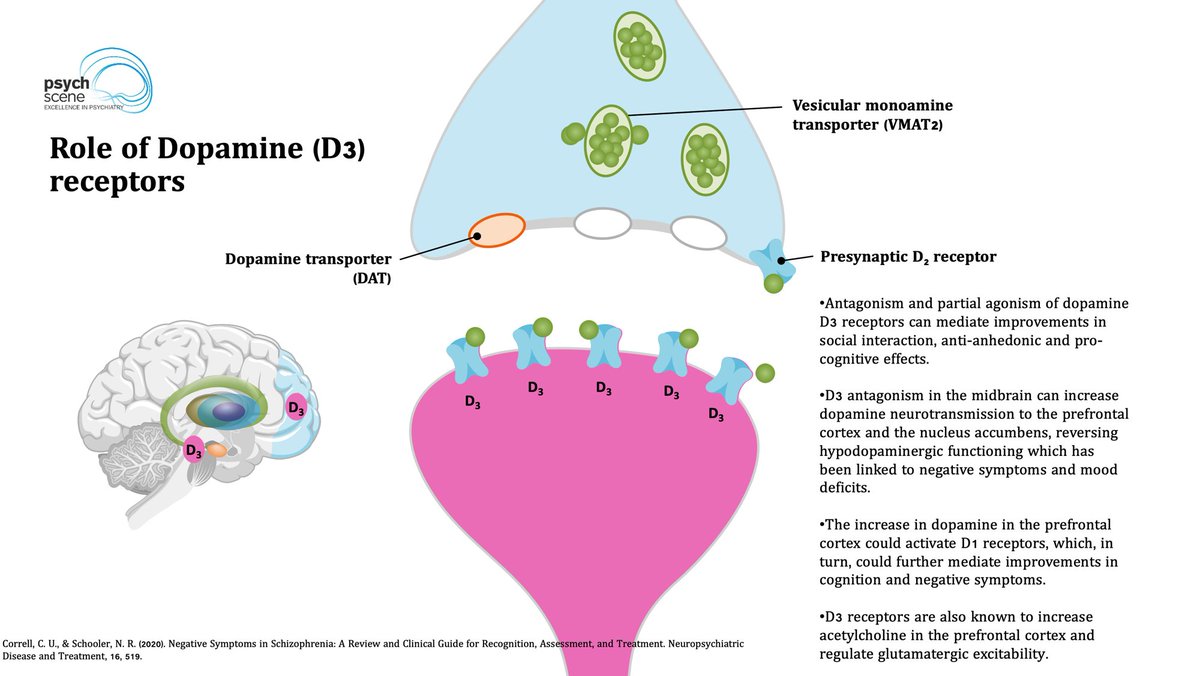
Dopamine D3 Receptors in Motivation and Reward
D3 receptors are densely expressed in the mesolimbic system and modulate mood, cognition, and social behaviour.
Agents with D3 activity (e.g. cariprazine) have shown benefit in targeting primary negative symptoms.
D3 receptors are densely expressed in the mesolimbic system and modulate mood, cognition, and social behaviour.
Agents with D3 activity (e.g. cariprazine) have shown benefit in targeting primary negative symptoms.
Primary vs Secondary Negative Symptoms
Primary symptoms are intrinsic to the illness.
Secondary symptoms may result from:
• Positive symptoms
• Extrapyramidal side effects
• Depression
• Environmental deprivation
Distinguishing between them is essential for accurate treatment planning.
Primary symptoms are intrinsic to the illness.
Secondary symptoms may result from:
• Positive symptoms
• Extrapyramidal side effects
• Depression
• Environmental deprivation
Distinguishing between them is essential for accurate treatment planning.
Assessment Strategies
Validated scales include:
• Brief Negative Symptom Scale (BNSS)
• Clinical Assessment Interview for Negative Symptoms (CAINS)
• NSA-16 or PANSS Negative Subscale
Structured assessments are critical for evaluating treatment response and clinical trials.
Validated scales include:
• Brief Negative Symptom Scale (BNSS)
• Clinical Assessment Interview for Negative Symptoms (CAINS)
• NSA-16 or PANSS Negative Subscale
Structured assessments are critical for evaluating treatment response and clinical trials.
Pharmacological Interventions
• Cariprazine: partial D3/D2 agonist with robust evidence from RCTs
• Amisulpride (low dose): efficacy in treating primary negative symptoms
• Adjuncts: N-acetylcysteine, modafinil, minocycline in selected cases
• Neuromodulation: rTMS and tDCS targeting DLPFC show emerging benefit
• Cariprazine: partial D3/D2 agonist with robust evidence from RCTs
• Amisulpride (low dose): efficacy in treating primary negative symptoms
• Adjuncts: N-acetylcysteine, modafinil, minocycline in selected cases
• Neuromodulation: rTMS and tDCS targeting DLPFC show emerging benefit
Avolition as a Central Node
Network models identify avolition as the most interconnected and impairing negative symptom.
Targeting motivation and behavioural activation may offer the greatest real-world benefit.
Network models identify avolition as the most interconnected and impairing negative symptom.
Targeting motivation and behavioural activation may offer the greatest real-world benefit.
Summary
Negative symptoms are central to the functional disability associated with schizophrenia.
They require active screening, structured measurement, and combined treatment strategies tailored to symptom type and severity.
Negative symptoms are central to the functional disability associated with schizophrenia.
They require active screening, structured measurement, and combined treatment strategies tailored to symptom type and severity.
Want to learn more about the neurobiology, clinical assessment, and management of negative symptoms in schizophrenia?
Read the full article, “Negative Symptoms in Schizophrenia – A Review of Neurobiology, Diagnosis and Management,” on The Psych Scene Hub:
psychscene.co/4mt7tWY
Read the full article, “Negative Symptoms in Schizophrenia – A Review of Neurobiology, Diagnosis and Management,” on The Psych Scene Hub:
psychscene.co/4mt7tWY
• • •
Missing some Tweet in this thread? You can try to
force a refresh